Abstract
Introduction
The Italian Society of Transfusion Medicine and Immunohaematology (SIMTI) carried out a survey on the current use of anti-D immunoprophylaxis (IP) in Italy, on its ways of use and on the impact that it has had on decreasing haemolytic disease of the newborn (HDN), due to maternal-foetal incompatibility for the D antigen.
Materials and methods
The survey was carried out using a questionnaire prepared by the Working Group established for this purpose by the SIMTI. The questions were divided into five groups: the ways of carrying out IP, evaluation of foetal-maternal haemorrhage, serological tests after IP, the current incidence of HDN, and data on exchange transfusions.
Results
Data were obtained from 69 Transfusion Services (TS). Four of these give IP antenatally, whereas in the remaining cases IP is given after birth. Almost all the TS evaluate the amount of foetal-maternal haemorrhage in order to give additional doses of anti-D IgG, with the most widely used method being the Kleihauer-Betke test. Data were collected from 176,010 pregnancies: 18,639 were D-negative women, of whom 18,440 were not immunised. There were 136 cases of HDN with anti-D antibodies, and 39 of these required exchange transfusions (ET). Furthermore, there were 1,535 pregnant women with anti-A and/or anti-B IgG, which were clinically significant in 83 and required ET in 37. Finally, 40 women had antibodies, directly related to the pregnancy, against antigens other than D (in eight of these cases ET was necessary).
Conclusions
The survey carried out by SIMTI was able to give a sufficiently full and accurate picture of current Italian practices concerning the use and ways of use of anti-D IP in pregnancy and the puerperum, as well as the incidence and characteristics of HDN. Furthermore, this survey was the basis for guidelines on the management of HDN, produced by SIMTI in collaboration with the Italian Society of Obstetricians and Gynaecologists.
Keywords: anti-D immunoprophylaxis, haemolytic disease of the newborn, anti-D immunoglobulins
Introduction
It has been very rare in Medicine that, in the span of little more than 20 years, the aetiology of a mysterious and unknown disease is discovered, its immunological pathogenesis determined, an efficient therapy (at least for the more severe and frequent cases) is introduced and, above all, preventive treatment is so effective as to decrease the number of intrauterine foetal deaths by more than 100-fold and the incidence of maternal alloimmunisation by more than 50-fold1.. This disease, previously known by a wide range of names (familial neonatal jaundice, severe neonatal jaundice, foetal erythroblastosis, neonatal erythaemia, etc.), is haemolytic disease of the newborn (HDN) due to or materno-foetal incompatibility for the D antigen (Rho RH1) of the Rh system. The period in which all these advances occurred started with the publication of the famous study by Levine and Stetson in 19392, the real date of the discovery of the Rh system3, and extended to the proposed use of anti-D antibodies in order to prevent a mother, carrying a D-positive foetus or having given birth to one, from starting to produce specific antibodies, that is, from becoming immunised.
This proposal was first made orally in 1960 by Finn4 and then formally, independently and almost contemporaneously by researchers from both England5 and Noth America6 in the early 1960s. As known, immunoprophylaxis (IP) is achieved by injecting the puerpera (postnatal prophylaxis) or the pregnant woman (antenatal prophylaxis) with anti-D IgG at doses ranging from 100 μg (500 UI), to 200 μg (1,000 UI), up to 300 μg (1,500UI).
The numbers show that HDN due to materno-foetal incompatibility for D (now known as Rh HDN) once had all the characteristics of a social disease. Approximately 1.5 to 2 pregnant women in 200 (in direct relation to the incidence of D-negative subjects in the area considered), had anti-D antibodies and were, therefore, able to cause the disease in their D-incompatible children7. For example, in Italy, up to the 1960s, each year about 7,000 subjects were affected by Rh HDN, with about 1,500 deaths each year (including, of course, in utero deaths)8.
There is a lack of complete world data on the incidence and severity of the disease before the introduction of prophylaxis. However, just as one example, Mollison and Walker reported that, in England in the early 1950s, there were about 1,000 deaths each year due to Rh HDN9.
Precisely in order to obtain accurate data on the current use of anti-D IP in Italy, on the way it is used and on the impact that it has had on the decrease of Rh HDN, in autumn 2004, on the occasion of the XXXVI National Congress of Transfusion Medicine (Florence, 30/9/04 – 3/10/04), the Italian Society of Transfusion Medicine and Immunohaematology (SIMTI) started a survey aimed at collecting this information.
