Abstract
Background
Consumer-directed health plans are increasingly common, yet little is known about their impact on physician decision-making and preventive service use.
Objective
To determine how patients’ deductible levels and socioeconomic status may affect primary care physicians’ recommendations for colorectal cancer screening.
Design, Setting, and Participants
Screening recommendations were elicited using hypothetical vignettes from a national sample of 1,500 primary care physicians. Physicians were randomized to one of four vignettes describing a patient with either low or high socioeconomic status (SES) and either low- or high-deductible plan. Bivariate and multivariate analyses were used to examine how recommendations varied as a function of SES and deductible.
Outcome Measures
Rates of recommendation for home fecal occult blood testing, sigmoidoscopy, colonoscopy, and inappropriate screening, defined as no screening or office-based fecal occult blood testing.
Results
A total of 528 (49%) eligible physicians responded. Overall, 7.2% of physicians recommended inappropriate screening; 3.2% of patients with high SES in low-deductible plans received inappropriate screening recommendations and 11.4% of patients with low SES in high-deductible plans for an adjusted odds ratio of 0.22 (0.05–0.89). The odds of a colonoscopy recommendation were over ten times higher (AOR 11.46, 5.26–24.94) for patients with high SES in low-deductible plans compared to patients with low SES in high-deductible plans. Funds in medical savings accounts eliminated differences in inappropriate screening recommendations.
Conclusions
Patient SES and deductible-level affect physician recommendations for preventive care. Coverage of preventive services and funds in medical savings accounts may help to mitigate the impact of high-deductibles and SES on inappropriate recommendations.
KEY WORDS: consumer-directed health plans, patient socioeconomic status, physician decision-making, colorectal cancer screening
INTRODUCTION
Consumer-directed health plans represent a market-based strategy designed to curb the steep rise in health-care spending.1–3 Enrollment in consumer-directed health plans (CDHPs), which combine high-deductible insurance products with medical savings accounts, has grown to 6.1 million Americans in 2008.4 Despite this rising enrollment, little evidence exists on how CDHPs affect physicians’ treatment recommendations and quality of care.
In theory, consumer-directed plans aim to reduce patients’ use of medical services, particularly those that are unnecessary or of lesser value. However, early research indicates that patients may decrease their use of both necessary and unnecessary care.5–7 In the case of preventive services, two large claims-based studies reveal that cancer screening rates are unchanged when they are exempt from the deductible.8,9 Yet 16% of purchased CDHP policies do not exempt any preventive services from the deductible; exemptions do not apply to all services, and over 40% of plans do not exempt more than $500 of services.10 CDHP enrollees may use medical savings accounts to pay for preventive care, but 50% of firms in 2007 did not make contributions to their employees’ accounts.11 In this environment, what will become of patients’ preventive service utilization?
Some CDHPs offer information technology to help patients weigh the costs and benefits of specific services, but such decision-support tools continue to be underutilized and underdeveloped.12,13 Therefore, patients enrolled in CDHPs may rely on their physicians for guidance in deciding which care to pursue. In this study, we explore how physicians will consider cost, coverage, and ability to pay in making recommendations for colorectal cancer screening.
Rates of screening for colorectal cancer are lower than those for breast and cervical cancer despite effective testing options of varying cost and frequency.14,15 Rates among low-income patients remain significantly lower than among high-income patients16–18 and use of inappropriate screening modalities is still prevalent.19–21 Physicians’ recommendations are a crucial motivator for patients to undergo colorectal cancer screening,22–24 yet many non-clinical factors, like lack of time and forgetfulness, determine whether such advice is given.25 By using a clinical vignette, we examine whether primary care physicians’ screening recommendations differ for a hypothetical patient with varied socioeconomic status and insurance coverage. Specifically, we test whether enrollment in a high-deductible insurance plan without exemptions for preventive care leads to higher rates of inappropriate screening recommendations and lower rates of colonoscopy, especially for individuals with low socioeconomic status. We further examine whether funds in medical savings accounts affect screening choice.
METHODS
Study Design and Population
We mailed an anonymous survey in May and June of 2007 to a nationally representative sample of 1,500 US primary care physicians randomly selected from the American Medical Association Masterfile. Eligible physicians were primary care providers aged 65 and younger. Each physician received a $2 incentive in the first mailing. Non-responders were sent two additional mailings without a financial incentive. Phone calls and internet searches were employed to determine whether non-respondents practiced primary care medicine and had an accurate mailing address.
Survey Design
The survey instrument was developed after a review of the literature and was test piloted among approximately 50 academic and community-based primary care physicians with the use of cognitive interviewing. The Institutional Review Board of the University of Pennsylvania approved this study.
