Abstract
Background
Voluntary donors normally tolerate blood donation very well, but, occasionally, adverse reactions of variable severity may occur during or at the end of the collection. Aim of this study was to estimate and possibly avoid the cause of unwanted reactions.
Materials and methods
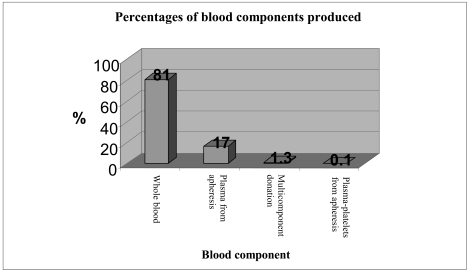
The study was conducted over a period of 6 months, from 24th October, 2005 to 24th April 2006. The donor population analysed consisted of 4,906 donors (3,716 male and 1,190 female). In total, 3,983 (81%) voluntaries have donated whole blood, 851 (17%) plasma from apheresis, 64 (1.3%) experienced multicomponent donation, and 8 (0.1%) were donors of plasma-platelet apheresis.
Results
Only 63 donors (1.2% of all the volunteers) suffered some kind of adverse reaction: 59 (1.08% of the subjects) had mild reactions (agitation, sweating, pallor, cold feeling, sense of weakness, nausea), and only 4 (3 males and 1 female, 0.2%) had more severe disorders, including vomiting, loss of consciousness, and convulsive syncope.
Conclusions
Although the number of donors who developed disturbances during or at the end of blood donations was very low, it is nevertheless desirable to reduce risks to a minimum. A set of advices is provided for preventing problems.
Keywords: blood donors, blood donations, adverse reactions
Introduction
Blood donors normally tolerate the donation very well, but occasionally adverse reactions of variable severity may occur during or at the end of the collection. The adverse reactions that occur in donors can be divided into local reactions and systemic reactions.
Local reactions occur predominantly because of problems related to venous access. They are usually haematomas due to extravasation from the veins, caused by incorrect placement of the needle during the venipuncture. Pain, hyperaemia and swelling may develop at the site of the extravasation. Other local events include pain due to slight trauma to the subcutaneous nerve endings. In most cases, however, these are banal complications that do not require any treatment. Local phlebitis and thrombophlebitis are more serious complications than the foregoing, but are very rare.
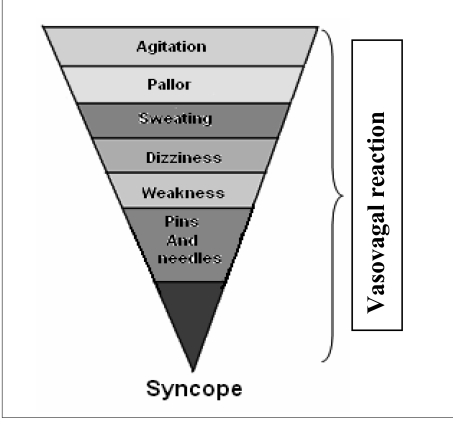
The systemic reactions, in contrast to the local reactions, can be divided into mild or severe. In most cases, they are vasovagal reactions than can be triggered by the pain of the venipuncture, by the donor seeing his or her own blood, by the donor seeing another donor unwell, by the anxiety and state of tension of undergoing the donation, etc. The systemic reactions are characterised by the appearance of pallor, sweating, dizziness, gastrointestinal disorders, nausea, hypotension, and bradycardia. Therapeutic intervention must be swift, otherwise this clinical picture, typical of a vasovagal reaction, will progress into an episode of syncope, of variable severity, which may or may not be complicated by the onset of tonic-clonic muscle spasms (convulsive syncope), accompanied by vomiting and loss of sphincter control.
Systemic reactions can occur during apheresis procedures, which require the use of anticoagulants such as acid-citrate-dextrose (ACD) for the collection of the blood component. This anticoagulant can cause hypocalcaemia, because of chelation. The lowered concentration of calcium ions leads to episodes of paraesthesia of the lips, oral cavity and limbs. These symptoms resolve after interruption of the apheresis procedure, although it may sometimes be necessary to use a therapeutic intervention, such as the administration of calcium gluconate. Much more rarely, tremor, muscle spasms, hypotension, tachycardia, arrhythmia, convulsions and tetany develop.
There are rare reports of acute intoxication due to overdoses of ACD1. Another rare complication, that can occur during apheresis procedures, is severe arrhythmias.