Materials and methods
The survey was carried out using a questionnaire prepared by a Working Group established for this purpose by the Society. The members of the Working Group are reported at the end of this paper.
The questionnaire comprised 24 questions, with various subquestions, divided into five groups: ways of providing IP, evaluation of foeto-maternal haemorrhage (FMH), serological tests after IP; current incidence of HDN, and data on exchange transfusions (ET).
The questionnaire was sent, via the online SIMTI website, to Italian Transfusion Services (TS). The ZLB company (Bioplasma Italy, Milan, Italy), which was interested in the project, took care of encouraging responses. The computer management of the project was entrusted to Maya Tecnologie (Verona, Italy).
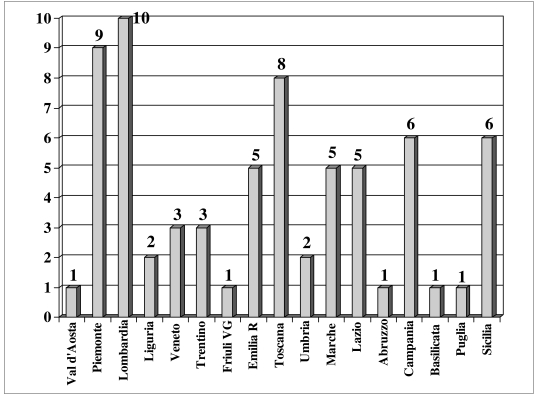
Sixty-six TS responded to all or most of the questions, whereas three others answered only those questions concerning IP. The geographical distribution of the 69 TS that provided useful information is illustrated in figure 1.
Figure 1.
Regional distribution of the Transfusion Services participating in the survey.
Results
Methods of carrying out IP
The results revealed that only four TS (Ospedale Maggiore in Bologna, Ospedali Galliera in Genoa, and the TS in Ragusa and San Cataldo in the province of Caltanissetta) practice antenatal prophylaxis, which is carried out between the 25th and 28th week of pregnancy using a dose of 250 μg (1,250 UI), except for the Ospedali Galliera, in which the dose used was 300 μg (1,500 UI).
Almost all the TS systematically carry out post-natal IP, both in “classical” cases of a D-negative puerpera who gives birth to a D-positive or weak-D neonate (or foetus) (62/69; 90%), and in cases in which it is not been possible to carry out D typing of the neonate (65/69; 94%). Furthermore, 71% of the TS (49 structures) allow for IP of a D-negative mother even if more than 72 hours have passed since the birth of a D-positive neonate.
Practically all the TS (only one TS did not respond) provide IP in the antenatal period in particular situations: spontaneous abortions, therapeutic abortions, ectopic pregnancies, intrauterine death of a foetus, as well as in cases of threatened abortion, invasive obstetric manoeuvres, direct trauma to the pregnant abdomen, haemorrhages during pregnancy or suspected FMH during the gestation.
The prophylactic doses of anti-D IgG used during pregnancy or after delivery range from 200 μg (1,000 UI), to 250 μg or 300 μg.All the data concerning IP are summarised in table I.
Table I.
Anti-D immunoprophylaxis (69 responses)
| Question | Yes (%) | No (%) | No answer (%) |
|---|---|---|---|
| Does your TS routinely use antenatal IP? | 4 (6%) | 62 (90%) | 3 (4%) |
| If so, at what dose and in which week of gestation? | 3 use 250μg (1,250 UI) and 1 uses 300 μg (1,500 UI) all between the 25th and 28th week | ||
| Does your TS use antenatal IP in particular situations (invasive manoeuvres, abortions, threatened abortions, abdominal trauma, etc.)? | 68 (98.5%) | - | 1 (1.5%) |
| If so, what doses are used? | 200μg (6 TS) -250μg (44 TS) - 300μg (17 TS) 1 TS did not answer | ||
| Is post-natal IP carried out routinely in D-negative puerperal women who give birth to a D-positive neonate? | 66 (96%) | - | 3 (4%) |
| If so, what doses are used? | 200 μg (6 TS) -250 μg (34 TS)- 300 μg (19 TS) 3 TS did not answer | ||
| If it not possible to administer the IP within 72 h of the delivery, is it given anyway? | 49 (71%) | 14 (20%) | 6 (9%) |
| If it is not possible to D type the neonate, is IP carried out anyway? | 65 (94%) | 2 (3%) | 2 (3%) |
| Is a weak-D (formerly Du) neonate considered as D+ and the D-negative puerpera given IP? | 65 (94%) | 2 (3%) | 2 (3%) |
| Is the efficacy of the IP checked a posteriori? | 35 (51%) | 31 (45%) | 3 (4%) |
| If so, after how long? | 9 TS after 4 months - 26 TS after 6 months | ||
A second aspect investigated in this part of the survey concerned the red cell immunohaematological tests carried out on the pregnant or puerperal women and their partners. The responses related to these issues are summarised in table II, which shows that the vast majority of the TS (65/ 69, 94%) searched for weak-D and, very interestingly, 43.5% of the TS (30/69) were able to identify the main D antigen variants, using specific, commercially available reagents (in most cases the Id Typing partial RhD from DiaMed [DiaMed Italia, Vedano al Lambro, MI, Italy] or, less frequently, the RH (D) Epitope Kit from Immucor [Immucor Italia, Noverasco d'Opera, MI, Italy]).
