Abstract
Objective
To determine whether a transtheoretical model-tailored expert system intervention increases dual method contraceptive use compared to a non-tailored educational intervention.
Study Design
We performed a randomized clinical trial of 542 women at high-risk for sexually transmitted infections (STIs) and unintended pregnancy. The intervention group received computer-based tailored feedback using a multimedia program. The control group received general contraceptive information and non-tailored advice.
Results
Participants in the intervention group were more likely to report use of dual contraceptive methods during follow-up (adjusted HRR = 1.70, 95% CI 1.09, 2.66) compared to controls. However, there were no differences in the rates of incident STI or unintended pregnancy between the two groups.
Conclusions
The computer-based TTM-tailored intervention resulted in a 70% increase in reported dual method contraceptive use in a group of women at high-risk for STIs and unintended pregnancy. Inconsistent use of dual methods may explain the lack of effect on unintended pregnancy rates and incident STIs.
Keywords: prevention, contraception, sexually transmitted diseases, unplanned pregnancy
INTRODUCTION
Unintended pregnancy, sexually transmitted infections (STIs), and the adverse health consequences of STIs are widespread public health problems in the United States and worldwide. An estimated 79 million pregnancies worldwide are unintended each year. 1 In 2000, in the United States, there were 3.2 million unintended pregnancies 2 and almost half of all pregnancies in the U.S. were unintended. 3 Additionally, in 2005 there were over 976,000 new cases of Chlamydia trachomatis infection - a 5.1% increase compared to 2004. The CDC also reported the first increase in reported cases of Neisseria gonorrhoeae infection since 1999 (339,593 cases).4
Encouraging the correct and consistent use of effective contraceptive methods, including barrier methods to prevent STIs, is one approach that could aid in the prevention of both unintended pregnancy and STIs. Sterilization and oral contraceptives have been the leading methods of contraception in the U.S. since 1982 and are highly effective at preventing pregnancy.5 Unfortunately, contraceptive methods with the highest efficacy for prevention of pregnancy provide no protection against STIs. Conversely, barrier contraceptive methods, when used consistently and correctly, can provide effective prevention of STIs but are associated with relatively higher pregnancy rates than other contraceptive methods.
Project PROTECT was a NIH-funded, randomized trial of two computer-based educational programs to encourage the use of dual methods of contraception for STI and pregnancy prevention. The intervention was a computer-assisted, tailored, intervention based on the transtheoretical (TTM) model of behavior change (described below). This intervention was compared to an enhanced standard care control that provided computer-based, non-tailored information and advice regarding the use of contraceptive methods. The hypotheses of this trial were: 1) the intervention will result in a greater increase in dual contraceptive use than the control; and 2) the intervention will result in greater protection against incident or recurrent cases of STIs and unintended pregnancies.
MATERIALS AND METHODS
A complete and detailed report of the methods of Project PROTECT is described elsewhere; 6 a summary of these methods is provided below. Institutional Review Board approval was obtained before the initiation of recruitment. Between October 1999 and October 2003, we screened and recruited 542 participants. To be eligible for the trial, women had to be English-speaking, between the ages of 13 and 35, sexually active with a male partner in the past 6 months and at high risk for unintended pregnancy or STI. Because age less than 25 years constitutes high risk for STIs,7 all sexually active women between the ages of 13 and 24 were eligible. Women age 25 and older were determined to be at high-risk if their history included any of the following: unintended pregnancy; history of an STI; inconsistent use of contraception; or other factors felt to place a patient at above average risk for unintended pregnancy or STI. Since a primary outcome of this study was unintended pregnancy, women were only included if they expressed the desire to avoid pregnancy for 24 months after randomization.
Participants were assigned by a computer-generated random sequence into the intervention or control groups. Randomization was stratified by study site and by baseline contraceptive group in an attempt to balance each of the site/group strata. Random assignment was separated from the executor of assignment. Although true masking was difficult in this setting, every effort was made to mask the follow-up evaluators to the treatment allocation.
INTERVENTION and CONTROL
Participants were randomized to one of two groups: the individualized intervention or the enhanced standard care condition (control). Both the intervention and control were computer-delivered, but required different levels of participation from the participants. The goal of the intervention was to encourage dual contraceptive method use. This computer program asked about current contraceptive use, and plans for future contraceptive use as well as demographic, reproductive, sexual and STI history, substance abuse, domestic violence, and levels of stress.
TTM-Tailored Expert System (Intervention)
The transtheoretical model (TTM) is a multivariable behavioral model that has been utilized in numerous tailored health promotion interventions6,8. In this study, the model conceptualizes a progression through stages of change toward the target behavior of adopting consistent dual condom and contraceptive use: precontemplation, contemplation, preparation, action and maintenance. The multimedia expert system administered a series of questions as on-screen text and by voice (via headset) and included pictures and music. Participants responded to the on-screen questionnaire using the mouse to click responses.