The aim of this study was to estimate the frequency and type of adverse events, distinguishing mild disturbances from more severe reactions, and to measure the time for the donor to recover a state of well-being. In this way it is possible to monitor and improve the donation clinics and the environmental context. A set of rules can be created to govern the behaviour of the staff and improve the quality of the interventions.
Our survey identified a group of donors predisposed to the development of adverse reactions and enabled us to prevent problems in these subjects at subsequent donations.
Materials and methods
The population analysed in this study consisted of 4,906 voluntary blood donors of whom 3,716 (75.74 %) were male and 1,190 (24.26%) female (male/ female ratio 3:1). The mean age of the men was 43 years and that of the women 41 years (minimum age 18 years, maximum age 66 years). The donors included were selected for complying with requisites established by current legislation.
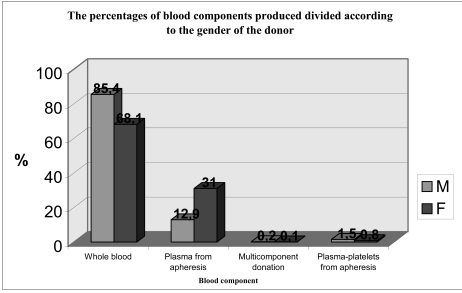
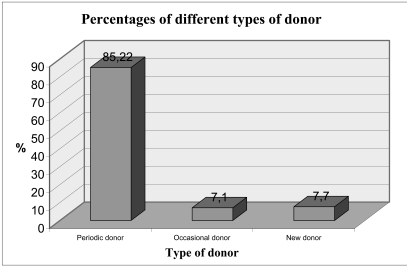
The population was further characterised into 3,983 (81%) donors of whole blood, 851 (17%) donors of plasma from apheresis, 64 (1.3%) multicomponent donors, and 8 (0.1%) donors of plasma-platelets from apheresis (Figure 1). Figure 2 illustrates the contributions that the two sexes gave to the different types of donations. The volunteers were also divided into 4,181 periodic donors, 348 occasional donors and 377 new donors (Figure 3).
Figure 1.
The percentages of different types of blood components produced during the period under consideration
Figure 2.
The percentages of the different blood components produced, divided according to the gender of the donor
Figura 3.
The percentages of different types of donor
In order to create the database, a data collection form was designed to record the parameters analysed in the study. The parameters were recorded in a dichotomous form (present/absent). A statistical-inferential analysis was carried out on the data collected, to determine whether there were any significant associations or independent factors.
The statistical analysis of the data, regarding both the descriptive statistics and the inferential analysis, was conducted using the SPSS, Minitab and OpenStat software packages. The various models of statistical analysis used concerned:
a contingency analysis of the groups of ‘first-time donors’ and ‘periodic donors’ against the factors, agitation and sweating;
multivariate logistic regression analysis, taking into consideration various factors, to quantify the weight of each of the different factors such as pallor, sweating, agitation, pain of a difficult venipuncture compared to that of an efficient venipuncture, in the development of a vasovagal reaction;
multivariate logistic regression analysis, to determine the weight of different factors, such as first donation, periodic donation, difficult venipuncture compared to an efficient venipuncture, in the development of syncope.
The data collection form had 22 fields, divided into four groups. The first group consisted of: sex, age, first donation, periodic donation. The second group concerned type of donation: whole blood, plasmapheresis, multicomponent apheresis. The third group consisted of efficient venipuncture and difficult venipuncture. Finally, the fourth group concerned the symptoms felt, by the donor during or after the donation, and consisted of 13 parameters: agitation, pallor, sweating, pins and needles, feeling of weakness, cold sensation, dizziness, nausea, vomiting, loss of consciousness, convulsive syncope, and loss of sphincter control.
In our Transfusion Service, the phlebotomy team consists of doctor who take the donation (four members of the permanent staff and one temporary doctor) and the nursing staff (six units of staff).
Results
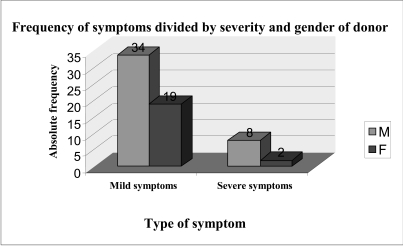
The incidence of vasovagal reactions was very low, occurring in 0.2 % of the total sample. Indeed, among the population of 4,906 donors, only 63 suffered some kind of adverse reaction, of a minor or more severe entity, accounting for 1.2% of all the subjects (Figures 4, 5 and 6). Among the population of 4,906 donors, the statistical probability of some type of adverse reaction was p = 1.2 %, a rather low value, considering the large number of subjects forming the statistical sample and the fact that ‘adverse reactions’ include vasovagal reactions, which are themselves represented by predominantly minor symptoms.
