Abstract
The inhaled form of Bacillus anthracis infection may be fatal to humans. The current standard of care for inhalational anthrax postexposure prophylaxis is ciprofloxacin therapy twice daily for 60 days. The potent in vitro activity of oritavancin, a semisynthetic lipoglycopeptide, against B. anthracis (MIC against Ames strain, 0.015 μg/ml) prompted us to test its efficacy in a mouse aerosol-anthrax model. In postexposure prophylaxis dose-ranging studies, a single intravenous (i.v.) dose of oritavancin of 5, 15, or 50 mg/kg 24 h after a challenge with 50 to 75 times the median lethal dose of Ames strain spores provided 40, 70, and 100% proportional survival, respectively, at 30 days postchallenge. Untreated animals died within 4 days of challenge, whereas 90% of control animals receiving ciprofloxacin at 30 mg/kg intraperitoneally twice daily for 14 days starting 24 h after challenge survived. Oritavancin demonstrated significant activity post symptom development; a single i.v. dose of 50 mg/kg administered 42 h after challenge provided 56% proportional survival at 30 days. In a preexposure prophylaxis study, a single i.v. oritavancin dose of 50 mg/kg administered 1, 7, 14, or 28 days before lethal challenge protected 90, 100, 100, and 20% of mice at 30 days; mice treated with ciprofloxacin 24 h or 24 and 12 h before challenge all died within 5 days. Efficacy in pre- and postexposure models of inhalation anthrax, together with a demonstrated low propensity to engender resistance, promotes further study of oritavancin pharmacokinetics and efficacy in nonhuman primate models.
Bacillus anthracis, a gram-positive, spore-forming rod and the causative agent of anthrax, primarily causes disease in animals. In humans, it can produce a fatal disease if the spores are inhaled or ingested. The Centers for Disease Control and Prevention recognizes B. anthracis as a category A agent with recognized bioterrorism potential (http://www.bt.cdc.gov/agent/anthrax/needtoknow.asp; accessed 5 December 2007). Furthermore, the threat of emerging natural resistance or “engineered” resistance (29, 36) remains a significant concern (24). For example, although penicillin is considered to be a treatment of choice for anthrax, numerous reports of β-lactamase-producing strains and of treatment failures have appeared in the literature (6, 13, 17, 30). Additionally, two open reading frames coding for β-lactamases have been identified in the B. anthracis genome (8, 32). Reports of B. anthracis resistance to ciprofloxacin, macrolides, and tetracyclines have likewise appeared (7, 9, 39). It is therefore important to reevaluate the spectrum of antibiotics that are either currently available or under development for anthrax treatment.
A widely accepted and well-characterized inhalation anthrax animal model for evaluation of antibiotic efficacy utilizes rhesus monkeys (16). However, this species is in short supply and other nonhuman primate models arguably are not characterized to the same extent with respect to pathophysiology, microbiology, and activity of control antibiotics that are used in treating the human form of the disease. The use of small-rodent models has proven invaluable in the assessment of antibiotic efficacy in other infectious diseases; such use minimizes the cost per antibiotic test and therefore increases the number of animals per test group, as well as the number of antibiotics or treatment regimens that can be tested at any given time. Recently, two murine aerosol challenge models of anthrax were characterized. Mouse pathophysiology reflects that seen in humans exposed to anthrax spores. While one model uses a capsule-deficient infecting strain (B. anthracis Sterne; 31), the other uses as the infecting strain B. anthracis Ames, a fully virulent, toxigenic, and capsule-producing isolate (22). The application of a predetermined dose and dose schedule based on “murine” infection modeling has been shown to greatly expand the utility of these small-animal models and allows for evaluation of the activity of test agents before efficacy testing in the more expensive and difficult nonhuman primate models (12).
Oritavancin is a novel, semisynthetic lipoglycopeptide that is currently in late-stage clinical development for complicated skin and skin structure infections (38). It exerts bactericidal activity against most clinically relevant gram-positive pathogens, including those phenotypically resistant to methicillin, vancomycin, fluoroquinolones, and macrolides. Oritavancin was previously shown to exert substantial activity against B. anthracis in vitro (20, 23). In addition, oritavancin accumulates significantly in macrophages and demonstrates potent activity in in vitro models of intracellular Staphylococcus aureus infections (4, 35). The demonstrated activity of oritavancin against B. anthracis in vitro and its accumulation and activity within macrophages, combined with the knowledge that dissemination of anthrax spores after aerosol challenge relies upon phagocytosis by macrophages and subsequent transit to the draining tracheobronchial lymph nodes (26), prompted us to ask whether oritavancin might exert particular activity in an animal model of inhalation anthrax.
The first objective of our study was to assess the in vitro activity of oritavancin against a collection of genetically diverse B. anthracis strains under recently optimized broth microdilution testing conditions with polysorbate 80 (10), which promotes quantitative drug recovery throughout the course of the assay (2). Second, we examined oritavancin pharmacokinetics in mice and characterized its activity in a well-characterized mouse model of inhalational anthrax (22). Efficacy data could then be applied to an FDA submission after nonhuman primate testing according to the “two animal rule” (14). Finally, we examined the propensity of oritavancin to select for resistance both in vitro and in vivo.
(Part of this work was presented at the 107th General Meeting of the American Society for Microbiology, Toronto, Ontario, Canada, 21 to 25 May 2007.)
MATERIALS AND METHODS
B. anthracis strains.
The 30 B. anthracis strains used in this study were from the United States Army Medical Research Institute of Infectious Diseases collection and included the Ames strain. The remaining strains were isolates from human or animal infections throughout the world and represent the eight genotype clades identified by Keim et al. (25).
Susceptibility of B. anthracis strains to oritavancin as measured by broth microdilution.
Oritavancin MICs were determined by broth microdilution in 96-well plates according to guidelines of the Clinical and Laboratory Standards Institute (10, 11). As recommended in guideline M100-S18 (10), polysorbate 80 was included at a final concentration of 0.002% throughout drug dissolution and all steps of the assay to minimize oritavancin binding to surfaces (2). To determine the impact, if any, of polysorbate 80 upon oritavancin MICs for B. anthracis, a parallel broth microdilution assay was conducted in which oritavancin was dissolved in water and drug dilutions were prepared without polysorbate 80. Quality control of oritavancin dilutions was established by using S. aureus ATCC 29213 with polysorbate 80 at 0.002% throughout; an acceptable range of oritavancin MICs against this strain is 0.015 to 0.12 μg/ml (10).
Animal research.
Research with mice was conducted in compliance with the Animal Welfare Act and other federal statutes and regulations relating to animals and experiments involving animals. Research adhered to principles stated in the Guide for the Care and Use of Laboratory Animals, National Research Council, 1996. The facilities in which this research was conducted are fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International.