Expert system treatment feedback was tailored to the participant’s own readiness to change her condom and contraceptive behaviors. The intervention was designed to accelerate stage movement toward the stages Action and Maintenance for dual method use, as well as to facilitate effective recycling through the stages as participants relapsed and progressed6. The feedback was written at a 6th grade reading level to ensure comprehension. Participants in the intervention group were scheduled for three different intervention sessions over a period of eighty days (baseline, one month, and two months).
Enhanced Standard Care (Control)
Participants in the enhanced standard care group completed one computer session at baseline consisting of standard contraceptive and STI prevention information. Participants in the control group input their responses to the same on-screen questionnaire as women in the treatment group. The participant indicated on the computer which methods they would like to learn more about, and the computer provided information about those contraceptive methods. Information presented in this on-screen feedback included: the benefits of dual method use and the benefits of each individual method, risk appraisal for STIs and human immunodeficiency virus (HIV), places to obtain condoms, tips for using condoms correctly, risks and benefits of hormonal contraception, side effect information and ways of dealing with side effects, and effectiveness data for various contraceptive methods. The control group feedback was not individualized or tailored.
Upon completion of the computer program, all participants received a printed feedback report. The intervention group received tailored feedback on the computer, while the control received non-tailored standard care information and advice. All participants were given a packet of information which contained standard information on dual methods and a sample condom.
PROCEDURES
At baseline, a gynecological and contraceptive history was taken and a pelvic examination was performed. A saline preparation of vaginal discharge was done to evaluate for trichomoniasis and bacterial vaginosis. In order to increase the sensitivity for the diagnosis of trichomoniasis, we first tested vaginal pH. If the pH was above 4.5 and no trichomonads were seen on microscopic evaluation, an InPouch (Biomed Diagnostics, San Jose, CA) trichomonas culture was performed. Strand-based testing (Applified DNA Assay, Becton-Dickenson, Spanks, MD) was completed for C. trachomatis and N. gonorrhoeae, and serologic testing was performed for syphilis and HIV. A pelvic examination was performed to evaluate for pelvic tenderness; CDC minimum and supportive criteria were assessed to diagnose acute pelvic inflammatory disease (PID).9
Six and eighteen months after the computer intervention phase, the participants were contacted by telephone and asked questions about their sexual history, current and planned contraceptive use, and attitudes regarding dual contraceptive use. This survey also gathered information regarding any clinical outcomes they may have experienced. At 12 and 24 months after baseline, participants were asked to return for follow-up examinations and for completion of follow-up and background surveys. At these visits, testing for trichomoniasis, N. gonorrhoeae, and C. trachomatis, serologic test for syphilis (RPR) and a sensitive urine pregnancy test were performed. Patients were examined for signs of PID and genital herpes infection. Participants were instructed to call the study team at any time if there was any suspicion of pregnancy an STI, and were invited to the study center for an interim visit with examination and testing.
The primary behavioral outcome was self-reported use of dual methods of contraception: 1) use of hormonal contraception plus a barrier method; 2) male condoms plus female condoms; 3) condoms plus spermicide; or 4) intrauterine device or sterilization plus a barrier method. The primary biological outcome was an incident or recurrent STI and/or an unintended pregnancy.
Sample size projections were based on detection two primary endpoints: 1) a two-fold increase in dual method use from approximately 15% to 30% (in the intervention compared to control), and 2) a 50% difference in incidence of an STI or unintended pregnancy (RR = 0.5) in the intervention group compared to control). We set the two-sided hypothesis tests at a type I error rate of 2.5% and a type II error rate if 10%. We assumed that the baseline event rate for an incident unintended pregnancy or STI was at least 30% over 12 months, that the intervention would reduce these events to 15% or less (RR = 0.5), and the attrition rate would be less than 25% over two years. Under this scenario, at least 250 participants were needed on each group (500 total).
We estimated the time to event (‘survival’) curve with the Kaplan Meier nonparametric estimator using the date on which an outcome was first recorded, e.g. date of clinic visit for an STI. Event rates were compared using the log rank statistic. All comparisons among the primary outcomes were made according to the intention-to-treat principle. Additionally, we used multivariable Cox proportional hazard models to adjust for covariates. Slight imbalances in study groups remaining after randomization were accounted for in our models by using a propensity score. The propensity score was estimated using logistic regression with treatment group as the outcome and included multiple factors related to risk for pregnancy and STI, including sexual behavior, sexual history, smoking, and alcohol and substance use.
RESULTS
Of the 1,112 women screened for Project PROTECT, 916 were eligible (See Figure 1). We collected data on age, race, unintended pregnancy and STI history, and contraceptive use on all patients screened. The characteristics of the patients randomized (N=542) were similar to the patients screened eligible, but not enrolled (See Table 1). However, patients enrolled were more likely to be non-Hispanic Black (26% v. 19%) and somewhat less likely to use hormonal contraceptive methods (33% v. 38%).
Figure 1.