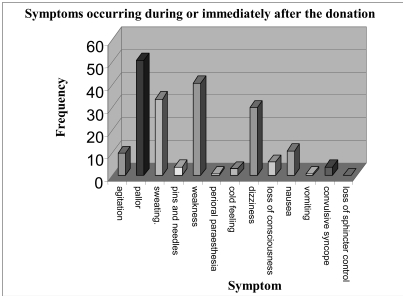
Figure 4.
Absolute frequency of mild or severe symptoms, stratified by gender, among the 63 subjects who had some kind of adverse reaction
Figure 5.
Absolute frequency of the symptoms occurring in donors during or immediately after the donation
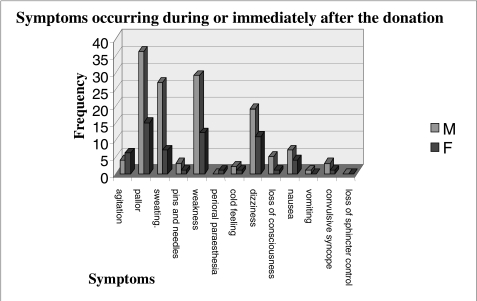
Figure 6.
Absolute frequency of symptoms according to the gender of the donors. It can be seen that women develop adverse reactions during donation of blood more rarely than do men
The statistical probability of an episode of complete loss of consciousness was equivalent to an incidence of 0.1%, that is, one case every 1,000 donors. The 63 donors who had some kind of adverse reaction were divided into two groups: the first group consisted of subjects who had mild adverse reactions (agitation, sweating, pallor, dizziness, cold feeling, sense of weakness, nausea, pins and needles)2,7,9,10; the second group consisted of the subjects who had severe adverse reactions (loss of consciousness, convulsive syncope, loss of sphincter control, vomiting)2,10–13. Only 1.08% of the subjects had mild adverse reactions and another 0.2% had more severe disorders, including vomiting, loss of consciousness, loss of sphincter control, and convulsive syncope.
The greatest number of reactions occurred during or after donations of whole blood, with there being fewer after donations of other blood components. This finding is explained by the greater number of donors, both periodic donors and first-time donors, recruited to give whole blood; plasma and other blood components were almost always donated by periodic donors. As can be seen from the therapeutic interventions carried out to resolve the clinical picture caused by “minor symptoms”, it was sufficient to put the subject in the Trendelenburg position (‘antishock’ position) to increase the afterload and thus provide adequate oxygenation of the brain.
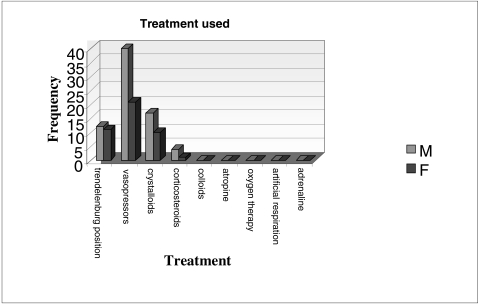
In other circumstances, besides putting the subject in the antishock position, it was also necessary to administer oral vasopressors (midodrine hydrochloride); fluid supplementation with an infusion of crystalloids was rarely needed (Figure 7). It should be noted that in no case were colloids necessary to expand the circulatory volume and, likewise, atropine was never necessary to restore the cardiac rhythm or for any other haemodynamic problems. Indeed, it should be appreciated that it is not necessary to use colloids (as clearly demonstrated by the data), since the volume of blood removed during a donation (450 mL ± 10% of blood) represents only about 10% of the total blood mass of a subject weighing 70 Kg. This is far from the tabulated values of blood loss that can cause hypovolaemic shock, since more than 15–20% of the total blood mass, that is, 800–1,500 mL of blood, need to be lost, in order to be in at least class I risk of hypovolaemia. Thus, a donation of 450 mL of blood will not put the subject even in class I risk, according to the table of classification of blood loss16–19. Nevertheless, this does not mean that some subjects, particularly those with marked anxiety, can not have a slight decrease in blood pressure21.
Figure 7.