Oritavancin pharmacokinetics and dosing determinations.
A pharmacokinetics study was performed with mice to compare oritavancin exposures in plasma after the administration of a single dose of oritavancin by the intravenous (i.v.) and intraperitoneal (i.p.) routes. Because multiple doses of test and control agents are typically required in the mouse model of inhalation anthrax for effective postexposure prophylaxis and treatment (22), the i.p. route is the preferred route of administration during therapy. However, the possibility of infrequent and even single i.v. administration of oritavancin has been established in efficacy studies in a neutropenic mouse model of S. aureus thigh infection (5), in an immunocompetent mouse model of Streptococcus pneumoniae infection (28), and in a rat model of S. aureus granuloma pouch infection (27). Mice (female CD-1; body weight, 19 to 21 g) received a single bolus dose of oritavancin of 32 mg/kg in dosing formulation (see below) either i.v. or i.p., and blood was collected by cardiac puncture (n = 3 mice/time point). Levels of oritavancin (total drug) in plasma were determined by a validated liquid chromatography-mass spectrometry method. Free oritavancin levels were calculated by using a value of 93.6% bound in mouse serum (W. Craig, unpublished data). Pharmacokinetic parameters were calculated by using WinNonlin software (Pharsight). All parameters were calculated by using a noncompartmental model.
Determination of efficacy of oritavancin in the mouse inhalation anthrax model. (i) Preparation of oritavancin dosing formulation.
Oritavancin for injection was formulated by dissolving oritavancin diphosphate (lot 01005PP00 [Targanta Therapeutics]; assay potency [volatile-free basis], 84.9%) in 5% dextrose in water to the appropriate concentration, followed by sterile filtration. Due to the saturable binding of oritavancin (2) and its near-quantitative loss to filter membranes at low drug concentrations (e.g., below 10 μg/ml; Targanta Therapeutics data, unpublished), oritavancin concentrations were maintained above 1 mg/ml during dissolution and filtration before dilution and administration.
(ii) B. anthracis strain and experimental design.
For trials of antibiotic efficacy, spores of B. anthracis Ames were prepared as described by Heine et al. (22), including heating the spore preparation to 65°C for 30 min before use; spores were then diluted in sterile water and used for an aerosol challenge at 50 to 75 times the median lethal dose (3.4 × 104 spores). Treatment groups generally consisted of 10 animals. Animals were observed and mortality was recorded to the end of the experiment, which ranged from 22 to 31 days postchallenge. For all experiments, negative control animals received either no treatment or vehicle (5% dextrose in water) alone. A positive control group that received ciprofloxacin at 30 mg/kg i.p., starting 24 h postchallenge, twice daily (q12h) for 14 days was routinely included as a control and comparator.
The three anthrax treatment models studied were postexposure prophylaxis, in which treatment began 24 h after challenge; postexposure treatment, in which treatment began 36, 42, or 48 h after challenge; and preexposure prophylaxis, in which drugs were administered up to 28 days before challenge.
(iii) Postexposure prophylaxis (single- and multiple-dose dose-ranging study).
Oritavancin was administered either i.p. at doses including 0.1, 0.3, 1, 3, 10, and 30 mg/kg once every 2 days (q48h) for 14 days or as a single i.v. dose of 5, 15, or 50 mg/kg. All treatments were initiated 24 h after challenge.
(iv) Postexposure treatment (single- and multiple-dose study).
To evaluate the efficacy of treatment after the appearance of clinical signs (i.e., post symptom development; 22), a study was performed in which therapy with oritavancin was delayed to either 36 or 48 h postchallenge. In this model, oritavancin was administered at 10 mg/kg i.p. q48 h for 14 days after the first dose at 36 or 48 h. Ciprofloxacin as a comparator agent was administered i.p. at 30 mg/kg q12h for 14 days beginning 36 or 48 h postchallenge. Alternatively, oritavancin treatment began 42 h postchallenge; for this group, oritavancin was administered as a single i.v. dose of 5, 15, or 50 mg/kg.
(v) Preexposure prophylaxis (single-dose study).
A single 50-mg/kg i.v. dose of oritavancin was administered either 24 h or 7, 14, or 28 days before challenge. As a comparator, ciprofloxacin was administered at 30 mg/kg i.p. either 24 h or 24 and 12 h before challenge.
Data analysis.
For all experiments, Kaplan-Meier curves were compared by the log rank test for significance over untreated controls, where differences in survival with P < 0.05 were considered significant.
Determination of bacterial burden in tissue.
Surviving mice from each group were euthanized at the experimental endpoint, typically at days 22 to 31 postchallenge. Lungs were aseptically removed, weighed, and homogenized in 1 ml of sterile water. Homogenates were serially diluted 1:10 in water, and 100-μl aliquots were plated on sheep blood agar plates (SBAP). To determine if anthrax spores were present, homogenates were heat shocked for 15 min at 65°C to kill vegetative cells and then serially diluted and plated on SBAP. Antibiotic susceptibilities of clones arising on SBAP were determined by broth microdilution (10, 11) with 0.002% polysorbate 80 throughout testing, as described above.
Methodology to examine in vitro resistance development to oritavancin in B. cereus.
B. cereus ATCC 4342 was subjected to serial passage (stepwise selection) in cation-adjusted Mueller-Hinton broth containing drugs at doubling dilution concentrations under standard susceptibility testing conditions (10, 11). The drugs used for selection were oritavancin, penicillin, ciprofloxacin, and rifampin. For oritavancin, polysorbate 80 was maintained at 0.002% for drug dissolution and dilution and in all steps of the broth microdilution assay (2, 10). Twenty cycles of broth microdilution assay were performed by using as the inoculum cells from the 0.5× MIC wells of the previous day's experiment. The test strain, B. cereus ATCC 4342, was tested in two independent rounds of 20 cycles for each agent. Any selectant with a fourfold or greater increase in the MIC of the challenge drug at day 20, compared to the MIC for the parent (unchallenged) strain at day 1, was passaged nonselectively (i.e., in the absence of drug) for an additional 5 days. After the nonselective growth period, broth microdilution MICs of oritavancin and comparator drugs were determined against the selectants and in parallel against the parent (unchallenged) strain.
RESULTS
Susceptibility of B. anthracis strains to oritavancin as measured by broth microdilution.