The survey instrument included a clinical vignette and a questionnaire about attitudes related to CDHPs. This study focuses on results from the clinical vignette. The vignette asked physicians to make a colorectal cancer screening recommendation for a healthy 50-year-old male (Appendix Box 1). There were four versions of the vignette, which varied by (1) patient’s socio-economic status (SES) and (2) insurance coverage for the screening test. Socio-economic status was defined as either low (indicated by the patient being “a cashier at a convenience store”) or high (indicated by the patient being “an executive at a brokerage firm”). Insurance coverage was defined as either a low-deductible copayment-based plan (indicated by a “$10 co-payment for any screening test”) or a high-deductible plan (indicated by “need to pay the full price of colon cancer screening”). This provided a two-by-two design (low SES/high deductible, high SES/high deductible, low SES/low deductible, high SES/low deductible), representing different levels of financial barriers to care. Physicians were randomized to receive one version of the vignette.
Vignettes included test prices based on the published literature26 (office FOBT $10, home FOBT $40, flexible sigmoidoscopy $300, and colonoscopy $1,000). Screening options included: no screening, office-based fecal occult blood test (FOBT), home-based FOBT, flexible sigmoidoscopy, flexible sigmoidoscopy plus FOBT, and colonoscopy. In the high-deductible versions, we included a follow-up question to assess the impact of a medical savings account. It asked physicians to make a screening recommendation for the same patient if his employer put $700 in a medical savings account that could be used now or saved from year to year. The $700 approximates the average employer contribution to an individual’s medical savings account in 2006.27 Each vignette closed with a series of questions exploring the importance (5-point scale) of various patient and test characteristics in making a screening recommendation.
Statistical Analysis
Screening recommendations were divided into four categories for analysis: (1) inappropriate recommendations, defined as office-based fecal occult blood testing or no screening;28,29 (2) home FOBT; (3) sigmoidoscopy with or without FOBT; (4) colonoscopy. Physicians’ responses on a 5-point scale about the importance of patient and test characteristics in making screening recommendations were dichotomized as either important (“important” or “very important”) or unimportant (“very unimportant,” “unimportant,” or “neutral”).
The study was powered at the 0.8 level (alpha 0.05) to detect a 10% absolute difference between screening recommendations given to low and high SES patients in a high-deductible plan. Physicians were randomized to high-deductible vignettes at a 2 to 1 ratio compared to low-deductible vignettes. We anticipated that the results from the two low-deductible vignettes would be pooled for analysis.
Response weights, based on physician characteristics, were used to adjust for non-response bias. Weighted results are presented. Descriptive statistics and chi-square tests were employed to compare the proportions of physicians choosing different screening modalities. Multivariable logistic regression was used to adjust for the effects of physician demographic and practice factors on choice of screening. Physician factors included age, gender, primary care specialty, board certification, medical degree, and country of medical school graduation; practice factors included academic affiliation, percentage of patients in practice covered by Medicaid, and region of the US. We compared recommendations between the four vignette versions, using low SES/high deductible as the reference group as this represented the patient with the greatest financial barriers to care. Then, we compared recommendations within SES and deductible strata. All analyses were performed using Stata 9.0.
RESULTS
After excluding doctors who did not practice primary care (124) and those with inaccurate mailing addresses (300), the adjusted response rate was 49% (528/1,076). Respondents were more likely than non-respondents to be female (29% vs. 25%, p = 0.04), US medical graduates (83% vs. 70%, p < 0.001), board certified (84% vs. 75%, p = 0.02), and family physicians/general practitioners (54% vs. 44%, p = 0.002). There were no significant differences between respondents and non-respondents with regard to age, medical degree, or region.
Table 1 provides demographic and practice characteristics on the 528 respondents. Randomization across the four vignettes was achieved with no significant differences between respondents based on demographic or practice characteristics.
Table 1.