Absolute frequency of the different types of treatment used
Among those subjects who did suffer adverse reactions, the systolic blood pressure never decreased below 80–90 mmHg immediately after the vasovagal reaction or syncope; the diastolic blood pressure values never fell below 40 mmHg and the heart rate was never slower than 40 beats per minute. For these reasons, it was not necessary to use more aggressive therapy; in all cases, intravenous infusion of crystalloids and oral administration of vasopressors was sufficient to control the symptoms1,4,5,9,21–24. Subjects with severe symptoms were given not only oral vasopressors, but also intravenous infusion of crystalloids in a ratio of 3:1, as suggested by the best accredited guidelines and protocols on blood loss. In no case was it necessary to use atropine to restore the heart rate. Only in a few cases, were corticosteroids administered in saline solution (hydrocortisone 1 g, methylprednisolone 1 g for intravenous use, Figure 7)25–31. All subjects, who had vasovagal reactions, recovered within 10–15 minutes after the donation, whereas the donors who suffered syncope recovered in 15–20 minutes with fluid compensation.
It can be said that agitation, pallor and sweating are the harbingers of a vasovagal reaction; indeed, these symptoms can be present already before the donation, being associated with the emotions that the donor accumulates during the reception at the donor site and while waiting to make the donation.
In this study it was possible to describe the sequential development of the symptoms precisely and, subsequently, they were recorded. It is, therefore, clear that dizziness and gastric disorders (nausea, dysphagia, epigastric pain and gastric pyrosis) represent the fully developed phase of the vasovagal reaction.
Of the 63/4,906 (1.2%) donors who had adverse reactions to blood donation, only 40 (0.8%) were administered oral vasopressors, while the other 23 (0.4%) recovered from the vasovagal reaction simply from being placed in the antishock position. Of the 63 donors who had a vasovagal reaction, only 18 (0.36%) were given crystalloid solutions, while less than five (0.1%) required additional therapy with cortisone (Figure 7). In no case was re-animation based on oxygen therapy or administration of adrenaline needed.
Episodes of convulsive syncope occurred in 0.08% (3/3,716) of males and also in 0.08 % (1/1,190) of females of the whole population. In these cases, it was necessary to use crystalloids and cortisone, which resolved this clinical complication within 15–20 minutes, without there being any repercussions in the hours following the donation.
Only one subject (0.02%) developed a vasovagal reaction with vomiting, which resolved very quickly after the infusion of crystalloids and cortisone.
The subjects, who manifested the typical clinical picture of a vasovagal reaction or episodes of syncope or convulsive syncope, were treated according to the Basic Life Support (BLS) protocol, in which the medical and nursing staff were trained during the compulsory BLS-D course.
Donors who developed the a vasovagal reaction were immediately placed in the antishock position. Their vital signs (blood pressure, heart rate and oxygen saturation) and state of consciousness were measured. The first action consisted in ensuring venous access, in case the infusion of fluids or drugs became necessary.
Likewise, the donors affected by episodes of syncope were also immediately placed in an antishock position, with particular care taken to hyperextend the head, in order to ensure that the tongue did not obstruct the oropharynx and that the respiratory tract remained patent, thus facilitating quick recovery.
It is essential to intervene rapidly in subjects with syncope, because in hypoxic states clonic contractions can develop. These, obviously, are not related in any way to epilepsy, but can lead to lesions due to the venipuncture needle and even cause the donor to fall off the donation bed/chair. It is, therefore, essential that the staff present restrict the movements of the donor. Donors who have any disorders must be retained at the donation centre until all vital parameters have returned to normal.
The follow-up of the subjects who had any type of complication was continued into the post-donation period, that is, for 20 to 30 minutes. After this period, the donors left the Transfusion Service, but were asked to inform the staff of the Service of their state of well-being the following day. None reported psychophysical disturbances in the second day post-donation20,22,23.
Discussion
Contingency analysis between groups of first-time donors and periodic donors
A contingency analysis of the groups of “first-time donors” and “periodic donors”, with regards to the variables agitation and sweating, which together reflect a state of anxiety, was conducted in order to study the level of association with these two groups of donors, stratified by gender. The analysis of the first-time donors showed that there was not a significant degree of association (chi-square = 5.59; 95 % CI and p = 0.06).