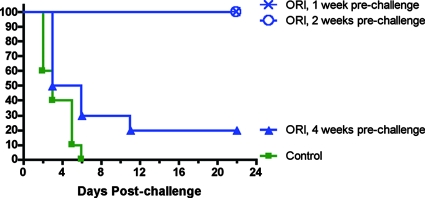
Oritavancin demonstrated potent activity in vitro against 30 strains of B. anthracis (Fig. 1) representing all eight genotype clades identified by Keim et al. (25). On average, oritavancin MICs decreased 4 doubling dilutions when susceptibilities were determined with polysorbate 80; the oritavancin MIC for 90% of the strains tested (MIC90) with polysorbate 80 (0.12 μg/ml; n = 30) was 16-fold lower than the MIC90 in the absence of polysorbate 80. This result is consistent with results from previous in vitro studies which showed a 16- to 32-fold increase in the oritavancin MIC90 for staphylococci and enterococci in the absence of polysorbate 80 as a result of drug binding to the surfaces of test vessels (2, 38). The oritavancin MIC for the Ames strain specifically shifted from 1 to 0.015 μg/ml in the presence of polysorbate 80. The one outlier strain in both determinations (oritavancin MIC, 4 μg/ml without polysorbate 80 and 1 μg/ml with polysorbate 80; Fig. 1) is known to be a high capsule producer. Minimum bactericidal concentrations were not determined for B. anthracis because of the presence of spores, which confounds the analysis (12). The broth microdilution results without polysorbate 80 that are presented here concur with results from an earlier in vitro study that was performed without polysorbate 80 and in which B. anthracis was found to be susceptible to oritavancin (23).
FIG. 1.
Oritavancin susceptibility distribution of B. anthracis (n = 30) in the absence and presence of 0.002% polysorbate 80. Susceptibilities were determined by broth microdilution according to CLSI M7-A7 and M100-S18 guidelines (10, 11). Solid black bars, no polysorbate 80; gray bars, with 0.002% polysorbate 80.
Oritavancin pharmacokinetics in mouse plasma.
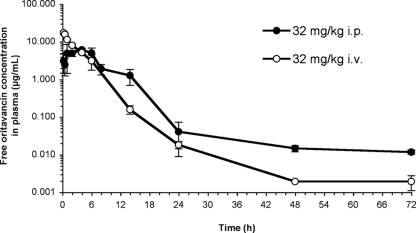
The plasma concentration-time profile of oritavancin after single i.v. dose (bolus) administration concurred with that from previous analyses of oritavancin pharmacokinetics in mice (5, 28). In the present study, the total oritavancin concentration was determined at each time point and then converted to the free oritavancin concentration by using a value for the fraction bound in mouse serum of 93.6% (W. Craig, unpublished data); calculated free oritavancin concentrations were plotted. After the administration of a single i.v. dose of oritavancin at 32 mg/kg to mice, the predicted free concentration of oritavancin in plasma remained above the MIC for the Ames strain of B. anthracis (0.015 μg/ml with polysorbate 80) for at least 24 h (Fig. 2). The observed free peak concentration, time to peak concentration, and area under the free-drug concentration-time curve from 0.25 to 72 h (fAUC0.25-72 h) were 17 μg/ml, 0.25 h, and 61 μg·h/ml, respectively, for the i.v. route and 6.1 μg/ml, 4 h, and 54 μg·h/ml, respectively, for the i.p. route. Thus, while the free-drug peak level in plasma was higher after i.v. versus i.p. administration and while the time to peak concentration was delayed to 4 h after i.p. administration, oritavancin exposures (measured here as fAUC0.25-72 h) were similar for the two routes. Because the maximum oritavancin concentration in serum/MIC and AUC/MIC ratios can predict efficacy in mouse models of penicillin-susceptible S. pneumoniae pneumonia (28), both the i.v. and i.p. routes of administration were deemed suitable to evaluate oritavancin efficacy because they offered similar total exposures for a given dose.
FIG. 2.
Concentration-time profile of oritavancin in mouse plasma after administration of a single 32-mg/kg dose by either the i.v. or the i.p. route. While total (bound plus free) oritavancin concentrations were measured, calculated free oritavancin concentrations, based on 93.6% protein binding in mouse serum, are plotted.
Oritavancin efficacy in the mouse inhalation anthrax model.
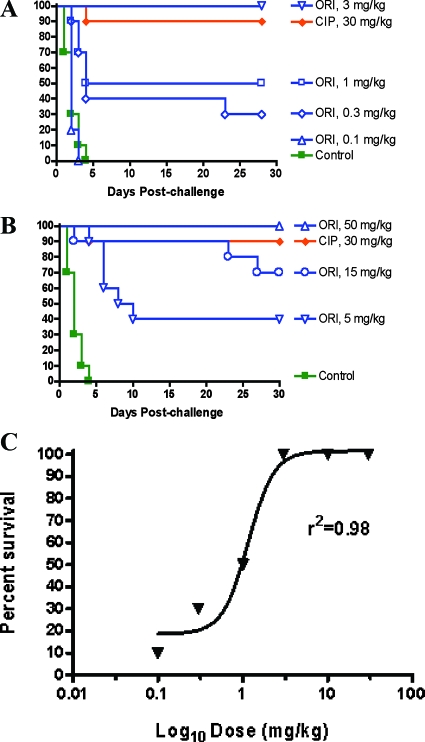
Postexposure prophylaxis model. The efficacy of oritavancin when administered by either the i.p. or the i.v. route was tested in the postexposure prophylaxis model, with the drug administered 24 h postchallenge. Oritavancin, when administered i.p. q48h for 14 days, provided significant protection compared to the untreated control group, with doses of 1 and 3 mg/kg protecting 50 and 100% of the mice, respectively (Fig. 3A). Furthermore, a single i.v. oritavancin dose of 15 or 50 mg/kg administered 24 h after challenge protected 70 or 100% of the mice, respectively (Fig. 3B). The protection provided by ciprofloxacin was similar (90% survival; Fig. 3A and B) but required i.p. dosing at 30 mg/kg/dose q12h for 14 days. This level of activity of ciprofloxacin concurs with that reported previously (22). A sigmoid Hill-type model was used to calculate the 50% effective dose (ED50). Based on the 14-day survival curve shown in Fig. 3C, when the infected mice were treated with oritavancin i.p. q48h beginning 24 h postchallenge, the ED50 was found to be 1.2 mg/kg (95% confidence interval [CI], 0.47 to 2.9 mg/kg). The Hill constant was 2.9. The fAUC0-48 h corresponding to the ED50 was 1.9 μg·h/ml (95% CI, 0.79 to 4.8 μg·h/ml).
FIG. 3.