Table II.
Immunohaematological tests (69 responses)
| Question | Yes (%) | No (%) | No answer (%) |
|---|---|---|---|
| Does your TS systematically search for weak-D in pregnant and puerperal women? | 66 (96%) | 3 (4%) | - |
| Does your TS search for variants of the D antigen? | 30 (43.5%) | 36 (52%) | 3 (4%) |
| Does your TS define the D compatibility of a woman's partner before antenatal IP (whether given routinely or because of particular events)? | 7 (10%) | 38 (55%) | 24 (35%) |
These reagents identify the following epitopes: DII, DIII,DIVa, DIVb, DV, DVI, DVII, DFR, DBT,andRoHar).
Only seven of the 69 TS determine the D antigen status of the partner before starting antenatal IP (whether as routine practice or because of the previously described situations occurring during a pregnancy).
Evaluation of FMH
Table III reports the timing of the investigations of FMH, whereas table IV reports the methods used for these investigations. Almost all the TS that returned the questionnaire (n=67; 97%) evaluated the amount of FMH in order to decide whether or not to give additional doses of anti-D IgG, in the case of substantial haemorrhage.Asked to indicate whether this investigation is carried out only in the post-partum period, 30 TS (44%) did not respond. Fourteen TS (20%) also evaluate FMH during pregnancies in which events that could cause haemorrhage occur and four (6%) evaluate possible FMH systematically, in a given period of gestation (two TS between the 25th and the 28th week and two after the 28th week of gestation).
Table III.
Evaluation of FMH (69 responses)
| Question | Yes (%) | No (%) | No answer or not detailed (%) |
|---|---|---|---|
| Does your TS evaluate the amount of FMH in order to decide the dose of anti-D IgG to give for IP? | 67 (97%) | 1 (1,5%) | 1 (1,5%) |
| Is this evaluation only made after delivery? | 25 (36%) | 14 (20%) | 30 (44%) |
| Or is this evaluation also carried out during a pregnancy if events that could cause FMH occur? | 14 (20%) | 25 (36%) | 30 (44%) |
| Or is this evaluation carried out systematically during a specific week of gestation? | 4 (6%) | - | 65 (94%) |
| If so, in which week of gestation? | 2 TS between the 25th and 29th week; 2 TS after the 28th week | ||
Table IV.
Methods for evaluating FMH (67 responses)
| Method | Number and percentage of TS |
|---|---|
| Acid elution (Kleihauer-Betke test) | 14 (21%) |
| Weak-D test on maternal blood under microscopy | 7 (10.5%) |
| Cytofluorimetry | 6 (9%) |
| Anti-D antibody consumption in gel-agglutination | 5 (7.5%) |
| Anti-D antibody consumption in gel-agglutination and cytofluorimetry | 2 (3%) |
| Kleihauer-Betke test + rosetting test | 1 (1.5%) |
| Kleihauer-Betke test + weak-D test | 1 (1.5%) |
| Not stated | 31 (46%) |
As far as concerns the technique used, taking into account that as many as 31 TS (46%) did not answer this question, it can be seen from table IV that the most widely used method is the acid elution test, universally known as the Kleihauer-Betke test10, used alone (14 TS) or together with other methods (2 TS) by 24% of the structures.