The contingency analysis of periodic donors (subjects who had, therefore, already given blood) vs. agitation and sweating, showed a strong, very statistically significant association (chi-square = 13.47; 95% CI and p = 0.001). This finding demonstrates a greater tendency to develop an anxiety syndrome, with this being much more pronounced in periodic donors; this can be explained by the not very large number of first donors (377/4,906; 7.7%) or by an anxiety factor that is intensely felt during subsequent donations. In fact, a state of anxiety can be manifested even before the donor reaches the donation bed/chair, with premonitory signs, such as agitation and sweating, which in themselves form a condition predisposing to a state of distress.
There was not a well-defined pathophysiological cause for the vasovagal reactions, but rather a set of neuropsychological factors that the subjects had developed during their life, starting from the first donation. In order to determine which of the prodromic factors was predominant in inducing vasovagal reactions during blood donation, we used a multivariate logistic regression model to identify those factors that could be responsible for causing the above mentioned state of distress.
Multivariate logistic regression analysis for vasovagal reactions
This analysis was used to determine whether there was a connection between the development of pallor and a difficult venipuncture. The donors who developed pallor were divided into two groups: those in whom the venipuncture had been traumatic and those in whom the venipuncture had been efficient. The logistic regression analysis showed that the group of donors, in whom the venipuncture was difficult, had a statistically higher probability of developing pallor (95% CI and p < 0.001). From these data, it can be concluded that a traumatic venipuncture, compared to an easy one, is a strong determinant of a vasovagal reaction. It can, therefore, be stated that a painful stimulus caused by venipuncture can lead to a vasovagal reaction.
The analysis was also used to determine whether there was a causal connection between the symptom of “sweating” and difficult venipuncture versus atraumatic venipuncture. The aim was to determine how much these two independent variables were determinant in inducing sweating. The logistic regression analysis showed that traumatic venipuncture was a statistically significant determinant (p <0.001 and 95% CI) compared to easy, non-harmful venipuncture. It can be said that the variable “traumatic venipuncture” plays a predisposing role in causing sweating and, therefore, in triggering vasovagal reactions.
Finally, the analysis was used to determine whether several factors simultaneously play a role in determining vasovagal reactions. In this case the dependent variable was taken to be the symptom of pallor, and the number of independent factors was increased to include traumatic venipuncture, easy venipuncture, agitation and sweating. The multivariate logistic regression analysis showed that there was a marked statistical significance (p < 0.0002 and 99% CI), in favour of the factor sweating.
All this is in agreement with the literature, in which it is described that an anxiogenic stimulus, represented by the strong emotion of giving blood or the donor’s sight of his or her own blood, evokes fear and anxiety and the expectation that the phenomenon could be repeated has the same emotional significance.
From a purely psychological point of view, this phenomenon can be likened to what is technically defined, in psychology, as a “simple phobia”, which is nothing other than a learned behaviour associated with an anxiogenic stimulus6,7,21. This type of behaviour, usually not conscious, is maintained by a set of dramatic or catastrophic thoughts and by unpredictable complications or consequences, that can occur during the donation. Vasovagal reactions often occur in these subjects immediately after the needle insertion, or even later, once the donation has been completed.
It can be said that, irrespectively of whether the venipuncture is traumatic or atraumatic, the donor attributes this part of giving blood a particular weight. Indeed, for many people, one of the uncertainties about giving blood derives from the psychological impact of the needle insertion.
Multivariate logistic regression analysis for syncope
The aim of the first analysis was to determine the importance of some factors such as first-time donor, periodic donor, and effective vs traumatic venipuncture in determining an episode of syncope. The group of donors who lost consciousness was stratified, according on the basis of several independent variables: first-time donor, periodic donor, effective venipuncture and traumatic venipuncture.
The multivariate logistic regression model showed very clearly that the greatest statistical significance occurred in the group of periodic donors (p <0.002 and 95% CI). This finding, which might seem to contradict what was stated above for vasovagal reactions, could suggest two fundamental concepts: the group of periodic donors who developed syncope was more numerous than that of the first-time donors and that loss of consciousness is not strictly related to the venipuncture, but rather to other factors. While venipuncture is one of the triggers of a vasovagal reaction, syncope represents the normal evolution of a poorly managed clinical situation.
At this point of the study, we used logistic regression analysis to determine whether there were factors associated with the symptoms of vasovagal reactions in common with factors causing a loss of consciousness. In this cases, loss of consciousness was taken as the dependent variable, with the independent variables being a cold feeling, sweating, pallor and dizziness. The factors sweating and dizziness emerged as being statistically significant (p <0.05 and 95% CI).