Characteristics of Primary Care Physicians and their Practice Settings
| Total sample no. (%) | |
|---|---|
| Total | 528 (100) |
| Age | |
| ≤45 | 187 (35.5) |
| 46–55 | 214 (40.6) |
| 56–65 | 126 (23.9) |
| Gender | |
| Male | 354 (70.9) |
| Female | 153 (29.0) |
| Specialty | |
| Internal medicine | 244 (46.3) |
| Family medicine/general practice | 283 (53.7) |
| Board certification | |
| Yes | 442 (83.7) |
| No | 86 (16.2) |
| Degree | |
| MD | 466 (88.3) |
| DO | 62 (11.7) |
| US medical graduate | |
| Yes | 436 (82.7) |
| No | 92 (17.3) |
| Academic affiliation | |
| Yes | 179 (34.4) |
| No | 341 (65.6) |
| % Medicaid patients in practice | |
| ≥20% | 111 (21.9) |
| <20% | 393 (78.1) |
| Region | |
| Northeast | 112 (21.2) |
| South | 166 (31.5) |
| Midwest | 145 (27.4) |
| West | 105 (19.9) |
| Vignette | |
| High SES/low deductible | 84 (16.0) |
| Low SES/low deductible | 91 (17.3) |
| High SES/high deductible | 172 (32.7) |
| Low SES/high deductible | 180 (34.0) |
Screening Recommendations by Vignette
Rates of inappropriate screening, home FOBT, sigmoidoscopy, and colonoscopy varied among the four vignettes (Fig. 1). Overall, 7.2% of physicians made inappropriate colon cancer screening recommendations. High SES patients with low-deductible plans received inappropriate screening recommendations 3.2% of the time; low SES patients with a high-deductible plan received inappropriate screening recommendations 11.4% of the time, resulting in an adjusted odds ratio of 0.22 (0.05–0.89) (Table 2).
Figure 1.
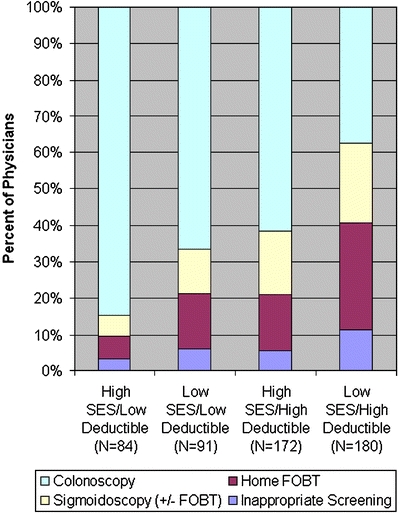
Distribution of colorectal cancer screening recommendations by vignette.
Table 2.
Physician Recommendations for Colorectal Cancer Screening by Deductible and Patient SES
| % of physicians (n = 528) | Adjusted OR* (95% CI) | P value | |
|---|---|---|---|
| Inappropriate screening | |||
| High SES/low deductible | 3.2 | 0.22 (0.05–0.89) | 0.03 |
| Low SES/low deductible | 5.9 | 0.53 (0.20–1.39) | 0.17 |
| High SES/high deductible | 5.4 | 0.42 (0.19–0.97) | 0.04 |
| Low SES/high deductible | 11.4 | 1 | |
| Home FOBT | |||
| High SES/low deductible | 6.6 | 0.15 (0.06–0.42) | <0.001 |
| Low SES/low deductible | 15.5 | 0.41 (0.20–0.81) | 0.01 |
| High SES/high deductible | 15.8 | 0.40 (0.23–0.69) | 0.001 |
| Low SES/high deductible | 29.3 | 1 | |
| Sigmoidoscopy | |||
| High SES/low deductible | 5.6 | 0.18 (0.06–0.61) | 0.006 |
| Low SES/low deductible | 12.0 | 0.43 (0.20–0.94) | 0.03 |
| High SES/high deductible | 17.4 | 0.66 (0.37–1.17) | 0.15 |
| Low SES/high deductible | 21.8 | 1 | |
| Colonoscopy | |||
| High SES/low deductible | 84.6 | 11.46 (5.26–24.94) | <0.001 |
| Low SES/low deductible | 66.6 | 3.91 (2.17–7.04) | <0.001 |
| High SES/high deductible | 61.5 | 3.32 (2.07–5.31) | <0.001 |
| Low SES/high deductible | 37.6 | 1 | |
OR, odds ratio; CI, confidence interval
*Adjusted for age, gender, board certification, specialty, medical degree type, country of medical school graduation, academic affiliation of practice, proportion of practice covered by Medicaid, region of the country
Compared to low SES/high deductible patients, all others—whether of high SES, low deductible, or both—were less likely to be recommended home FOBT and more likely to be recommended colonoscopy. Physicians recommended colonoscopy 84.6% of the time to high SES/low deductible patients and 37.6% of the time to low SES/high deductible patients (AOR 11.46, 5.26–24.94). Additional comparisons of screening recommendations between the different vignettes are made in subsequent sections. A test to determine whether SES modified the association between deductible level and screening recommendation was not significant for any of the four screening categories.
When making their recommendations, over 90% of physicians in each vignette category identified screening guidelines and test effectiveness as important or very important (Table 3). The extent to which patient income, patient insurance coverage, test cost, and test frequency factored into physicians’ recommendations varied by vignette.