Proportional survival from oritavancin (ORI) or ciprofloxacin (CIP) treatment in the postexposure prophylaxis model of inhalation anthrax. All treatments began 24 h postchallenge. Control animals received no treatment. (A) Mice in the CIP group received CIP i.p. at 30 mg/kg q12h for 14 days. ORI doses are indicated on the right and were administered i.p. q48h for 14 days. ORI doses of 10 and 30 mg/kg administered q48 h i.p. for 14 days provided 100% protection; the corresponding survival curves are not shown for clarity. (B) Mice in the CIP group received CIP i.p. at 30 mg/kg q12h for 14 days. Single ORI doses were administered i.v. and are indicated on the right. (C) Proportional 14-day survival as a function of ORI dose in the postexposure prophylaxis model of inhalation anthrax. The ED50 from a sigmoid Hill-type model was 1.2 mg/kg (95% CI, 0.47 to 2.9 mg/kg).
Table 1 shows that the spore load in lung tissue at the termination of the study did not exceed 5 × 104 CFU/g tissue in mice treated with oritavancin. Previous experiments showed that tissue spore burdens near or below this range are consistent with survival (22).
TABLE 1.
Summary of efficacy in the inhalational anthrax model and posttreatment spore counts in lungs of surviving mice
| Agent | Regimen | Start of therapy | % Proportional survivala | CFU/g in lung |
|---|---|---|---|---|
| None | 0 (100% dead at day 4) | NDb | ||
| CIPc | 30 mg/kg q12h × 14 days | 24 h postchallenge | 90e | 5.20 × 104 |
| ORId | 30 mg/kg i.p. q48h × 14 days | 24 h postchallenge | 100e | 1.82 × 104 |
| ORI | 10 mg/kg i.p. q48h × 14 days | 24 h postchallenge | 100e | 4.79 × 104 |
| ORI | 3 mg/kg i.p. q48h × 14 days | 24 h postchallenge | 100e | 3.68 × 104 |
| ORI | 1 mg/kg i.p. q48h × 14 days | 24 h postchallenge | 50f | 2.95 × 104 |
| ORI | 0.3 mg/kg i.p. q48h × 14 days | 24 h postchallenge | 30g | 2.80 × 104 |
| ORI | 0.1 mg/kg i.p. q48h × 14 days | 24 h postchallenge | 0 (100% dead at day 3) | ND |
| ORI | 50 mg/kg i.v. single dose | 24 h postchallenge | 100e | 3.61 × 104 |
| ORI | 15 mg/kg i.v. single dose | 24 h postchallenge | 70e | 2.03 × 104 |
| ORI | 5 mg/kg i.v. single dose | 24 h postchallenge | 40e | 3.50 × 104 |
| CIP | 30 mg/kg q12h × 14 days | 24 h postchallenge | 100e | 1.09 × 103 |
| CIP | 30 mg/kg q12h × 14 days | 36 h postchallenge | 70e | 2.88 × 103 |
| CIP | 30 mg/kg q12h × 14 days | 48 h postchallenge | 80g | 3.08 × 103 |
| ORI | 10 mg/kg i.p. q48h × 14 days | 24 h postchallenge | 100e | 3.50 × 103 |
| ORI | 10 mg/kg i.p. q48h × 14 days | 36 h postchallenge | 90f | 2.52 × 103 |
| ORI | 10 mg/kg i.p. q48h × 14 days | 48 h postchallenge | 50g | 1.68 × 103 |
| ORI | 50 mg/kg i.v. single dose | 42 h postchallenge | 55g | 0.74 × 103 |
| CIP | 30 mg/kg i.p. single dose | 24 h prechallenge | 0 (100% dead at day 3) | ND |
| CIP | 30 mg/kg i.p. two doses | 24 + 12 h prechallenge | 0 (100% dead at day 3) | ND |
| ORI | 50 mg/kg i.v. single dose | 24 h prechallenge | 100e | 1.98 × 103 |
| ORI | 50 mg/kg i.v. single dose | 7 days prechallenge | 90, 100e | 6.30 × 104 |
| ORI | 50 mg/kg i.v. single dose | 14 days prechallenge | 100e | 6.50 × 104 |
| ORI | 50 mg/kg i.v. single dose | 28 days prechallenge | 20h | 5.10 × 104 |
For 9 or 10 animals/group. P values were determined by log rank test versus the untreated control.
ND, not determined.
CIP, ciprofloxacin.
ORI, oritavancin.
P ≤ 0.0001.
P ≤ 0.001.
P ≤ 0.01.
P < 0.05.
Postexposure treatment model.
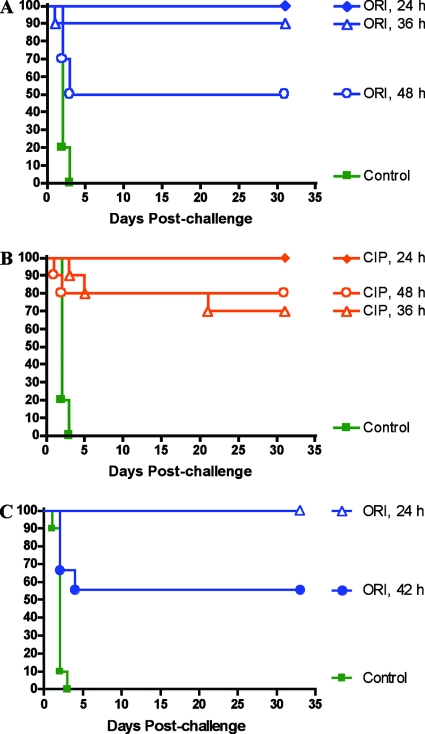
By 36 to 42 h, clinical signs of inhalational anthrax become evident in the mouse model (22, 26, 31); the efficacy of therapeutic agents including ciprofloxacin and doxycycline is significantly reduced, and mice succumb to fulminant bacteremia shortly thereafter (22). In a model of delayed treatment of postexposure inhalational anthrax, oritavancin provided 90 and 50% protection when treatment (10 mg/kg q48h for 14 days) was administered i.p. starting 36 and 48 h, respectively, postchallenge (Fig. 4A). Ciprofloxacin, administered at 30 mg/kg i.p. q12h for 14 days, protected 70 and 80% of the mice when treatment was initiated 36 and 48 h, respectively, after challenge (Fig. 4B). When we assessed the protection afforded by a single i.v. dose of oritavancin given 42 h postchallenge, we found that oritavancin at 50 mg/kg protected 56% of the mice (Fig. 4C). Thus, oritavancin offered significant protection when therapy, by both the i.p. and i.v. routes, was delayed until 36, 42, or 48 h postchallenge.
FIG. 4.
Proportional survival from oritavancin (ORI) or ciprofloxacin (CIP) treatment in the postexposure (delayed) treatment model of inhalation anthrax. Control animals received no treatment. (A) Mice in the ORI groups received ORI i.p. at 10 mg/kg q48h for 14 days. Treatment was initiated at 24 h (ORI, 24 h), 36 h (ORI, 36 h), or 48 h (ORI, 48 h) postchallenge. (B) Mice in the CIP groups received CIP i.p. at 30 mg/kg q12h for 14 days. Treatment was initiated at 24 h (CIP, 24 h), 36 h (CIP, 36 h) or 48 h (CIP, 48 h) postchallenge. (C) Mice received a single dose of ORI (50 mg/kg i.v.) either 24 or 42 h postchallenge.