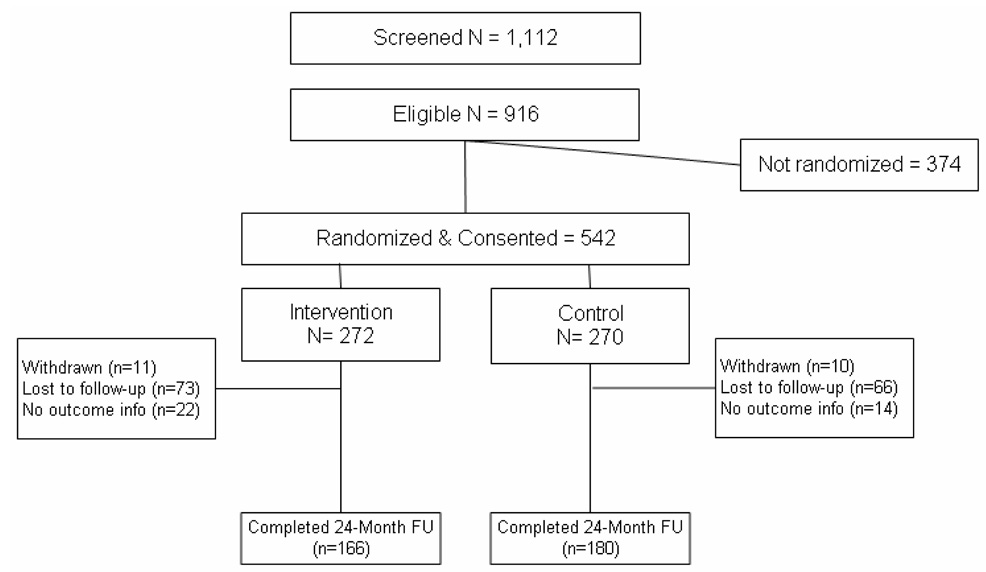
Study Flow Diagram
TABLE 1.
Baseline characteristics of study participants
| Total N = 542 | Intervention N = 272 | Control N = 270 | Eligible, not enrolled N = 374 | |
|---|---|---|---|---|
| Age | ||||
| <20 years | 155 (29) | 82 (30) | 73 (27) | 128 (34) |
| 20–24 years | 273 (50) | 140 (51) | 133(49) | 166 (44) |
| 25+ years | 114 (21) | 50 (18) | 64 (24) | 80 (21) |
| Race/ethnicity | ||||
| White, non-Hispanic | 243 (45) | 125 (46) | 118 (44) | 198 (54) |
| Black, non-Hispanic | 141 (26) | 70 (26) | 71 (26) | 70 (19) |
| Hispanic | 93 (17) | 43 (16) | 50 (19) | 59 (16) |
| Other | 65 (12) | 34 (13) | 31 (11) | 43 (12) |
| Education | ||||
| Less than high school | 133 (25) | 56 (21) | 77 (29) | N/A |
| High school/GED | 200 (37) | 105 (39) | 95 (35) | N/A |
| 2 year degree or some college | 163 (30) | 87 (32) | 76 (28) | N/A |
| 4 year degree or more | 45 (8) | 24 (9) | 21 (8) | N/A |
| Smoking status | 260 (48) | 132 (49) | 128 (48) | N/A |
| Substance use | 326 (60) | 169 (63) | 157 (58) | N/A |
| History of STI | 253 (47) | 116 (43) | 137 (51) | 160 (43) |
| History of unintended pregnancy | 263 (49) | 127 (47) | 136 (51) | 196 (53) |
| No contraceptive use | 184 (34) | 88 (32) | 96 (36) | 100 (27) |
| Hormonal contraceptive use | 177 (33) | 95 (35) | 82 (30) | 142 (38) |
| Male condoms | 159 (29) | 75 (28) | 84 (31) | 112 (30) |
| Lifetime number of sexual partners | ||||
| 1 to 2 | 70 (13) | 34 (13) | 36 (13) | N/A |
| 3 to 5 | 189 (35) | 99 (36) | 90 (33) | N/A |
| 6 to 10 | 129 (24) | 69 (25) | 60 (22) | N/A |
| 11 or more | 153 (28) | 70 (26) | 83 (31) | N/A |
| Number of sexual partners in past month | ||||
| 0 | 73 (13) | 40 (15) | 33 (12) | N/A |
| 1 | 386 (71) | 203 (75) | 183 (68) | N/A |
| 2 or more | 81 (15) | 28 (11) | 53 (20) | N/A |
| New main partner past 6 months | 139 (26) | 71 (26) | 68 (25) | N/A |
| Sex after drinking | ||||
| Never | 263 (49) | 132 (49) | 131 (49) | N/A |
| 1 to 2 times | 163 (30) | 79 (29) | 84 (31) | N/A |
| 3 or more times | 115 (21) | 61 (22) | 54 (20) | N/A |
| Forced to have sex in past year | 56 (10) | 30 (11) | 26 (10) | N/A |
Peipert. Tailored intervention to increase dual-contraceptive method use: a randomized trial to reduce unintended pregnancies and sexually transmitted infections. Am J Obstet Gynecol 2008.