Table 3.
Percent of Physicians who said that the following Test and Patient Factors were Important or very important when making their Screening Recommendation
| High SES/low deductible, % | Low SES/low deductible, % | High SES/high deductible, % | Low SES/high deductible, % | |
|---|---|---|---|---|
| Screening guidelines | 98 | 92 | 92 | 90 |
| Effectiveness of test | 96 | 92 | 95 | 92 |
| Cost of the test | 49* | 61* | 59* | 74* |
| Income of patient | 34* | 33* | 48* | 69* |
| Insurance of patient | 59* | 53* | 45* | 64* |
| Convenience of test | 51 | 48 | 47 | 41 |
| Frequency of test | 79* | 62* | 58* | 55* |
*Significant intervignette differences (chi-squared test P < 0.05)
Screening Recommendations Within Deductible Strata
The above results describe the odds ratios of recommending different colorectal cancer screening modalities based on both patients’ SES and deductible. However, we were also interested in comparing recommendations for patients of different SES within high-deductible and low-deductible plans. The results of these analyses are shown in Table 4. Within high deductible plans, patients with high SES were significantly less likely to receive recommendations for inappropriate screening (AOR 0.41, 0.18–0.93) and home FOBT (AOR 0.39, 0.22–0.69) and more likely to receive recommendations for colonoscopy (AOR 3.44, 2.11–5.61) compared to patients with low SES. Within low-deductible plans where patients pay $10 for any screening test, patients with high SES were significantly more likely to receive recommendations for colonoscopy (AOR 3.33, 1.42–7.80) than patients with low SES.
Table 4.
Physician Recommendations for Preventive Colorectal Cancer Screening within Deductible Strata by Patient SES
| SES | ||||||
| High-deductible plan | High (n = 185) | Low (n = 178) | % Diff | P value* | Adjusted OR† (95% CI) | P value |
| Inappropriate screening | 5.4% | 11.4 | −6.0 | 0.04 | 0.41 (0.18–0.93) | 0.03 |
| FOBT | 15.8 | 29.3 | −13.5 | 0.002 | 0.39 (0.22–0.69) | 0.001 |
| Sigmoidoscopy | 17.4 | 21.8 | −4.4 | 0.50 | 0.67 (0.37–1.21) | 0.19 |
| Colonoscopy | 61.5 | 37.6 | 23.9 | <0.001 | 3.44 (2.11–5.61) | <0.001 |
| SES | ||||||
| Low-deductible plan | High (n = 97) | Low (n = 68) | ||||
| Inappropriate screening | 3.2% | 5.9 | −2.7 | 0.45 | 0.22 (0.04–1.24) | 0.09 |
| FOBT | 6.6 | 15.5 | −8.9 | 0.15 | 0.35 (0.10–1.21) | 0.10 |
| Sigmoidoscopy | 5.6 | 12.0 | −6.4 | 0.28 | 0.49 (0.15–1.67) | 0.31 |
| Colonoscopy | 84.6 | 66.6 | 18.0 | 0.02 | 3.33 (1.42–7.80) | 0.006 |
OR, odds ratio; CI, confidence interval
*Fisher’s exact test
†Adjusted for age, gender, board certification, specialty, medical degree type, country of medical school graduation, academic affiliation of practice, proportion of practice covered by Medicaid, region of the country
Screening Recommendations Within SES Strata
We next sought to compare screening recommendations for patients with the same SES but different deductible levels. Among patients with low SES, rates of inappropriate screening were not significantly different among plan types. However, patients with low SES in low-deductible plans were significantly less likely to be recommended home FOBT (AOR 0.43, 0.21–0.86) and sigmoidoscopy (AOR 0.41, 0.18–0.91) and more likely to be recommended colonoscopy (AOR 3.74, 2.08–6.72) than those in high-deductible plans. Among patients with high SES, those in low-deductible plans were significantly more likely to be recommended colonoscopy (AOR 3.33, 1.42–7.80) than those in high-deductible plans. Rates of recommendations for inappropriate and FOBT screening did not differ significantly.
Effects of a Medical Savings Account
For physicians who received the high-deductible versions of the vignette, a follow-up question asked whether $700 in the patient’s medical savings account would affect their recommendation. Bivariate and multivariate analyses demonstrated that low SES/high deductible patients with $700 in a medical savings account no longer received recommendations for inappropriate screening at a higher rate than other patients.