The second most frequently used investigation is the test for weak-D (formerly Du) in the mother's blood, with test results read under the microscope11; this investigation is used alone (7 TS) or together with the Kleihauer-Betke test (1 TS) by 12% of the TS. Cytofluorimetric studies12 are also used with a certain frequency: six TS use this technique alone and two use it in association with a gel agglutination test of the consumption of anti-D antibodies (overall, 12% of the TS).
This last test, which is the most recently introduced into immunohaematological practice13, is used by seven TS: five (7.5%) of which have adopted it as the only method and two (3%) of which use it together with or alternatively to cytofluorimetry. Finally, one TS (1.5%) stated that it also uses the rosetting test14 as an alternative to the Kleihauer-Betke test, despite this former being a very complex technique.
Questioned on the existence of internal guidelines on the appropriate management of HDN and correct transfusional treatment of the foetus or neonate affected by the disease, 32 TS (46%) replied that they have such guidelines, whereas 33 (48%) do not have guidelines and four (6%) TS did not reply to the question.
Serological tests after IP
Thirty-five (51%) of the TS regularly check the efficacy of the prophylaxis 4 to 6 months after administering it.
Current incidence of HDN
Table V reports the total number of pregnancies followed (n=176,010). The table also presents the number of D-negative pregnant (or puerperal) women studied (n=18,639) and that of non-immunised D-negative pregnant women(n=18,440).
Table V.
Number of evaluated pregnancies and immunised subjects
| Question | Number | TS that supplied data |
|---|---|---|
| Pregnancies considered | 176,010 | 63 |
| RhD negative pregnancies | 18,639 | 53 |
| RhD negative pregnancies without anti-D sensitisation | 18,461 | 43 |
| Pregnancies showing anti-D sensitisation (at delivery) | 59 | 53 |
| Pregnancies showing anti-D sensitisation during the pregnancy | 119 | 54 |
| Total anti-D sensitised women | 178 | - |
| Of whom, anti-D sensitised women despite IP | 12 | 54 |
| Pregnant women with anti A and/or anti-B IgG antibodies | 1,535 | 44 |
| Pregnant women with direct antibodies against non-D/non-ABO antigens related directly to the pregnancy | 40 | 59 |
| Specificity of the antibodies to other antigens related directly to the pregnancy | anti-c 8 | 9 |
| anti-E 4 | ||
| anti-E+c 1 | ||
| anti-E+S 1 | ||
| anti-C 1 | ||
| anti-K1 3 | ||
| anti-K1+Jka 1 | ||
| anti-Jka 2 | ||
| anti-Fya 1 | ||
| anti-Jsa 1 |
One hundred and seventy-eight women had anti-D antibodies: more precisely, 59 cases of anti-D immunisation were found at the time of delivery, while in the other 119 cases, the anti-D sensitisation had been detected during periodic controls, carried out systematically during the pregnancy.
It is of particular interest that the immunisation in 12 of these 178 cases occurred despite the fact that IP had been given to the pregnant woman on the occasion of a previous D-incompatible delivery. Only three of the TS were able to indicate the reason for the lack of the protective action of the IP: in two cases this was due to insufficient doses (because of a mistaken evaluation of FMH) and in one case because of delayed administration of the IP. The other nine TS, in which this problem occurred, stated that they did not know the reason.
There were 1,535 pregnant women who had anti-A and/ or anti-B IgG antibodies in their serum, but these were reported as being of significant clinical relevance in only 83 cases.
Fifty-five women had antibodies to antigens other than D. Telephone calls were made to obtain further information on these cases: only in 40 cases was the sensitisation directly related to a pregnancy.
Data on ET
Table VI shows the reported numbers of cases of HDN (due to anti-D immunisation, ABO incompatibility or antibodies to other blood group antigens), as well as the number of ET carried out.
Table VI.
Number of cases of HDN and ET
| HDN | Number |
|---|---|
| HDN due to anti-D sensitisation | 136 |
| HDN due to ABO incompatibility | 1,535 |
| HDN due to antibodies with other specificities | 40 |
| ET for HDN due to anti-D sensitisation | 39 |
| ET for HDN due to ABO incompatibility | 37 |
| ET for HDN due to other types of antibodies | 8 |
Discussion
The first point that should be made about this survey is that, unfortunately, a relatively low number of TS participated: 69, of which three only in part, of the more than 300 contacted are certainly few and, furthermore, many of the most important TS, with undoubtedly large populations, did not respond.