The demographic, reproductive, and historical data collected from the study population at baseline stratified by intervention group is shown in Table 1. The median age was 22 years, 26% were black, and 17% were Hispanic. Over 90% were single, 25% had less than a high school education, and 48% were smokers. In terms of sexual risk factors, 49% had an unintended pregnancy, 47% had a history of a STI, and the majority had 6 or more lifetime sexual partners. Over one-third reported no contraceptive use at baseline.
Of the eligible women, 272 were randomized to the intervention group and 270 were randomized to the control group. Table 1 shows that randomization achieved similar characteristics in the two groups, yet, there were some slight imbalances. Participants in the control group were more likely to have less than a high school education (29% v. 21%, P=0.03), a history of a STI (51% v. 43%, P=0.07), and more likely to have two or more sexual partners in the past month (20% v. 11%, P=0.02).
The behavioral and biological outcomes are presented in Table 2 and illustrated in Figure 2 and Figure 3. Participants randomized to the intervention reported faster initiation of dual method use during the follow-up period (unadjusted hazard rate ratio (HRR) = 1.38, 95% confidence interval (CI) 1.00, 1.89). This effect was even more pronounced when we adjusted for baseline imbalances using the propensity score (HRRadj= 1.70, 95% CI 1.09, 2.66).
TABLE 2.
Behavioral and biological outcomes by study group (24 months of follow-up)
| Intervention N = 272 | Control N = 270 | Unadjusted HRR (95% CI) | Adjusted for propensity scorea | Adjusted for dual method | Adjusted for any dual method use & propensity score | |
|---|---|---|---|---|---|---|
| Reported any dual method use | 86 (32) | 71 (26) | 1.38 (1.00, 1.89) | 1.70 (1.09, 2.66) | — | — |
| Consistent condom use | 124 (46) | 124 (46) | 1.14 (0.89, 1.47) | 1.26 (0.88, 1.79) | — | — |
| Any STI or unintended pregnancy | 95 (35) | 93 (34) | 1.08 (0.81, 1.44) | 1.19 (0.79, 1.79) | 1.14 (0.86, 1.52) | 1.28 (0.85, 1.93) |
| Unplanned pregnancy | 60 (22) | 62 (23) | 1.00 (0.70, 1.43) | 1.17 (0.71, 1.95) | 1.04 (0.73, 1.48) | 1.22 (0.73, 2.04) |
| Any STI | 43 (16) | 44 (16) | 1.06 (0.69, 1.61) | 1.29 (0.70, 2.36) | 1.11 (0.73, 1.70) | 1.40 (0.76, 2.58) |
| Chlamydia | 27 (10) | 26 (10) | 1.13 (0.66, 1.94) | 1.31 (0.61, 2.82) | 1.19 (0.69, 2.04) | 1.42 (0.66, 3.07) |
| Gonorrhea | 12 (4) | 13 (5) | 0.96 (0.44, 2.11) | 1.83 (0.61, 5.50) | 0.97 (0.44, 2.14) | 1.86 (0.62, 5.64) |
| Trichomonas | 13 (5) | 9 (3) | 1.52 (0.65, 3.55) | 2.41 (0.72, 8.02) | 1.66 (0.71, 3.88) | 2.78 (0.83, 9.27) |
| PID | 8 (3) | 4 (1) | 2.13 (0.64, 7.07) | 1.03 (0.20, 5.19) | 2.39 (0.72, 7.96) | 1.23 (0.24, 6.23) |
Adjusts for important covariates and relevant 2-way interactions.
Peipert. Tailored intervention to increase dual-contraceptive method use: a randomized trial to reduce unintended pregnancies and sexually transmitted infections. Am J Obstet Gynecol 2008.
Figure 2.
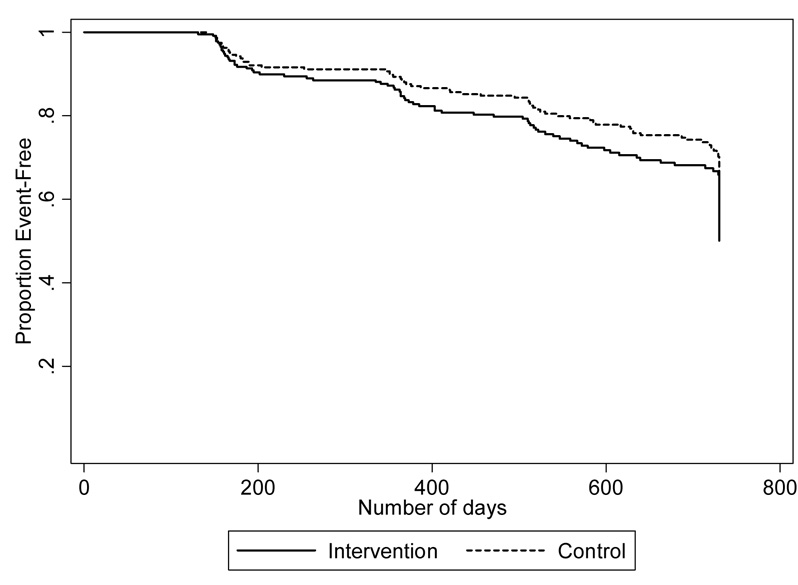
Days to initiation of dual method use by treatment group
Figure 3.
