To the Editor:
Total leukocyte count in the peripheral blood has been reported to be a significant predictor of future cardiac events and mortality.1 Leukocyte-derived salivary lysozyme has been associated with oral infection,2 and serum lysozyme has been implicated in impaired glucose metabolism,3 a contributory factor for endothelial dysfunction.4 We postulated that salivary lysozyme, therefore, would be associated with coronary heart disease (CHD).
This study was approved by the joint ethical committee of the Kuopio University Hospital and the University of Kuopio. We investigated the relationship between the CHD and lysozyme levels in a case-control study of 250 angiographically confirmed CHD patients and 250 sex- and age-matched controls, adjusting for age, sex, smoking, body mass index (BMI), diabetes mellitus, total cholesterol/high-density lipoprotein (HDL) cholesterol, hypertension, and serum C-reactive protein (CRP) levels ≥10 mg/L or ≥3 mg/L using logistic regression analyses. To assess the specific contribution of oral health through impaired glucose metabolism, we controlled for the Asymptotic Dental Score (ADS), an estimate of oral infection burden, comprising 5 major oral pathologies, namely pericoronitis, gingivitis, dental caries, root remnants, and the edentulous state.5
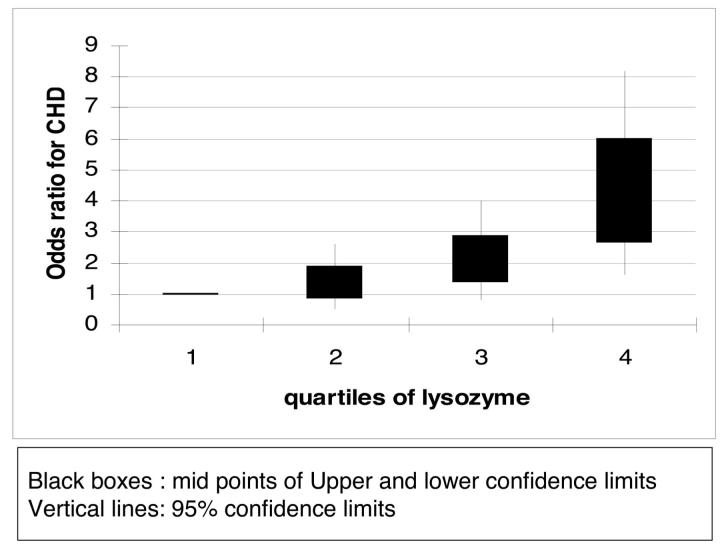
The basic characteristics of the cohort (Table I, available online at http://atvb.ahajournals.org) and cross-tabulation of lysozyme levels and other vascular risk factors are presented online (Table II, available online at http://atvb.ahajournals.org). After adjustment for established cardiac risk factors including age, sex, smoking, total cholesterol/HDL cholesterol, diabetes, hypertension, BMI, and CRP, odds ratios (ORs) with 95% CIs for the association between salivary lysozyme and CHD increased from 1.00 (the reference group) to 1.16 (0.51 to 2.63), 1.82 (0.83 to 4.01), and 3.62 (1.60 to 8.16) from the lowest to highest quartiles of salivary lysozyme (P value for linear trend <0.0001; Figure; Table III, available online at http://atvb. ahajournals.org). Models using log-transformed lysozyme or omitting the intermediate variables such as diabetes or hypertension generated similar results. When we adjusted for the ADS, the ORs (CI) decreased slightly to 1.00, 1.12 (0.48 to 2.62), 1.92 (0.85 to 4.34), and 3.45 (1.50 to7.93). When we adjusted for CRP using a threshold of 3 mg/L, the OR for the fourth quartile of lysozyme decreased to 2.73 (1.53 to 4.87) compared with the other 3 quartiles combined and the C-statistic also decreased, suggesting a reduced explanatory ability of CRP at 3 mg/L.
Salivary lysozyme conferred a much stronger association with CHD than the ADS oral infection score. We hypothesize that this additional risk increase might be attributable to impaired glucose metabolism and subsequent accumulation of advanced glycation end products (AGE) as depicted in the conceptual model (Figure I, available online at http://atvb.ahajournals.org). However, this hypothesis calls for further prospective studies.