The main aim of the survey was, however, fulfilled, with the collected data showing that IP, at least post-natal IP, is carried out in all the structures contacted.
It is equally important to note that, while only four of the 69 TS systematically use antenatal IP, all the Services (more exactly, 68 out of 69, but one TS did not answer the question) give prophylaxis during a pregnancy if there is a possibility of foetal blood entering the maternal circulation (invasive obstetric manoeuvres, abortions or threatened abortions, trauma to the pregnant abdomen and other similar situations).
The vast majority of the TS carry out post-natal IP in any case, even when it has not been possible to ascertain the D status of the neonate or when the “classical” 72 hours after delivery have been exceeded. The weak-D neonate, despite the low immunogenicity of this phenotype, is considered by 94% of the TS as a D-positive subject and the mother is, therefore, given prophylaxis. Finally, about half (51%) of the TS regularly check the efficacy of the prophylaxis after 4–6 months: this is not a high percentage, but the difficulties in getting patients to return for follow-up controls are well-known.
In the part of the questionnaire dedicated to immunohaematological investigations of the pregnant woman, the neonate and the woman's partner, the most notable fact is that almost half of the TS (more exactly, 30 out of 69; 44%) are able to determine the D variants, carrying out these investigations when needed. This success is directly related to the possibility of using specific, commercially available reagents for the single epitopes making up the whole antigenic D complex.
With regards to FMH, almost all the TS (n=67; 97%) stated that they carried out investigations to evaluate the amount of any haemorrhage, in order to use the appropriate dose of anti-D IgG. The most widely used investigation was the Kleihauer-Betke method of acid eluation, alone or together with other techniques (the rosetting test or weak-D test). A not irrelevant number of TS used much more complex techniques, such as cytofluorimetry (n=8; 12%), the weak-D test or gel agglutination technology to measure antibody consumption. Moreover, it should be noted that 31 TS (46%) did not answer the question on the technique used to determine the amount of FMH.
The last sections of the questionnaire were designed to collect information on the number of pregnancies, the number of D-negative pregnant women, the incidence of anti-D immunisation and the number of cases of HDN occurring, in particular those caused by anti-D antibodies alone or together with other specificities, but also those due to ABO incompatibility or to antibodies against other blood group antigens.
The data acquired, concerning pregnancies followed, do give a picture of the Italian situation, since they were related to just under one quarter of all pregnancies and births occurring in Italy in the 2 years considered (2003–2004); in fact, in these 2 years there were 807,000 births (544,000 in 2003 and 263,000 in 2004).
The percentage of D-negative pregnant or puerperal women (18,639 out of 176,010; 10.5%) is definitely lower than that expected for Caucasian women, among whom the incidence is between 13 and 15%.
However, given the considerable immigration that has taken place recently in Italy, it is more than probable that some of the pregnant women studied were from countries outside Europe, in which the frequency of D-negative subjects is much lower.
An important finding is that 99% of the D-negative pregnant women were not sensitised. Overall, anti-D antibodies were found in 178 pregnant women: the lack of responses to the pertinent questions on the real incidence of maternal anti-D sensitisation prevents definitive, numerical estimates from being made. The data that are available (178 women immunised during pregnancy or at delivery) corresponds to a sensitisation rate of 0.96% among the D-negative pregnant women.
More than a few women were immunised despite having undergone IP on the occasion of previous pregnancies: the exact number was 12. Only in three cases were the TS able to report the possible cause of the lack of a protective effect.
There were 136 cases of HDN due to anti-D immunisation which, in most cases, were of relatively modest clinical relevance, given that ET was necessary in only 39 of these cases (28.7%): in the remaining cases, less aggressive management, such as phototherapy or microtransfusions, was sufficient to correct the hyperbilirubinaemia or anaemia.
Even taking into consideration the lower incidence of HDN due to anti-D in Italy in the era prior to prophylaxis, that is, 1.5 cases every 200 pregnancies, there should have been 6,052 cases. There has, therefore, been a decrease of about 98% in this disease, which is an extremely significant and reassuring result, in line with the changes in other countries15.