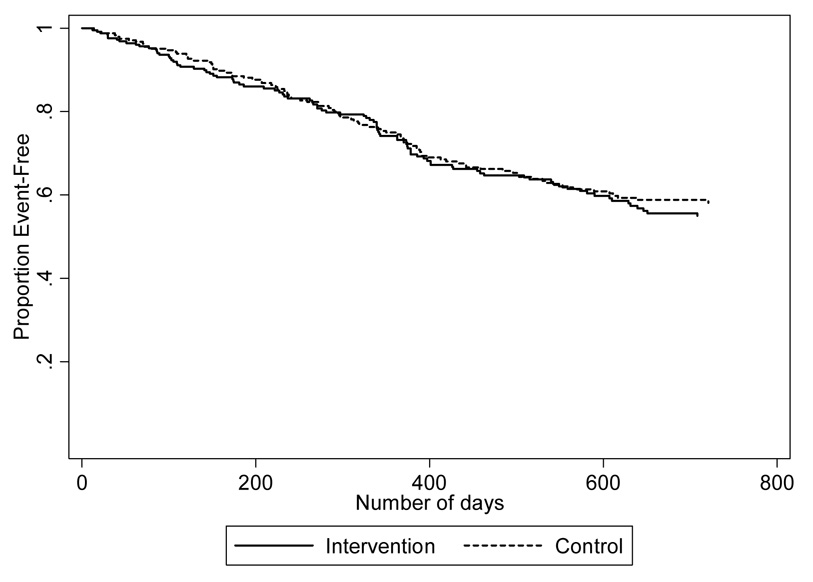
Days to first STI or pregnancy by treatment group
Reported consistent condom use was almost 30% higher in the intervention group compared to controls, but this difference was not statistically significant (HRRadj = 1.26, 95% CI 0.89, 1.79). As illustrated in Figure 3 and detailed in Table 2, there were no differences between the two groups for unintended pregnancy or incident STI. The effect of reported dual method use on more than one follow-up was not associated with time to first outcome (STI or pregnancy; HRRadj = 0.66, 95% CI 0.37, 1.18). However, women who reported dual method use on more than one follow-up questionnaire had a significantly reduced risk of pregnancy alone (HRRadj = 0.36, 95% CI 0.15, 0.91).
We evaluated correlates of reported dual method use (Table 3) as well as the biological outcomes (Table 4). Women with less than a high school education were slower to report the initiation of dual method use, while women using either hormonal contraceptive or male condoms at baseline were faster. There was no association of age, race/ethnicity, history of unintended pregnancy and number of sexual partners with initiation of dual method use. Common risk factors for STIs and unintended pregnancy emerged from this analysis (Table 4). Younger age, black race, lower education, history of STI and/or unintended pregnancy, and multiple sexual partners in the past month were all associated with an increase in the biological outcomes of STI or unintended pregnancy. Use of hormonal contraceptives and no recent sexual partner were associated with fewer incident STIs or unintended pregnancies. When we evaluated factors associated with STIs and unintended pregnancy separately, correlates for the two outcomes were different. Use of hormonal contraception was found to be highly effective at preventing unintended pregnancy (HRadj = 0.60, 95% CI 0.40, 0.90), but was not effective at preventing STIs (HRadj = 0.70, 95% CI 0.44, 1.12). History of STI was associated with an incident STI (HRadj = 2.99, 95% CI 1.87, 4.80) but was not associated with unintended pregnancy (HRadj = 1.38, 95% CI 0.96, 1.97).
TABLE 3.