As was found in the postexposure prophylaxis experiments described above, the load of B. anthracis spores in the lung tissue (≤3 × 103 CFU/g; Table 1) of mice treated with oritavancin at the end of the postexposure treatment study was consistent with survival (22).
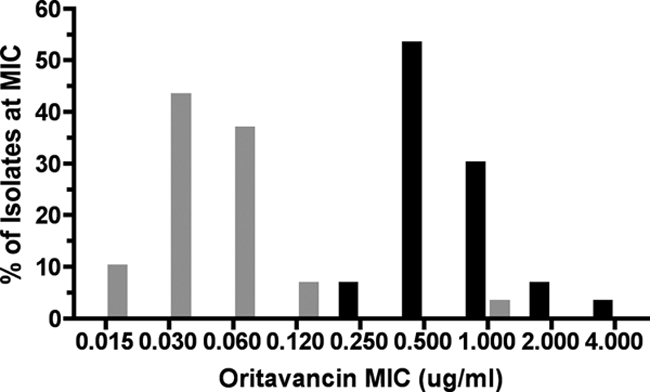
Preexposure prophylaxis model.
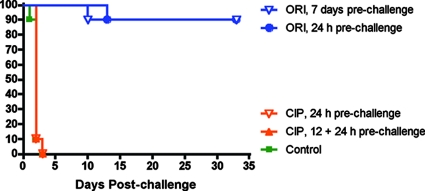
The striking efficacy of oritavancin when administered in single doses (Fig. 3B and 4C) and its extended half-life in mice (Fig. 2) (5, 28) and humans (15) prompted us to ask whether its activity could persist in a preexposure prophylaxis setting. Results presented in Fig. 5 indicate that oritavancin, when administered as a single i.v. dose of 50 mg/kg either 24 h or 7 days before a lethal spore challenge, protected 90% of the animals at the 33-day postchallenge endpoint. At the same dose, oritavancin prophylactic activity extended to 14 days prechallenge (100% survival at 22 days postchallenge) but declined sharply when oritavancin was administered 28 days before challenge (20% survival at 22 days postchallenge) (Fig. 6). For comparison, ciprofloxacin, when administered either as a single 30-mg/kg i.p. dose 24 h before a spore challenge or as two 30-mg/kg i.p. doses 24 and 12 h before a spore challenge, failed to protect, as all of the mice died from infection by day 4 postchallenge (Fig. 5). Thus, preexposure prophylaxis of lethal anthrax infection was unique to oritavancin.
FIG. 5.
Proportional survival of mice receiving a single dose of oritavancin (ORI; 50 mg/kg, i.v.) or one or two doses of ciprofloxacin (CIP; 30 mg/kg, i.p.) before spore challenge. ORI doses were administered either 24 h or 7 days before spore challenge; CIP doses were administered either 24 h or 24 and 12 h before challenge. Control animals received no treatment.
FIG. 6.
Proportional survival of mice that received a single dose of ORI (50 mg/kg, i.v.) at 1, 2, or 4 weeks before spore challenge. Control animals received no treatment.
Evaluation of oritavancin resistance development in vivo.
A key concern of extended antibiotic treatment regimens is the emergence of drug resistance during therapy, which can confound resolution of the disease. To address whether oritavancin treatment failures in the mouse model of inhalational anthrax may have resulted from decreasing oritavancin susceptibility of the infecting strain, oritavancin MICs for B. anthracis bacteria that were cultured from animals that died during oritavancin therapy were determined and compared to the MIC for the infecting (naïve) strain. Broth microdilution assays under standard conditions with polysorbate 80 for oritavancin (10, 11) demonstrated that the recovered isolates were as susceptible to oritavancin as the naïve strain was (i.e., MIC identical or twofold different).
Stepwise selection for oritavancin resistance in B. cereus in vitro.
Deliberate manipulation of B. anthracis in efforts to augment inherent resistance or to engineer resistance may pose a significant biosafety risk. To extend the analysis of oritavancin resistance emergence, a surrogate for B. anthracis, B. cereus ATCC 4342, was tested for its propensity to develop resistance to oritavancin and control drugs penicillin, ciprofloxacin, and rifampin by stepwise selection in vitro in broth medium under standard susceptibility testing (MIC assay) conditions (10, 11) with polysorbate 80 in assays of oritavancin. After 20 cycles of selection, selectants with a fourfold or greater increase in the MIC of the challenge drug were passaged nonselectively; MICs of oritavancin and comparator agents were then determined in parallel for both the stepwise selectant and the parent (unchallenged) strain. Results indicated that the oritavancin MICs of oritavancin selectants did not differ by more than twofold relative to those of the parent strain (Table 2). In contrast, the following increases in the MICs of the comparator agents that were used for selection were noted: ciprofloxacin, 4- to 32-fold; rifampin, 8- to 16-fold; penicillin, 8- to >16,000-fold. The high level of penicillin resistance encountered during one of the two independent in vitro stepwise selection studies may have resulted from the expression of a cryptic or inducible β-lactamase (37).
TABLE 2.
Results of in vitro stepwise resistance selection with B. cereus ATCC 4342a
| Agent | MIC (μg/ml) for:
|
Fold change in MIC | |
|---|---|---|---|
| Parent | Selectant | ||
| Oritavancin | 0.004-0.008 | 0.008 | 1-2 |
| Ciprofloxacin | 0.12 | 0.5-4 | 4-32 |
| Rifampin | 0.03 | 0.25-0.5 | 8-16 |
| Penicillin | 0.008 | 0.06->128 | 8->16,000 |
Twenty daily cycles of drug selection, followed by 5 days of nonselective growth, for those isolates that showed fourfold or greater increases in the MIC relative to the MIC for the parent strain. Results of two independent experiments are shown as ranges where the result differed and as a single value where the results were identical between replicates.
DISCUSSION
Oritavancin, a lipoglycopeptide antibiotic that is currently in development for skin and soft-tissue infections, demonstrated potent activity against B. anthracis both in vitro and in mice. Broth microdilution experiments with polysorbate 80 yielded an oritavancin MIC90 of 0.12 μg/ml with 30 genetically diverse strains of B. anthracis. In animal studies, oritavancin administered by either the i.p. or the i.v. route increased the proportional survival of mice that had received a lethal challenge of B. anthracis spores. Characterization of oritavancin activity and studies of its propensity to select for resistance in vitro and in vivo in the present study led us to conclude that oritavancin may offer significant potential for anthrax treatment.