Lysozyme is secreted locally, and there is no significant correlation between serum and salivary lysozyme.6 Salivary lysozyme may underscore dual pathways by which poor oral health may contribute to CHD pathogenesis.5 Poor dentition is a limiting factor for adequate intake of beneficial nutrients to prevent CHD (ie, fiber,7 antioxidants,8,9 and fruits and vegetables10). Moreover, edentulism encourages high fat and carbohydrate intake,11,12 thus, it may contribute to a higher level of AGE and subsequent CHD.13-15
The conclusion of our meta-analysis,16 that persons with periodontal disease might be at a higher risk of developing cardiovascular disease, has been corroborated by several recent trials reporting that periodontal treatment decreased the level of systemic CRP17-19 and further by other immunologic studies that linked the periodontal pathogen Porphyromonas gingivalis to atherosclerosis.20-22
Leukocytes may play a role in cardiopathogenesis, as Kowolik et al23 and Margolis et al24 concurred. Salivary lysozyme may be a marker for the dual contribution of oral leukocytes to cardiopathogenesis, via infection and elevated AGE deriving from an unhealthy diet.
In conclusion, increased quartiles of salivary lysozyme, which may be a consequence of oral infection or impaired glucose metabolism, were associated with increasing ORs (1.00, 1.16, 1.82, and 3.62, respectively, P for trend <0.0001) for CHD after controlling for traditional CHD risk factors.
Further prospective investigations are warranted to establish whether this is a causal relationship.
OR for CHD according to the quartiles of lysosyme levels.
References
- 1.Margolis KL, Manson JE, Greenland P, Rodabough RJ, Bray PF, Safford M, Grimm RHJ, Howard BV, Assaf AR, Prentice R. Leukocyte count as a predictor of cardiovascular events and mortality in postmenopausal women: the Women’s Health Initiative Observational Study. Arch Intern Med. 2005;165:500–508. doi: 10.1001/archinte.165.5.500. [DOI] [PubMed] [Google Scholar]
- 2.Suomalainen K, Saxen L, Vilja P, Tenovuo J. Peroxidases, lactoferrin and lysozyme in peripheral blood neutrophils, gingival crevicular fluid and whole saliva of patients with localized juvenile periodontitis. Oral Dis. 1996;2:129–134. doi: 10.1111/j.1601-0825.1996.tb00213.x. [DOI] [PubMed] [Google Scholar]
- 3.Zheng F, Cai W, Mitsuhashi T, Vlassara H. Lysozyme enhances renal excretion of advanced glycation endproducts in vivo and suppresses adverse age-mediated cellular effects in vitro: a potential AGE sequestration therapy for diabetic nephropathy? Mol Med. 2001;7:737–747. [PMC free article] [PubMed] [Google Scholar]
- 4.Eckel RH, Wassef M, Chait A, Sobel B, Barrett E, King G, Lopes-Virella M, Reusch J, Ruderman N, Steiner G, Vlassara H. Prevention Conference VI: Diabetes and Cardiovascular Disease: Writing Group II: pathogenesis of atherosclerosis in diabetes. Circulation. 2002;105:e138–e143. doi: 10.1161/01.cir.0000013954.65303.c5. [DOI] [PubMed] [Google Scholar]
- 5.Janket SJ, Qvarnstrom M, Meurman JH, Baird AE, Nuutinen P, Jones JA. Asymptotic dental score and prevalent coronary heart disease. Circulation. 2004;109:1095–1100. doi: 10.1161/01.CIR.0000118497.44961.1E. [DOI] [PubMed] [Google Scholar]
- 6.Wagner V, Wagnerova M. Lack of correlation between serum and salivary concentration levels of immunoglobulin A and lysozyme (muramidase) J Hyg Epidemiol Microbiol Immunol. 1989;33:353–356. [PubMed] [Google Scholar]
- 7.Nowjack-Raymer RE, Sheiham A. Association of edentulism and diet and nutrition in US adults. J Dent Res. 2003;82:123–126. doi: 10.1177/154405910308200209. [DOI] [PubMed] [Google Scholar]
- 8.Hung HC, Willett W, Ascherio A, Rosner BA, Rimm E, Joshipura KJ. Tooth loss and dietary intake. J Am Dent Assoc. 2003;134:1185–1192. doi: 10.14219/jada.archive.2003.0353. [DOI] [PubMed] [Google Scholar]