Differences in colonoscopy recommendations remained between the vignettes. High SES/low deductible patients were significantly more likely to be recommended colonoscopy than low SES/high deductible patients (84.6% vs. 56.9%; AOR 4.40, 2.09–9.27) and than high SES/high deductible patients (84.6% vs. 68.8%; AOR 2.61, 1.19–5.74). Within high-deductible plans, patients with high SES remained more likely to be recommended colonoscopy than patients with low SES (68.8% vs. 56.9%; AOR 1.97, 1.22–3.18).
DISCUSSION
This study examines how patient SES and high-deductible insurance without exemptions for preventive services may alter the quality of colorectal cancer screening. We found that the odds of receiving inappropriate colorectal cancer screening recommendations were almost five times higher for patients with low SES in high-deductible coverage than for patients with high SES in traditional low-deductible plans. Available funds in a medical savings account seemed to limit this advice for inappropriate care. Recommendations for both home FOBT and colonoscopy were independently associated with patient SES and deductible levels. This study raises many issues with regard to how physicians will advise consumers faced with high deductibles and varying abilities to pay for care out-of-pocket.
To date, CDHPs have preferentially attracted people with higher incomes and fewer financial constraints,12,30 but the implications for patients with low SES must be understood as the individual and small group markets grow,31 as more small employers offer only CDHPs to their employees, and as Medicaid experiments with greater consumerism.32 Accordingly, primary care doctors are increasingly caring for patients enrolled in these plans; 41% currently care for patients with CDHPs and 43% report low knowledge of these plans.33
Our finding that more than one in ten physicians would recommend inappropriate screening to a low SES patient with high-deductible coverage is concerning. Advice for office-based FOBT is already too common19–21 and may become even more prevalent under CDHPs. Physicians confronted with patients with low SES and high-deductible coverage revealed that cost, coverage, and income considerations were more important to them than for those doctors advising a patient with fewer financial barriers. While consideration of ability to pay is essential in acting as a successful patient agent in CDHPs,34 it may lead to troubling trade-offs between cost and quality as demonstrated here. Some may argue that a $30 incremental increase in cost ($40 for home FOBT minus $10 for office FOBT) may be prohibitive for a patient with limited means and that some screening is better than none, but such an implication merits policy debate.
The implications are less clear with regard to differential rates of recommendation among appropriate screening modalities. Is there a right choice when deciding between home FOBT, sigmoidoscopy, and colonoscopy? All tests are considered to be effective and cost-effective based on widely accepted criteria,35 and choice among them is often a function of availability, provider practice style, and patient preference. In our study, recommendations for colonoscopy increased as financial barriers to use decreased. On the surface, this makes sense and seems reasonable as patients with low SES and high-deductible coverage may not be able to afford a $1,000 test. Yet an 11-fold difference in the odds of colonoscopy recommendation for such a patient (compared to a high SES patient in a low-deductible plan) raises concerns about the equitable distribution of medical resources.
As demonstrated by our findings, medical savings accounts may be important tools in mitigating disparities in inappropriate screening recommendations. Differences in colonoscopy recommendations, though, may persist. In practice, many patients may not have money in their savings accounts: approximately 50% of employees do not receive account contributions from their employers,11 and low income patients gain minimal to no tax advantages via these accounts, making personal contributions unlikely.36
Surprisingly, among patients who were required to pay only a $10 copayment for each of the screening tests, differences by patient SES were found. Ten-dollar copayments led to significantly lower rates of colonoscopy for patients with low SES. The ways that physicians incorporate patient SES into their decision-making remains poorly understood.37,38 Our data reveal that physicians’ recommendations for care mirror current SES disparities in actual colorectal cancer screening.
We also did not expect lower rates of colonoscopy recommendations for high SES patients with high-deductible coverage as compared to those with low-deductible coverage and a $10 copayment. Though possible, it seems unlikely that physicians were afraid that the patient with high SES would be unable to afford the cost of the colonoscopy. Rather, the variation may reflect the different mental accounting and cost-benefit calculations that physicians may perform when the test is paid for by the insurance company versus the individual patient.