As might have expected, perhaps directly related to questions that could be equivocal (even if, apparently, corrected formulated), the answers concerning HDN due to ABO incompatibility created some confusion. In fact, the presence of a high titre of anti-A and/or anti-B IgG in the maternal serum and a positive direct antiglobulin test (from 1+ up to 2–3+) on neonatal red blood cells is commonly indicated as ABO HDN, even without serious consequences for the neonate, alongside the form which, in contrast, is associated with important clinical symptoms, requiring intensive phototherapy and, in the most severe cases, ET. In fact, the number of pregnant women found to have class IgG anti-A and/or anti-B antibodies was very high: 1,535 cases were reported. However, there were few cases of HDN due to ABO incompatibility (in total, 83) and the majority of these cases were of limited clinical relevance, given that ET had to be used in only 37 cases.
Particular note should be made of the 73 cases in which irregular antibodies to antigens of blood group systems other than D were found in the serum of pregnant women. This is a substantial number, considering that these cases represent more than 40% of the cases of anti-D immunisation detected.
Furthermore, from investigations conducted a posteriori, it emerged, as reported in the results, that 40 of these cases were directly related to the pregnancy. In the remaining cases the pregnant women had become immunised through previous transfusion therapy (or previous pregnancies with a different partner) and the foetus or neonate did not have the antigen involved.
Only in 23 cases were data related to the antibody specificities supplied; as can be seen in table VI, there was a wide range of specificities, all of which were relatively common, except a case of anti-Jsa (anti-Sutter or anti-K6) immunisation, which caused clinically important HDN, such as to require ET. In this respect, it can be stated that HDN due to antibodies other than anti-D was clinically important in eight cases, in which it was necessary to use ET therapy.
In conclusion, although limited by the relatively low number of TS that participated actively in the initiative, supplying data that could be interpreted and evaluated, the survey carried out by the “Research and Development” Area of SIMTI was able to give a sufficiently broad and correct picture of the current Italian use and ways of use of anti-D IP in pregnant and puerperal women, as well as the incidence and characteristics of the cases of HDN that do occur.
Furthermore, this survey formed the information base and stimulus for the production, by SIMTI in collaboration with the Italian Society of Obstetricians and Gynaecologists (SIGO), of recommendations for the management of haemolytic disease of the newborn16. These recommendations are fruit of an important professional collaboration and agreement on a subject of great medical relevance.
Acknowledgments
We thank all the Transfusion Services, listed below, which participated in the survey:
Ancona, Aosta, Asti, Battipaglia (SA), Biella, Ospedale Maggiore Bologna, Bolzano, Brescia, Brunico (BZ), Busto Arsizio (VA), Caltanissetta, Camposampiero (PD), Casale Monferrato (AL), Ospedale Cannizzaro Catania, Cesena (FO), Città di Castello (PG), Civitanova Marche (MC), Civitavecchia (Rome), Domodossola (VB), Eboli (SA), Empoli (FI), Faenza (RA), Policlinico Careggi Florence, S Giovanni di Dio Hospital Florence, Foligno (PG), Galatina (LE), Gallarate (VA), Ospedale Galliera Genoa, Ivrea (TO), Jesi (AN), Lucca, Macerata, Mantova, Melzo (MI), Messina, Modena, Mondovì (CN), Monza (MI), Monaldi Hospital Naples, Ostia (Rome), Palermo, Polyclinic Palmanova (UD), Pesaro, Pontedera (PI), Potenza, Prato, Ragusa, Reggio Emilia, Rieti, Fatebenefratelli San Pietro Hospital Rome, Umberto I Polyclinic Rome, Salerno, San Cataldo CL), Sansepolcro (AR), Sapri (SA), Savigliano (CN), Savona, Sondrio, Sulmona (AQ), Maria Vittoria Hospital Turin, Sant'Anna Hospital Turin, Trento, Udine, Vallo della Lucania (SA), Varese, Verona, Vigevano (PV), Voghera (PV), Volterra (PI).
Our thanks also to Dr. Franco Gatta and the ZLB company (Bioplasma Italy, Milan, Italy) for stimulating interest in the project, soliciting the replies and organising the computerised management of the questionnaire on the SIMTI website through the Maya Tecnologie company (Verona, Italy).
Footnotes
The Working Group on the “Re-evaluation of the incidence and prophylaxis of HDN in Italy”, which carried out and evaluated the survey, was nominated by the Board of Directors of SIMTI and was composed of Claudio Velati, head of the “Research and Development” area, Giorgio Reali (co-ordinator of the Group), Franco Biffoni, Pietro Bonomo, Augusto d'Angiolino, Fernanda Morelati, and Massimo Ripamonti.