Oritavancin administered i.p. at 3 mg/kg q48h for 14 days or i.v. at 50 mg/kg as a single dose was at least as active as ciprofloxacin administered at 30 mg/kg q12h for 14 days when treatments began 24 h postchallenge. The number of doses of oritavancin was therefore substantially lower than that of ciprofloxacin to achieve equivalent protection; either 7 i.p. doses or a single i.v. dose of oritavancin provided 100% protection, whereas 28 i.p. doses of ciprofloxacin were required to achieve 90 to 100% protection. We note that single i.v. oritavancin doses of 32 and 50 mg/kg in mice are predicted (or extrapolated) to provide free-drug exposures in plasma of approximately 61 and 95 μg·h/ml, respectively (fAUC0.25-72 h, this study; fAUC0-24 h, reference 5). For comparison, an oritavancin fAUC0-24 h of 167 μg·h/ml is predicted in human plasma following a single 800-mg i.v. dose (15), with a human serum protein binding value of 85% (5). Thus, total drug exposures that provide maximal or near-maximal single-dose efficacy in the mouse inhalational anthrax model are clinically relevant. Any selection of dose and dose regimen for eventual therapeutic use in humans, however, must consider the higher serum protein binding levels in mice compared to those in humans and both pharmacokinetic and efficacy data in nonhuman primates.
The currently recommended treatment strategy for postexposure anthrax requires a lengthy (60-day) course of ciprofloxacin administered q12h (34). An infrequent or even single-dose dosing strategy such as that demonstrated to be effective for oritavancin in the mouse model could thus prove to be beneficial after accidental or deliberate exposure of citizens to anthrax spores because it may potentially circumvent problems of poor compliance and resulting compromised treatment efficacy.
Late deaths in the 15-mg/kg oritavancin single i.v. dose treatment group were most likely due to outgrowth of residual spores still present in the lung tissue, possibly after antibiotic levels dropped below an as-yet-undefined therapeutic threshold. After the single dose of oritavancin of 50 mg/kg, for which there were no late deaths, the spore burden was predictably reduced to below the infection threshold (22) before the level of oritavancin dropped below its therapeutic threshold. Further pharmacokinetic-pharmacodynamic studies with oritavancin in the mouse aerosol anthrax model may be useful to identify oritavancin levels in plasma and the lungs, or intracellular levels, that would be predictive of efficacy.
Delay of the start of treatment from 24 h to at least 36 h postchallenge in the mouse aerosol anthrax model results in the appearance of clinical signs associated with dissemination of anthrax into the blood and tissues (22). This model has therefore been termed the postexposure treatment model, as it may reflect the need for long and aggressive courses of therapy after the onset of symptoms to achieve cure in humans. Oritavancin demonstrated substantial activity in this model of postexposure treatment, achieving 90, 55, and 50% protection when treatment was initiated at 36, 42, or 48 h postchallenge, respectively. While the protection that was provided by oritavancin in all tests of postexposure treatment remained statistically significantly different from the untreated control, the modest proportional survival provided by oritavancin when treatment was delayed to 42 or 48 h postchallenge highlights the increasing stringency of the treatment model as the delay between challenge and initiation of therapy increases.
The preexposure prophylaxis that was afforded by a single 50-mg/kg i.v. dose of oritavancin 24 h before aerosol challenge underscores the extended half-life of this drug (5, 15, 27, 28). Furthermore, this finding suggests that oritavancin may concentrate in those cellular compartments where spores may germinate in the early stages of infection (24, 26). This idea is consistent with data that show significant intracellular accumulation of oritavancin and its potent activity against intracellular S. aureus in macrophages in vitro (35, 41).
Further studies with nonhuman primates to predict whether oritavancin could serve as an alternative therapy for prophylaxis or treatment after accidental or deliberate exposure of humans to B. anthracis are now warranted. Due to the persistence of spores in the lungs and tissues of individuals exposed to B. anthracis, current recommended therapies must continue for at least 60 days. The enhanced efficacy of oritavancin in vivo in the mouse aerosol model suggests that less frequent dosing relative to ciprofloxacin may still provide a similar degree of protection. Importantly, infrequent oritavancin dosing in vivo did not lead to the development of oritavancin resistance. We propose that the multiple mechanisms of action of oritavancin (1, 3, 33, 42) should allow it to retain activity against drug-resistant strains of B. anthracis, including those resistant to penicillin, macrolides, fluoroquinolones, and vancomycin, throughout oritavancin therapy.
Although penicillin has long been considered a treatment of choice for anthrax, there are numerous reports that suggest the emergence of resistance to penicillin (6, 13, 30). Furthermore, resistance to ciprofloxacin, macrolides, and tetracyclines in specific B. anthracis strains has also been reported (7, 9, 39). In our study, stable mutants of a surrogate organism, B. cereus, demonstrating reduced susceptibility to oritavancin were not obtained by stepwise oritavancin selection in vitro. In contrast, mutants showing at least a fourfold reduced susceptibility to ciprofloxacin, rifampin, and penicillin were isolated during the course of 20 days of selection with these agents (Table 2). These findings are supported by the finding that oritavancin MICs for B. anthracis clones recovered and cultured from mice that died during oritavancin treatment were equivalent to or within 1 doubling dilution of the MIC of the infecting Ames strain. Together, these findings predict that the potential for B. anthracis to develop high-level resistance to oritavancin during therapy is low.
Overall, the findings suggest that oritavancin is of significant interest for further development, potentially for prophylactic use for first responders to anthrax threats and for postexposure prophylaxis and treatment in cases of known or suspected anthrax exposure. Relative to other investigational or clinically used agents that were recently evaluated in in vivo models of inhalational anthrax (daptomycin [21], dalbavancin [19], cethromycin [40], and faropenem [18]), the single-dose efficacy of oritavancin in postexposure prophylaxis, postexposure treatment, and preexposure prophylaxis of inhalational anthrax is unrivalled. Future studies will assess oritavancin pharmacokinetics and efficacy in nonhuman primate models of inhalational anthrax and characterize oritavancin pharmacodynamics in the mouse model of preexposure prophylaxis in an attempt to define a threshold for plasma and intracellular drug levels that predict postchallenge protection.
Acknowledgments
The research with B. anthracis described herein was sponsored by the Defense Threat Reduction Agency, project 02-4-2C-013 (H.S.H.).
The opinions, interpretations, conclusions, and recommendations are ours and are not necessarily endorsed by the U.S. Army and the Department of Defense.
We thank Karine Laquerre, Valérie Ostiguy, Ibtihal Fadhil, Cordelia Cadieux, Odette Bélanger, and Adel Rafai Far for characterizing oritavancin pharmacokinetics in mice. We acknowledge the support of Ingrid Sarmiento for assistance with stepwise selection experiments.