There are several limitations to our study. First, with any survey non-response bias is a concern. Weighted analyses were employed. Randomization achieved balance between physician respondents to each of the vignettes. Second, the study was initially powered to combine the results of low and high SES patients enrolled in low-deductible health plans. We were unable to combine these results because responses to these vignettes were significantly different from one another, thus decreasing the power of certain inter-group comparisons. Third, social desirability bias may have influenced physicians to recommend colonoscopy over other tests. Fourth, in this study hypothetical patients were randomly assigned to physicians, whereas in reality patients of differening SES are often distributed in a non-random manner among providers. Fifth, this study was the first item of a larger survey of consumer-directed health plans that may lead to conditioning effects. Sixth, the vignettes were not meant to reflect high-deductible health plans with first-dollar coverage of preventive services. Such first-dollar coverage has become more common11 as policy experts have been calling for exemptions for high-value services.39,40
Lastly, our vignettes made key assumptions about physician recommendations for care and clinical decision-making within CDHPs. The patient in our scenario handed over his agency to the physician.34 While not uncommon in traditional plans, deferring to the primary care physician may become more common when patients are faced with difficult clinical decisions pitting cost against quality. Physicians who received our vignette knew the patient’s SES and insurance coverage and the price of various screening modalities. Arguably, primary care physicians have a sense of their patients’ SES via their employment status, a key component of the social history. Many physicians may not currently be aware of patients’ insurance type, but CDHPs may change this dynamic. By design, high deductibles and savings accounts aim to make patients more aware of their coverage. Faced with financial skin in the game, patients may signal to physicians accordingly about their plan specifics. Price information, too, may be provided to a physician by a primed consumer. Not only is such information becoming increasingly available through insurers offering CDHPs41–43, but also over 70% of physicians currently feel ready to advise patients regarding the cost of medical care.33 Although recent research suggests that physicians do not consider out-of-pocket costs owing to discomfort, lack of time, and a perceived inability to intervene,44–47 CDHPs enrollees may compel physicians to reconsider these issues. Therefore, our findings may not reflect actual decision-making within CDHPs, but they highlight crucial issues that must be explored further.
As more patients enroll in insurance plans with high deductibles and medical savings accounts, it is vital to understand how these plans affect physician decision-making, patient preferences, and the doctor-patient relationship. When preventive screening is not exempted from the deductible, patients in high-deductible plans may be less likely to receive recommendations for colonoscopy. Furthermore, patients with low socioeconomic status in high-deductible plans may be more likely to receive recommendations for inappropriate screening. This subset of patients seems most vulnerable to poor quality of care in a consumer-driven environment. Despite recent progress in CDHP benefit design, employer contributions to medical savings accounts and exemptions from the deductible for preventive care should be ensured.
Acknowledgements
The authors wish to thank the following individuals for their helpful suggestions and advice: David Asch M.D., Judy Shea Ph.D., Katrina Armstrong M.D., and Josh Metlay M.D. Ph.D. at the University of Pennsylvania and Caleb Alexander M.D. at the University of Chicago. No compensation was received for their contributions.
Funding for the study was provided by the Robert Wood Johnson Clinical Scholars Program at the University of Pennsylvania. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and the preparation, review or approval of the manuscript. Drs. Pollack and Mallya had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. This work has been presented at the annual meetings of the Robert Wood Johnson Clinical Scholars Program (Fort Lauderdale, November 2007) and the North American Primary Care Research Group (Vancouver, October 2007)
Funding for the study was provided by the Robert Wood Johnson Clinical Scholars Program at the University of Pennsylvania.
Conflict of Interest Dr. Polsky is spending the 2007–2008 academic year as a Senior Economist at the President’s Council of Economic Advisors. The authors report no other conflicts of interest.
Appendix Box 1. Sample vignette
| Mr. Jones, a 50-year-old male, presents for a new patient appointment. He has no significant personal or family medical history and no complaints today. His physical exam is within normal limits including his blood pressure and body mass index. You discuss dietary and physical activity goals with Mr. Jones and then bring up colon cancer screening. |
| Mr. Jones works as a cashier at a convenience store [an executive at a brokerage firm]. Under his health plan, he will need to pay the full price of colon cancer screening [a $10 co-payment for any screening test]. For reference, the prices of the tests are as follows: |
| •OFFICE FECAL OCCULT BLOOD TESTING.....................$10 |
| (One FOBT card with single sample from digital rectal exam) |
| •HOME FECAL OCCULT BLOOD TESTING........................$40 |
| (Multiple FOBT cards with self-collected samples) |
| •FLEXIBLE SIGMOIDOSCOPY.......................................$300 |
| •COLONOSCOPY.......................................................$1000 |
| All of the above tests are available in your area. You review the screening options with Mr. Jones and ask him what test, if any, he would like to undergo. He says he will defer to your judgment. |
Footnotes
Craig Evan Pollack and Giridhar Mallya: The authors contributed equally to this publication.