Correlates of dual method use
| Crude HRR (95% CI) | Adjusted for randomization, age, race/ethnicity, education, STI, pregnancy and recent partners HRR (95% CI) | Adjusted for all main effects and randomization HRR (95% CI) | |
|---|---|---|---|
| Age (continuous) | 1.01 (0.97, 1.05) | 1.01 (0.97, 1.06) | 1.01 (0.96, 1.06) |
| Race/ethnicity | |||
| White, non-Hispanic | — | — | — |
| Black, non-Hispanic | 0.74 (0.51, 1.07) | 0.87 (0.58, 1.29) | 0.87 (0.57, 1.33) |
| Hispanic | 0.72 (0.44, 1.18) | 0.76 (0.45, 1.26) | 0.78 (0.46, 1.32) |
| Other | 0.97 (0.64, 1.47) | 1.04 (0.68, 1.59) | 1.03 (0.66, 1.59) |
| Education | |||
| Less than high school | 0.35 (0.19, 0.64) | 0.48 (0.24, 0.95) | 0.46 (0.23, 0.94) |
| High school/GED | 0.59 (0.34, 1.01) | 0.78 (0.43, 1.41) | 0.63 (0.34, 1.17) |
| 2 year degree or some college | 0.81 (0.47, 1.39) | 0.98 (0.55, 1.74) | 0.74 (0.41, 1.34) |
| 4 year degree or more | — | — | — |
| Current smoker | 0.85 (0.62, 1.16) | 0.93 (0.66, 1.31) | 1.13 (0.77, 1.65) |
| Substance use | 0.74 (0.54, 1.01) | 0.69 (0.49, 0.97) | 0.67 (0.45, 0.98) |
| History of STI | 0.61 (0.44, 0.84) | 0.70 (0.49, 1.01) | 0.70 (0.48, 1.02) |
| History of unintended pregnancy | 0.84 (0.61, 1.15) | 0.99 (0.69, 1.41) | 0.93 (0.64, 1.36) |
| Hormonal contraceptive use | 1.77 (1.29, 2.43) | 1.62 (1.17, 2.24) | 1.86 (1.26, 2.76) |
| Male condoms | 0.99 (0.91, 1.07) | 1.08 (0.76, 1.52) | 1.54 (1.02, 2.33) |
| Lifetime number of sexual partners | |||
| 1 to 2 | — | — | — |
| 3 to 5 | 1.30 (0.79, 2.13) | 1.41 (0.84, 2.36) | 1.43 (0.85, 2.40) |
| 6 to 10 | 1.08 (0.63, 1.85) | 1.18 (0.68, 2.07) | 1.30 (0.72, 2.36) |
| 11 or more | 0.85 (0.50, 1.46) | 0.98 (0.54, 1.78) | 1.03 (0.54, 1.95) |
| Number of sexual partners in past month | |||
| 0 | 0.65 (0.39, 1.10) | 0.63 (0.37, 1.08) | 0.64 (0.35, 1.20) |
| 1 | — | — | — |
| 2 or more | 0.85 (0.54, 1.33) | 0.91 (0.57, 1.44) | 0.96 (0.59, 1.55) |
| New partner past 30 days | 1.09 (0.76, 1.55) | 1.12 (0.78, 1.62) | 1.10 (0.74, 1.66) |
| Sex after drinking | |||
| Never | — | — | — |
| 1 to 2 times | 0.90 (0.62, 1.32) | 0.90 (0.61, 1.33) | 0.96 (0.61, 1.50) |
| 3 or more times | 1.45 (0.98, 2.13) | 1.38 (0.92, 2.06) | 1.55 (0.97, 2.48) |
| Forced to have sex in past year | 1.00 (0.98, 1.02) | 1.00 (0.98, 1.03) | 1.02 (1.00, 1.05) |
Peipert. Tailored intervention to increase dual-contraceptive method use: a randomized trial to reduce unintended pregnancies and sexually transmitted infections. Am J Obstet Gynecol 2008.
TABLE 4.
Correlates of biological outcomes of STI and/or unintended pregnancy
| Crude HRR (95% CI) | Adjusted for randomization, age, race/ethnicity, education, STI, pregnancy and recent partners HRR (95% CI) | Adjusted for all main effects and randomization HRR (95% CI) | |
|---|---|---|---|
| Age (continuous) | 0.96 (0.92, 1.00) | 0.93 (0.89, 0.97) | 0.93 (0.89, 0.97) |
| Race/ethnicity | |||
| White, non-Hispanic | — | — | — |
| Black, non-Hispanic | 1.92 (1.42, 2.60) | 1.41 (1.01, 1.97) | 1.44 (1.02, 2.02) |
| Hispanic | 1.40 (0.91, 2.16) | 1.34 (0.88, 2.06) | 1.29 (0.80, 2.07) |
| Other | 1.10 (0.74, 1.63) | 0.89 (0.60, 1.32) | 0.85 (0.57, 1.28) |
| Education | |||
| Less than high school | 4.56 (2.05, 9.70) | 2.55 (1.15, 5.67) | 2.01 (0.88, 4.57) |
| High school/GED | 3.07 (1.42, 6.64) | 1.87 (0.85, 4.11) | 1.52 (0.68, 3.40) |
| 2 year degree or some college | 1.35 (0.60, 3.08) | 1.03 (0.45, 2.36) | 0.91 (0.39, 2.10) |
| 4 year degree or more | — | — | — |
| Current smoker | 1.14 (0.85, 1.51) | 1.08 (0.79, 1.46) | 1.13 (0.80, 1.58) |
| Substance use | 1.08 (0.81, 1.45) | 1.04 (0.76, 1.43) | 1.07 (0.76, 1.55) |
| History of STI | 2.02 (1.50, 2.71) | 1.71 (1.23, 2.38) | 1.81 (1.28, 2.57) |
| History of unintended pregnancy | 2.02 (1.50, 2.72) | 1.82 (1.31, 2.52) | 2.00 (1.42, 2.80) |
| Hormonal contraceptive use | 0.62 (0.45, 0.86) | 0.65 (0.46, 0.91) | 0.56 (0.39, 0.81) |
| Male condoms | 1.01 (0.99, 1.03) | 0.92 (0.65, 1.29) | 0.80 (0.55, 1.16) |
| Lifetime number of sexual partners | |||
| 1 to 2 | — | — | — |
| 3 to 5 | 1.06 (0.67, 1.67) | 1.16 (0.73, 1.85) | 1.02 (0.63, 1.65) |
| 6 to 10 | 1.08 (0.66, 1.76) | 1.10 (0.67, 1.82) | 0.92 (0.54, 1.58) |
| 11 or more | 1.03 (0.63, 1.66) | 0.80 (0.48, 1.34) | 0.65 (0.37, 1.12) |
| Number of sexual partners in past month | |||
| 0 | 0.67 (0.41, 1.08) | 0.60 (0.36, 1.00) | 0.53 (0.30, 0.91) |
| 1 | — | — | — |
| 2 or more | 1.59 (1.10, 2.30) | 1.45 (0.99, 2.13) | 1.56 (1.05, 2.32) |