References
- 1.Royal College of Physicians of Edinburgh and Royal College of Obstetricians and Gynaecologists of UK London [No Authors listed] Statement from the Consensus Conference on anti-D prophylaxis. Vox Sang. 1998;74:127–8. doi: 10.1046/j.1423-0410.1998.7420127.x. [DOI] [PubMed] [Google Scholar]
- 2.Levine P, Stetson RE. An unusual case of intra-group agglutination. JAMA. 1939;113:126–7. doi: 10.1001/jama.251.10.1316. [DOI] [PubMed] [Google Scholar]
- 3.Rosenfield RE. Who discovered Rh? A personal glimpse of the Levine-Wiener argument. Transfusion. 1989;29:355–7. doi: 10.1046/j.1537-2995.1989.29489242804.x. [DOI] [PubMed] [Google Scholar]
- 4.Finn R. Report of a meeting at the Liverpool Medical Institution: February 18th 1960. Lancet. 1960;i:526. [Google Scholar]
- 5.Finn R, Clarke CA, Donohue WTA, et al. Experimental studies on the prevention of Rh haemolytic disease. Br Med J. 1961;i:1486–90. doi: 10.1136/bmj.1.5238.1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freda VJ, Gorman JG, Pollack W. Successful prevention of experimental Rh sensitisation in man with an anti-Rh gamma-2-globulin preparation: a preliminary report. Transfusion. 1964;4:26–32. doi: 10.1111/j.1537-2995.1964.tb02824.x. [DOI] [PubMed] [Google Scholar]
- 7.Woodrow JC, Donohoe WT. Rh-immunization by pregnancy: results of a survey and their relevance to prophylactic therapy. Br Med J. 1968;iv:139–44. doi: 10.1136/bmj.4.5624.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sansone G. La malattia emolitica neonatale, ieri e oggi. In: Sansone G, Dambrosio F, editors. Atti del Convegno sui Problemi Attuali della MEN; Genoa. 17–19 December 1971; Genoa: Stringa Editore; 1971. pp. 17–26. [Google Scholar]
- 9.Mollison PL, Walker W. Controlled trials of the treatment of haemolytic disease of the newborn. Lancet. 1952;i:429–33. doi: 10.1016/s0140-6736(52)91949-1. [DOI] [PubMed] [Google Scholar]
- 10.Kleihauer E, Braun H, Betke K. Demonstration von fetalem Hämoglobin in den Erythrozyten eines Blutausstrichs. Klin Wochenschr. 1957;35:637–8. doi: 10.1007/BF01481043. [DOI] [PubMed] [Google Scholar]
- 11.Polensky HF, Sebring ES. Detection of fetal maternal hemorrhage: an evaluation of serological tests related to Rho (D) immune globulin (human) Transfusion. 1971;11:162–5. doi: 10.1111/j.1537-2995.1971.tb04396.x. [DOI] [PubMed] [Google Scholar]
- 12.Nance SJ, Nelson JM, Arndt PA, et al. Quantitation of fetal-maternal hemorrhage by flow-cytometry. A simple and accurate method. Am J Clin Pathol. 1989;91:288–92. doi: 10.1093/ajcp/91.3.288. [DOI] [PubMed] [Google Scholar]
- 13.Salama A, David M, Wittmann G, et al. Use of the gel agglutination technique for determination of fetomaternal hemorrhage. Transfusion. 1998;38:177–80. doi: 10.1046/j.1537-2995.1998.38298193101.x. [DOI] [PubMed] [Google Scholar]
- 14.Sebring ES, Polensky HF. Detection of fetal maternal hemorrhage in Rh immune globulin candidates. A rosetting technique using enzyme treated Rh2Rh2 indicator cells. Transfusion. 1982;22:468–71. doi: 10.1046/j.1537-2995.1982.22683068604.x. [DOI] [PubMed] [Google Scholar]
- 15.de Silva M, Engelfriet CP, Reesink HW, editors. International Forum. Current status of immunoprophylaxis with anti-D immunoglobulins. Vox Sang. 2003;85:328–37. doi: 10.1111/j.0042-9007.2003.364_1.x. [DOI] [PubMed] [Google Scholar]
- 16.Biffoni F, D'Angiolino A, Massaro AL, et al. Recommendations for the management of haemolytic disease of the newborn. Blood Transfus. 2006;4:237–50. [Google Scholar]