References
- 1.Goodman JC. What is consumer-directed care? Health Aff. 2006;25:w540–w543. [DOI] [PubMed]
- 2.Miller T. Getting on the soapbox: views of an innovator in consumer-directed care. Health Aff. 2006;25:w549–w551. [DOI] [PubMed]
- 3.Bush GW. Executive order: promoting quality and efficient health care in federal government administered or sponsored health care programs. Available at: http://www.whitehouse.gov/news/releases/2006/08/20060822-2.html. Accessed June 6, 2008.
- 4.American Health Insurance Plans Center for Policy and Research. January 2008 Census Shows 6.1 Million People Covered by HSA/High-Deductible Health Plans. Washington D.C.: American Health Insurance Plans; 2008.
- 5.Wharam JF, Landon BE, Galbraith AA, et al. Emergency department use and subsequent hospitalizations among members of a high-deductible health plan. JAMA. 2007;297:1093–1102. [DOI] [PubMed]
- 6.Davis K, Doty MM, Ho A. How high is too high? Implications of high-deductible health plans. New York City: The Commonwealth Fund; 2005.
- 7.The Kaiser Family Foundation. National Survey of Enrollees in Consumer Directed Health Plans. Washington D.C.: The Henry J. Kaiser Foundation; 2006.
- 8.Rowe J, Brown-Stevenson T, Downey R, Newhouse J. The effect of consumer-directed health plans on the use of preventive and chronic illness services. Health Aff. 2008;27:113–120. [DOI] [PubMed]
- 9.Busch S, Barry C, Vegso S, Sindelar J, Cullen M. Effects of a cost-sharing plan on use of preventive services at one large employer. Health Aff. 2006;25:1529–1536. [DOI] [PubMed]
- 10.America’s Health Insurance Plans Center for Policy and Research. A Survey of Preventive Benefits in Health Savings Account (HSA) Plans, July 2007. Washington, D.C.: America’s Health Insurance Plans; 2007.
- 11.The Kaiser Family Foundation and Health Research and Education Trust. Employer Health Benefits 2007 Annual Survey. The Kaiser Family Foundation and HRET; 2007.
- 12.Buntin MB, Damberg C, Haviland A, et al. Consumer-directed health plans: early evidence about effects on cost and quality. Health Aff. 2006;25:w516w–530. [DOI] [PubMed]
- 13.Fronstin P, Collins S. Findings from the 2007 EBRI/Commonwealth Fund Consumerism in Health Survey. Washington D.C.: EBRI; 2008. [PubMed]
- 14.Swan J, Breen N, Coates R, Rimer B, Lee N. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97:1528–1540. [DOI] [PubMed]
- 15.Lemon S, Zapka J, Puleo E, Luckmann R, Chasan-Taber L. Colorectal cancer screening participation: comparisons with mammography and prostate-specific antigen screening. Am J Pub Health. 2001;91:1264–1272. [DOI] [PMC free article] [PubMed]
- 16.Ananthakrishnan A, Schellhase K, Sparapani R, Laud P, Neuner J. Disparities in colon cancer screening in the Medicare population. Arch Intern Med. 2007;167:258–264. [DOI] [PubMed]
- 17.Phillips K, Ladabaum S-YLU, Haas J, et al. Trends in colonoscopy for colorectal cancer screening. Med Care. 2007;45:160–167. [DOI] [PubMed]
- 18.Liang S-Y, Phillips KA, Nagamine M, Ladabaum U, Haas JS. Rates and predictors of colorectal cancer screening. Preventing Chronic Disease. 2006;3:1–13. [DOI] [PMC free article] [PubMed]
- 19.Sox H. Office-based testing for fecal occult blood: do only in case of emergency. Ann Intern Med. 2005;142:146–148. [DOI] [PubMed]
- 20.Nadel M, Shapiro J, Klabunde C, et al. A national survey of primary care physicians’ methods for screening for fecal occult blood. Ann Intern Med. 2005;142:86–94. [DOI] [PubMed]
- 21.Klabunde CN, Frame PS, Meadow A, Jones E, Nadel M, Vernon SW. A national survey of primary care physicians’ colorectal cancer screening recommendations and practices. Prev Med. 2003;36:352–362. [DOI] [PubMed]
- 22.Zapka J, Puleo E, Cickers-Lahti M, Luckmann R. Healthcare system factors and colorectal cancer screening. Am J Prev Med. 2002;23:28–35. [DOI] [PubMed]
- 23.Lewis S, Jensen N. Screening sigmoidoscopy: factors associated with utilization. J Gen Intern Med. 1996;11:542–544. [DOI] [PubMed]