Footnotes
Published ahead of print on 7 July 2008.
REFERENCES
- 1.Allen, N. E., and T. I. Nicas. 2003. Mechanism of action of oritavancin and related glycopeptide antibiotics. FEMS Microbiol. Rev. 26:511-532. [DOI] [PubMed] [Google Scholar]
- 2.Arhin, F. F., I. Sarmiento, A. Belley, G. A. McKay, D. C. Draghi, P. Grover, D. Sahm, T. R. Parr, Jr., and G. Moeck. 2008. Effect of polysorbate 80 on oritavancin binding to plastic surfaces: implications for susceptibility testing. Antimicrob. Agents Chemother. 52:1597-1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arhin, F. F., I. Sarmiento, T. R. Parr, Jr., and G. Moeck. 2007. Mechanisms of action of oritavancin in Staphylococcus aureus, abstr. C1-1471, p. 85. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother. American Society for Microbiology, Washington, DC.
- 4.Barcia-Macay, M., C. Seral, M. P. Mingeot-Leclercq, P. M. Tulkens, and F. Van Bambeke. 2006. Pharmacodynamic evaluation of the intracellular activities of antibiotics against Staphylococcus aureus in a model of THP-1 macrophages. Antimicrob. Agents Chemother. 50:841-851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boylan, C. J., K. Campanale, P. W. Iversen, D. L. Phillips, M. L. Zeckel, and T. R. Parr, Jr. 2003. Pharmacodynamics of oritavancin (LY333328) in a neutropenic-mouse thigh model of Staphylococcus aureus infection. Antimicrob. Agents Chemother. 47:1700-1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bradaric, N., and V. Punda-Polic. 1992. Cutaneous anthrax due to penicillin-resistant Bacillus anthracis transmitted by an insect bite. Lancet 340:306-307. [DOI] [PubMed] [Google Scholar]
- 7.Brook, I., T. B. Elliott, H. I. Pryor II, T. E. Sautter, B. T. Gnade, J. H. Thakar, and G. B. Knudson. 2001. In vitro resistance of Bacillus anthracis Sterne to doxycycline, macrolides and quinolones. Int. J. Antimicrob. Agents 18:559-562. [DOI] [PubMed] [Google Scholar]
- 8.Chen, Y., F. C. Tenover, and T. M. Koehler. 2004. β-Lactamase gene expression in a penicillin-resistant Bacillus anthracis strain. Antimicrob. Agents Chemother. 48:4873-4877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choe, C., S. Bouhaouala, I. Brook, T. Elliott, and G. Knudson. 2000. In vitro development of resistance to ofloxacin and doxycycline in Bacillus anthracis Sterne. Antimicrob. Agents Chemother. 44:1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clinical and Laboratory Standards Institute. 2008. Performance standards for antimicrobial susceptibility testing; eighteenth informational supplement. CLSI document M100-S18. Clinical and Laboratory Standards Institute, Wayne, PA.
- 11.Clinical and Laboratory Standards Institute. 2006. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard—seventh edition. CLSI document M7-A7. Clinical and Laboratory Standards Institute, Wayne, PA.
- 12.Deziel, M. R., H. Heine, A. Louie, M. Kao, W. R. Byrne, J. Basset, L. Miller, K. Bush, M. Kelly, and G. L. Drusano. 2005. Effective antimicrobial regimens for use in humans for therapy of Bacillus anthracis infections and postexposure prophylaxis. Antimicrob. Agents Chemother. 49:5099-5106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doğanay, M., and N. Aydin. 1991. Antimicrobial susceptibility of Bacillus anthracis. Scand. J. Infect. Dis. 23:333-335. [DOI] [PubMed] [Google Scholar]
- 14.Federal Register. 2002. New drug and biological drug products; evidence needed to demonstrate effectiveness of new drugs when human efficacy studies are not ethical or feasible. Final rule. Fed. Regist. 67:37988-37998. [PubMed] [Google Scholar]
- 15.Fetterly, G. J., C. M. Ong, S. M. Bhavnani, J. S. Loutit, S. B. Porter, L. G. Morello, P. G. Ambrose, and D. P. Nicolau. 2005. Pharmacokinetics of oritavancin in plasma and skin blister fluid following administration of a 200-milligram dose for 3 days or a single 800-milligram dose. Antimicrob. Agents Chemother. 49:148-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Friedlander, A. M., S. L. Welkos, M. L. Pitt, J. W. Ezzell, P. L. Worsham, K. J. Rose, B. E. Ivins, J. R. Lowe, G. B. Howe, P. Mikesell, and W. B. Lawrence. 1993. Postexposure prophylaxis against experimental inhalation anthrax. J. Infect. Dis. 167:1239-1242. [DOI] [PubMed] [Google Scholar]
- 17.Gold, H. 1955. Anthrax: a report of one hundred seventeen cases. Arch. Intern. Med. 96:387-396. [DOI] [PubMed] [Google Scholar]
- 18.Heine, H. S., C. M. Rubino, J. Bassett, L. Miller, P. G. Ambrose, S. M. Bhavnani, A. Forrest, G. L. Drusano, A. Beaudry, J. Li, N. Janjic, and S. C. Gill. 2007. Pharmacokinetic-pharmacodynamic (PK-PD) assessment of faropenem (FAR) in a lethal murine-Bacillus anthracis (BA) inhalation post-exposure prophylaxis model, abstr. A-1435, p. 34. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother. American Society for Microbiology, Washington, DC.
- 19.Heine, H. S., J. Bassett, and L. Miller. 2005. In vitro and in vivo activity of dalbavancin (DAL) against Bacillus anthracis (BA), abstr. F-2079, p. 232. Abstr. 45th Intersci. Conf. Antimicrob. Agents Chemother. American Society for Microbiology, Washington, DC.
- 20.Heine, H. S., J. Bassett, L. Miller, A. Basset, T. R. Parr, Jr., and G. Moeck. 2007. Efficacy of oritavancin in a murine model of Bacillus anthracis spore inhalation anthrax, abstr. A-101, p. 23. Abstr. 107th Gen. Meet. Am. Soc. Microbiol. American Society for Microbiology, Washington, DC.
- 21.Heine, H. S., J. Bassett, L. Miller, G. P. Andrews, and W. R. Byrne. 2004. Efficacy of daptomycin against Bacillus anthracis (anthrax) in a murine model of anthrax-spore inhalation, abstr. A-051, p. 10-11. Abstr. 104th Gen. Meet. Am. Soc. Microbiol. American Society for Microbiology, Washington, DC.