- 9.Lowe G, Woodward M, Rumley A, Morrison C, Tunstall-Pedoe H, Stephen K. Total tooth loss and prevalent cardiovascular disease in men and women: possible roles of citrus fruit consumption, vitamin C, and inflammatory and thrombotic variables. J Clin Epidemiol. 2003;56:694–700. doi: 10.1016/s0895-4356(03)00086-6. [DOI] [PubMed] [Google Scholar]
- 10.Joshipura KJ, Hu FB, Manson JE, Stampfer MJ, Rimm EB, Speizer FE, Colditz G, Ascherio A, Rosner B, Spiegelman D, Willett WC. The effect of fruit and vegetable intake on risk for coronary heart disease [see comment] Ann Intern Med. 2001;134:1106–1114. doi: 10.7326/0003-4819-134-12-200106190-00010. [DOI] [PubMed] [Google Scholar]
- 11.Johansson I, Tidehag P, Lundberg V, Hallmans G. Dental status, diet and cardiovascular risk factors in middle-aged people in northern Sweden. Community Dent Oral Epidemiol. 1994;22:431–436. doi: 10.1111/j.1600-0528.1994.tb00792.x. [DOI] [PubMed] [Google Scholar]
- 12.Janket S, Baird A, Chuang S, Jones J, et al. Examining the link between coronary heart disease and the elimination of chronic dental infections. J Am Dent Assoc. 2001;132:1648–1650. doi: 10.14219/jada.archive.2001.0300. Heart of the matter/a response letter to the article by Hujoel P. [DOI] [PubMed] [Google Scholar]
- 13.Libby P, Plutzky J. Diabetic macrovascular disease: the glucose paradox? [comment] Circulation. 2002;106:2760–2763. doi: 10.1161/01.cir.0000037282.92395.ae. [DOI] [PubMed] [Google Scholar]
- 14.Vlassara H. Recent progress in advanced glycation end products and diabetic complications. Diabetes. 1997;46(suppl 2):S19–S25. doi: 10.2337/diab.46.2.s19. [DOI] [PubMed] [Google Scholar]
- 15.Liu S, Willett WC. Dietary glycemic load and atherothrombotic risk. Curr Atheroscler Rep. 2002;4:454–461. doi: 10.1007/s11883-002-0050-2. [DOI] [PubMed] [Google Scholar]
- 16.Janket S, Baird A, Chuang S, Jones JA. Meta-analysis of periodontal disease and risk of coronary heart disease and stroke. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:559–569. doi: 10.1067/moe.2003.107. [DOI] [PubMed] [Google Scholar]
- 17.D’Aiuto F, Ready D, Tonetti MS. Periodontal disease and C-reactive protein-associated cardiovascular risk. J Periodontol. 2004;39:236–241. doi: 10.1111/j.1600-0765.2004.00731.x. [DOI] [PubMed] [Google Scholar]
- 18.D’Aiuto F, Parkar M, Andreou G, Brett PM, Ready D, Tonetti MS. Periodontitis and atherogenesis: causal association or simple coincidence? J Clin Periodontol. 2004;31:402–411. doi: 10.1111/j.1600-051X.2004.00580.x. [DOI] [PubMed] [Google Scholar]
- 19.Iwamoto Y, Nishimura F, Soga Y, Takeuchi K, Kurihara M, Takashiba S, Murayama Y. Antimicrobial periodontal treatment decreases serum C-reactive protein, tumor necrosis factor-alpha, but not adiponectin levels in patients with chronic periodontitis. J Periodontol. 2003;74:1231–1236. doi: 10.1902/jop.2003.74.8.1231. [DOI] [PubMed] [Google Scholar]
- 20.Choi J, Chung S, Kang H, Rhim B, Kim S, Kim S. Establishment of porhyromonas gingivalis heat-shock-proteint specific T-cell line from atherosclerosis patients. J Dent Res. 2002;81:344–348. doi: 10.1177/154405910208100511. [DOI] [PubMed] [Google Scholar]
- 21.Li L, Messas E, Batista EL, Jr, Levine RA, Amar S. Porphyromonas gingivalis infection accelerates the progression of atherosclerosis in a heterozygous apolipoprotein E-deficient murine model. Circulation. 2002;105:861–867. doi: 10.1161/hc0702.104178. [erratum appears in Circulation 2002;105:1617] [DOI] [PubMed] [Google Scholar]
- 22.Janket S, Meurman JH. Underlying chronic infection and leukocyte count [Comments/letter] Arch Intern Med. 2005;165:1795. doi: 10.1001/archinte.165.15.1795-b. [DOI] [PubMed] [Google Scholar]
- 23.Kowolik MJ, Dowsett SA. Leukocyte response to dental plaque accumulation: a risk factor for heart disease? (letter/comments) Arch Intern Med. 2005;165:1795–1796. doi: 10.1001/archinte.165.15.1795-c. [DOI] [PubMed] [Google Scholar]
- 24.Margolis KL, Manson JE, Greenland P. Leukocyte response to dental plaque accumulation: a risk factor for heart disease? (In reply) Arch Intern Med. 2005;165:1796. [Google Scholar]