- 24.Mandelson M, Curry S, Anderson L. Colorectal cancer screening participation by older women. Am J Prev Med. 2000;19:149–154. [DOI] [PubMed]
- 25.Guerra C, Schwartz J, Armstrong K, Brown J, Hughes-Halbert C, Shea J. Barriers of and facilitators to physician recommendations of colorectal cancer screening. J Gen Intern Med. 2007;22:1681–1688. [DOI] [PMC free article] [PubMed]
- 26.Taylor WC. A 71-yearl-old woman contemplating a screening colonoscopy. JAMA. 2006;295:1161–1167. [DOI] [PubMed]
- 27.Claxton G, Gabel JR, Gil I, et al. Health benefits in 2006: premium increases moderate, enrollment in consumer-directed health plans modest. Health Aff. 2006;25:w476–w485. [DOI] [PubMed]
- 28.Byers T, Levin B, Rothenberger D, Dodd G, Smith R. American Cancer Society Guidelines for Early Detection of Colorectal Polyps and Cancer: update 1997. CA-Cancer J Clin. 1997;47:154–160. [DOI] [PubMed]
- 29.United States Preventive Service Task Force. Screening for colorectal cancer: recommendation and rationale. Ann Intern Med. 2002;137:129–131. [DOI] [PubMed]
- 30.Parente S, Feldman R, Christianson J. Employee choice of consumer-driven health insurance in a multiplan, multiproduct setting. Health Serv Res. 2004;39:1091–1111. [DOI] [PMC free article] [PubMed]
- 31.America’s Health Insurance Plans Center for Policy and Research. January 2007 Census Shows 4.5 Million People Covered by HSA/High-Deductible Health Plans. Washington D.C.: America’s Health Insurance Plans; 2007.
- 32.Greene J. State Approaches to Consumer Direction in Medicaid. New Jersey: Center for Health Care Strategies, Inc.; 2007.
- 33.Mallya G, Pollack C, Polsky D. Are primary care physicians ready to practice in a consumer-driven environment? Am J Manag Care. Forthcoming, 2008. [PubMed]
- 34.Alexander GC, Hall MA, Lantos JD. Rethinking professional ethics in the cost-sharing era. Am J Bioethics. 2006;6:w17–w22. [DOI] [PubMed]
- 35.Pignone M. Cost-effectiveness analyses of colorectal cancer screening: a systematic review for the US preventive services task force. Ann Int Med. 2002;137:132–141. [DOI] [PubMed]
- 36.Glied SA, Remler DK. The Effect of Health Savings Accounts on Health Insurance Coverage. New York: The Commonwealth Fund; 2005. [PubMed]
- 37.Denberg TD, Kim FJ, Flanigan RC, et al. The influence of patient race and social vulnerability on urologist treatment recommendations in localized prostate carcinoma. Med Care. 2006;44:1137–1141. [DOI] [PubMed]
- 38.Bernheim S, Ross J, Krumholz H, Bradley E. Influence of patients’ socioeconomic status on clinical management decisions: a qualitative study. Ann Fam Med. 2008;6:53–59. [DOI] [PMC free article] [PubMed]
- 39.Brennan T, Reisman L. Value-based insurance design and the next generation of consumer-driven health care. Health Aff. 2007;26:w204–w207. [DOI] [PubMed]
- 40.Bloche MG. Consumer-directed health care and disadvantage. Health Aff. 2007;26:1315–1327. [DOI] [PubMed]
- 41.Rosenthal M, Hsuan C, Milstein A. A report card on the freshman class of consumer-directed health plans. Health Aff. 2005;24:1592–1600. [DOI] [PubMed]
- 42.Fuhrmans V. Insurer reveals what doctors really charge: to help people compare fees, Aetna posts some online; a potential bargaining tool. The Wall Street Journal. August 18, 2005.
- 43.Rubenstein S. Patients get new tools to price health care. The Wall Street Journal. June 13, 2006.
- 44.Pham HH, Alexander GC, O’Malley AS. Physician consideration of patients’ out-of-pocket costs in making common clinical decisions. Arch Intern Med. 2007;167:663–668. [DOI] [PubMed]
- 45.Alexander GC, Casalino LP, Meltzer DO. Patient-physician communication about out-of-pocket costs. JAMA. 2003;290:953–958. [DOI] [PubMed]
- 46.Alexander GC, Casalino LP, Meltzer DO. Physician strategies to reduce patients’ out-of-pocket prescription costs. Arch Intern Med. 2005;165:633–636. [DOI] [PubMed]
- 47.Alexander GC, Casalino LP, Tseng C-W, McFadden D, Meltzer DO. Barriers to patient-physician communication about out-of-pocket costs. J Gen Intern Med. 2004;19:856–860. [DOI] [PMC free article] [PubMed]