- 22.Heine, H. S., J. Bassett, L. Miller, J. M. Hartings, B. E. Ivins, M. L. Pitt, D. Fritz, S. L. Norris, and W. R. Byrne. 2007. Determination of antibiotic efficacy against Bacillus anthracis in a mouse aerosol challenge model. Antimicrob. Agents Chemother. 51:1373-1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heine, H. S., R. Dicks, and G. Andrews. 2001. In vitro activity of oritavancin (LY333328), levofloxacin, meropenem, GAR936 and linezolid against strains of Bacillus anthracis, abstr. E-524, p. 173. Abstr. 41st Intersci. Conf. Antimicrob. Agents Chemother. American Society for Microbiology, Washington, DC.
- 24.Inglesby, T. V., T. O'Toole, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. M. Friedlander, J. Gerberding, J. Hauer, J. Hughes, J. McDade, M. T. Osterholm, G. Parker, T. M. Perl, P. K. Russell, and K. Tonat. 2002. Anthrax as a biological weapon, 2002: updated recommendations for management. JAMA 287:2236-2252. [DOI] [PubMed] [Google Scholar]
- 25.Keim, P., L. B. Price, A. M. Klevytska, K. L. Smith, J. M. Schupp, R. Okinaka, P. J. Jackson, and M. E. Hugh-Jones. 2000. Multiple-locus variable-number tandem repeat analysis reveals genetic relationships within Bacillus anthracis. J. Bacteriol. 182:2928-2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leffel, E. K., and L. M. Pitt. 2006. Anthrax, p. 77-93. In J. R. Swearengen (ed.), Biodefense. Research methodology and animal models. CRC Press Taylor and Francis, Boca Raton, FL.
- 27.Lehoux, D., F. F. Arhin, I. Fadhil, K. Laquerre, V. Ostiguy, I. Sarmiento, G. Moeck, and T. R. Parr, Jr. 2006. Oritavancin demonstrates rapid and sustained bactericidal activity in the rat granuloma pouch model of Staphylococcus aureus infection, abstr. B-404, p. 38. Abstr. 46th Intersci. Conf. Antimicrob. Agents Chemother. American Society for Microbiology, Washington, DC.
- 28.Lehoux, D., G. A. McKay, I. Fadhil, K. Laquerre, M. Malouin, V. Ostiguy, G. Moeck, and T. R. Parr, Jr. 2007. Efficacy of oritavancin in a mouse model of Streptococcus pneumoniae pneumonia, abstr. P-1781. Abstr. 17th Eur. Congr. Clin. Microbiol. Infect. Dis. and 25th Int. Congr. Chemother. European Society of Clinical Microbiologyand Infectious Diseases, Basel, Switzerland.
- 29.Leitenberg, M. 1993. The biological weapons program of the former Soviet Union. Biologicals 212:187-191. [DOI] [PubMed] [Google Scholar]
- 30.Lightfoot, N. F., R. J. D. Scott, and P. C. B. Turnbull. 1990. Antimicrobial susceptibility of Bacillus anthracis. Salisbury Med. Bull. 68(Suppl.):95-98. [Google Scholar]
- 31.Loving, C. L., M. Kennett, G. M. Lee, V. K. Grippe, and T. J. Merkel. 2007. Murine aerosol challenge model of anthrax. Infect. Immun. 75:2689-2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Materon, I. C., M. Queenan, T. M. Koehler, K. Bush, and T. Palzkill. 2003. Biochemical characterization of β-lactamases Bla1 and Bla2 from Bacillus anthracis. Antimicrob. Agents Chemother. 47:2040-2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McKay, G. A., I. Fadhil, S. Beaulieu, S. Ciblat, A. Rafai Far, G. Moeck, and T. R. Parr, Jr. 2006. Oritavancin disrupts transmembrane potential and membrane integrity concomitantly with cell killing in Staphylococcus aureus and vancomycin-resistant enterococci, abstr. C1-682, p. 76. Abstr. 46th Intersci. Conf. Antimicrob. Agents Chemother. American Society for Microbiology, Washington, DC.
- 34.Meyerhoff, A., R. Albrecht, J. M. Meyer, P. Dionne, K. Higgins, and D. Murphy. 2004. US Food and Drug Administration approval of ciprofloxacin hydrochloride for management of postexposure inhalational anthrax. Clin. Infect. Dis. 39:303-308. [DOI] [PubMed] [Google Scholar]
- 35.Nguyen, H. A., O. Denis, A. Vergison, P. M. Tulkens, M. Struelens, and F. Van Bambeke. 2007. Comparative intracellular activity of 10 antistaphylococcal antibiotics (AABS) against a stable small colony variant (SCV) of S. aureus in a model of human THP-1 macrophages, abstr. A-1437, p. 34. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother. American Society for Microbiology, Washington, DC.
- 36.Pile, J. C., J. D. Malone, E. M. Eitzen, and A. M. Friedlander. 1998. Anthrax as a potential biological warfare agent. Arch. Intern. Med. 158:429-434. [DOI] [PubMed] [Google Scholar]
- 37.Pollock, M. R. 1950. Penicillinase adaptation in B. cereus: adaptive enzyme formation in the absence of free substrate. Br. J. Exp. Pathol. 31:739-753. [PMC free article] [PubMed] [Google Scholar]
- 38.Poulakou, G., and H. Giamarellou. 2008. Oritavancin: a new promising agent in the treatment of infections due to gram-positive pathogens. Expert Opin. Investig. Drugs 17:225-243. [DOI] [PubMed] [Google Scholar]
- 39.Price, L. B., A. Volger, T. Pearson, J. D. Busch, J. M. Schupp, and P. Keim. 2003. In vitro selection and characterization of Bacillus anthracis mutants with high-level resistance to ciprofloxacin. Antimicrob. Agents Chemother. 47:2362-2365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sivko, G., K. Gebhardt, P. Olson, R. Hunt, Z. Xu, P. Flavin, D. Eiznhamer, and M. Flavin. 2007. Efficacy of cethromycin against a lethal inhalation anthrax challenge in rhesus macaques, abstr. B-2031, p. 64-65. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother. American Society for Microbiology, Washington, DC.
- 41.Van Bambeke, F., S. Carryn, C. Seral, H. Chanteux, D. Tyteca, M. P. Mingeot-Leclercq, and P. M. Tulkens. 2004. Cellular pharmacokinetics and pharmacodynamics of the glycopeptide antibiotic oritavancin (LY333328) in a model of J774 mouse macrophages. Antimicrob. Agents Chemother. 48:2853-2860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang, T., S. Walker, and D. E. Kahne. 2007. Probing the mechanism of inhibition of bacterial peptidoglycan glycotransferases by glycopeptide analogs, abstr. C1-1474, p. 86. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother. American Society for Microbiology, Washington, DC.