| New partner past 30 days | 1.12 (0.81, 1.55) | 1.04 (0.75, 1.45) | 0.92 (0.63, 1.32) |
| Sex after drinking | |||
| Never | — | — | — |
| 1 to 2 times | 1.01 (0.72, 1.40) | 1.09 (0.77, 1.54) | 0.87 (0.58, 1.30) |
| 3 or more times | 1.25 (0.86, 1.80) | 1.40 (0.96, 2.05) | 1.22 (0.80, 1.86) |
| Forced to have sex in past year | 1.01 (0.99, 1.03) | 1.00 (0.98, 1.02) | 0.99 (0.93, 1.06) |
Peipert. Tailored intervention to increase dual-contraceptive method use: a randomized trial to reduce unintended pregnancies and sexually transmitted infections. Am J Obstet Gynecol 2008.
COMMENT
The intervention based on the transtheoretical model of behavior change resulted in an increase in our primary behavioral outcome, self-reported dual method contraceptive use, compared to the control. However, there were no differences in the number of incident STIs or unintended pregnancies. It is possible that the intervention was more effective at the reported initiation of dual method use, but the duration of use and adherence were not sustained long enough to translate into a reduction in STIs and unintended pregnancy. This concept is supported by our analysis evaluating repeated reports of dual method use; women reporting dual method use at more than one follow-up visit were at reduced risk of incident STIs or unintended pregnancies.
We found that lower educational level, African-American race, history of STI or unintended pregnancy, and two or more partners in the past 30 days were correlated with our biological outcomes of unintended pregnancy and incident STI. Having no partners in the past 30 days and the use of hormonal contraception were protective. Risk factors for STIs differed from risk factors for unintended pregnancy. As expected, we found that the use of hormonal contraception was effective at preventing unintended pregnancy, but was not effective at preventing STIs.
The concept of “dual methods” of contraception involves the use of both a method that is highly effective at pregnancy prevention and a method that is highly effective at prevention of STIs. The most common combination of methods is pills and condoms.10 Existing data indicate that the use of dual methods is not the norm. The National Survey on Family Growth (NSFG) found that only 2.6% of the 38,302 women in the 1995 sample were using the oral contraceptive pill and the condom together for protection.11 The Youth Risk Behavior Survey found that only 6.6% of women between the ages of 14 and 22 were using dual methods of contraception.12 Although 4.1% of all women were using both the male condom and oral contraceptives, the prevalence was highest among younger women (11–15% for those under 25 years).13
Data from the NSFG evaluating changes in contraceptive use between 1995 and 2002 are encouraging. According to Santelli and colleagues, 7.5% of women in the 15–19 year age group used a hormonal method and condom in 1995. This percentage increased to 17.9% in 2002.14 The use of two or more methods increased from 12% in 1995 to 33% in 2002 among 15–17 year-olds. An increase was also noted in 18–19 year-olds with 11% using two or more methods in 1995 and 22% in 2002.10 The authors conclude that most of the decline in adolescent pregnancy is attributable to improved contraceptive use.14 Whether increased dual method use will result in a population impact in terms of STI prevention remains to be seen.
Previous studies have found tailored expert systems comparable to this one to increase condom use compared to generic standard care interventions in adolescent females in family planning clinic settings15 and in adult males and females recruited from community-based settings.16 Both studies relied on self-reported consistent condom use as primary outcomes. These study results suggest that self-reported contraceptive behaviors and incident STIs or unintended pregnancies may be less closely related than hypothesized.
There are several alternative explanations for our findings. It is possible that increased patient contact in the intervention group was the primary reason for the increase in reported dual method use. The intervention had three monthly computer-based sessions, while the control had only a single computer-based session. This might result in a true increased rate of dual method use or a reporting bias: participants receiving the message that dual contraceptive method use is the preferred behavior may be more likely to report the behavior.
Our study has a number of strengths and limitations that should be considered. As a randomized trial, we can assess the effectiveness of our intervention in a high-risk group of women. We are able to determine incident STIs and unplanned pregnancy, as oppose to cross-sectional and retrospective studies that cannot easily address temporal sequence. One limitation of our report is that despite our a priori sample size calculation and recruiting over 500 women, our power to address some outcomes is limited. Approximately 28–31% of participants reported male condom use pre-intervention. This increased to over 40% post-intervention in both groups. Thus, our power to assess differences is limited by the increased condom use in our control arm.
In summary, STIs and unintended pregnancy are a tremendous burden on young women and the healthcare system. While we did not see a sustained biological effect of dual method use in our trial, the intervention resulted in more women reporting initiation of dual contraceptive method use. The Transtheoretical model may be a useful used in conjunction with computer-based technology to assist young women in the progression through the stages of behavior change. Future trials should focus on methods to encourage consistent use of dual methods to prevent both unintended pregnancy and STIs.
ACKNOWLEDGEMENTS
The authors wish to acknowledge Joseph Hogan, ScD from Center for Statistical Sciences, Brown University, Providence, Rhode Island for his early contributions to the study design and statistical analysis.
Supported by grants RO1-HD36663, Stage-Matched Intervention to Increase Dual Method Use, and K24 HD01298, Midcareer Investigator Award in Women’s Health Research from the National Institutes of Child Health and Human Development.
Footnotes
This paper was presented at the Annual Meeting of the Infectious Diseases Society for Obstetrics and Gynecology, Boston, MA, August 9-11, 2007 and the Annual Scientific Session of the St. Louis Gynecological Society, St. Louis, MO on April 17, 2007.
CONDENSATION
A tailored, computer-based intervention resulted in a 70% increase in reported dual method contraceptive use in women at high-risk for STIs and unintended pregnancy.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Population Council. Increase in effective contraceptive use can reduce abortion rate. Momentum Population Council. 2001 [Google Scholar]
- 2.Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspect. 1998;30:24–29. 46. [PubMed] [Google Scholar]
- 3.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance, 2005. Atlanta, GA: US Department of Health and Human Services; 2006. [Google Scholar]
- 5.Moodley P, Connolly C, Sturm AW. Interrelationships among human immunodeficiency virus type 1 infection, bacterial vaginosis, trichomoniasis, and the presence of yeasts. J Infect Dis. 2002;185:69–73. doi: 10.1086/338027. [DOI] [PubMed] [Google Scholar]
- 6.Peipert JF, Redding CA, Blume J, et al. Design of a Stage-Matched Intervention Trial to Increase Dual Method Contraceptive Use (Project PROTECT) Contemporary Clinical Trials. 2007;28:626–637. doi: 10.1016/j.cct.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 7.Peipert JF. Clinical practice. Genital chlamydial infections. N Engl J Med. 2003;349:2424–2430. doi: 10.1056/NEJMcp030542. [DOI] [PubMed] [Google Scholar]
- 8.Prochaska JO, Velicer WF, Redding CA, et al. Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer and receive regular mammograms. Prev Med. 2005;41:406–416. doi: 10.1016/j.ypmed.2004.09.050. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Sexually Transmitted Disease Treatment Guidelines. MMWR. 2006;55(RR11):58–63. [Google Scholar]
- 10.Santelli JS, Morrow B, Anderson JE, Lindberg LD. Contraceptive use and pregnancy risk among U.S. high school students, 1991–2003. Perspect Sex Reprod Health. 2006;38:106–111. doi: 10.1363/psrh.38.106.06. [DOI] [PubMed] [Google Scholar]
- 11.Piccinino LJ, Mosher WD. Trends in contraceptive use in the United States: 1982–1995. Fam Plann Perspect. 1998;30:4–10. 46. [PubMed] [Google Scholar]
- 12.Santelli JS, Warren CW, Lowry R, et al. The use of condoms with other contraceptive methods among young men and women. Fam Plann Perspect. 1997;29:261–267. [PubMed] [Google Scholar]
- 13.Mosher WD, Martinez GM, Chandra A, Abma JC, Willson SJ. Use of contraception and use of family planning services in the United States: 1982–2002. Adv Data. 2004:1–36. [PubMed] [Google Scholar]
- 14.Santelli JS, Lindberg LD, Finer LB, Singh S. Explaining recent declines in adolescent pregnancy in the United States: the contribution of abstinence and improved contraceptive use. Am J Public Health. 2007;97:150–156. doi: 10.2105/AJPH.2006.089169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Redding CA, Prochaska JO, Rossi JS, et al. Effectiveness of a randomized clinical trial of stage-matched interventions targeting condom use and smoking in young urban females. Ann Behav Med. 2002;24:S061. [Google Scholar]
- 16.Redding CA, Morokoff PJ, Rossi JS, et al. Effectiveness of a computer-delivered TTM-tailored intervention at increasing condom use in at-risk heterosexual adults: RI Project Respect. Ann Behav Med. 2004;27:S113. [Google Scholar]