Sweating, in fact, causes a further decrease in blood pressure because of vasodilatation, with sequestration of the blood in splanchnic organs and stasis in the lower limbs, due to gravity. All this is added to the fall in blood pressure caused by the removal of blood during the donation (450 mL). The result is a slight and temporary deficit in blood flow to the brain. Dizziness follows on from hypoxia and causes a sense of ill-being or a vasovagal reaction, which sometimes evolves into syncope in the absence of a swift therapeutic intervention. Therefore, as shown by the logistic regression analysis, there is a chain reaction, which starts gradually with a banal vasovagal stimulus and then evolves inexorably into syncope, if not adequately treated13–17,20.
Conclusions
Although the number of donors who developed disturbances in relation to donating blood was very low, it is nevertheless desirable to reduce risks to a minimum, working not only with the maximum environmental safety, but also with complete medical assistance. Thus, a series of innovations have been introduced to facilitate not only the work of the staff, but also safe donation by the volunteer blood donors. The remedies and specific areas of care are the following:
shorten the waiting times,
do not allow the fasted donor to remain standing for long periods,
allow the donor a light breakfast, excluding sugar, milk and milk products, in particular in subjects predisposed to develop some form of distress3,
ensure a comfortable room temperature and humidity,
avoid a semi-sitting position during the donation,
identify those subjects who are particularly anxious and ensure them the greatest comfort and the most assiduous attention by the staff,
if necessary, reduce the amount of blood collected, within the limits allowed by law (range 405–495 mL),
engage particularly anxious donors in conversation, in order to distract their attention from what is happening,
carry out the venipuncture precisely and cleanly,
avoid traumatic needle insertion with invasive and painful manoeuvres,
identify the best venous access, by inspecting both forearms,
if the first venipuncture is unsuccessful, allow the donor to rest and reassure him or her, before attempting a new venipuncture,
do not let the donor leave the donor site too quickly,
invite donors to wear comfortable clothes, avoiding tight ties and belts,
do not let the donors drink very hot or very cold drinks during the recovery phase,
monitor very carefully young, bradycardic donors, whose blood pressures tend to be low,
do not take blood from donors, who have carried out very intensive sporting activities in the preceding 24 hours,
give great care to those donors who take antihypertensive drugs, particularly β-blockers,
donation of blood components is contraindicated after a night shift,
do not allow donors to eat solid foods during the donation16,17,
it is recommended that donor do not drink alcohol the night before a donation,
react swiftly to the initial symptom of pallor, by putting the subject in the Trendelenburg position,
reassure the donor,
loosen any tight clothing, in order to facilitate normal respiration,
if necessary, administer vasopressors per os,
if the donor has low blood pressure, infuse fluids (physiological saline, Ringer’s lactate solution, balanced solutions),
monitor the donor and retain him or her at the donor site until there has been an adequate haemodynamic recovery,
if recovery is very slow, corticosteroids can be administered as a continuous infusion in a solution,
if the pulse is very weak and the heart rate slow, atropine can be administered,
if the clinical situation evolves into an episode of syncope, ensure that the airways are patent.
Figure 8.
The order of appearance of the typical symptoms of a vasovagal reaction in a blood donor, which, if not treated promptly, evolves into syncope
References
- 1.Winters JL. Complications of donor apheresis. J Clin Apher. 2006;21:132–41. doi: 10.1002/jca.20039. [DOI] [PubMed] [Google Scholar]
- 2.Danic B, Gouezec H, Bigant E, et al. Incidents of blood donation. Transfus Clin Biol. 2005;12:153–9. doi: 10.1016/j.tracli.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 3.van Jaarsveld H, Pool GF. Beneficial effects of blood donation on high density lipoprotein concentration and the oxidative potential of low density lipoprotein. Atherosclerosis. 2002;161:395–402. doi: 10.1016/s0021-9150(01)00638-4. [DOI] [PubMed] [Google Scholar]
- 4.Bern MM, Bierbaum BE, Katz JN, et al. Autologous blood donation and subsequent blood use in patients undergoing total knee arthroplasty. Transfus Med. 2006;16:313–9. doi: 10.1111/j.1365-3148.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 5.Tsuboi S, Tamura Y, Fujibayashi T, et al. Hemagglutination of preoperative blood donation in patients with rheumatoid arthritis. Mod Rheumatol. 2004;14:77–81. doi: 10.1007/s10165-003-0271-4. [DOI] [PubMed] [Google Scholar]
- 6.Schulzki T, Seidel K, Storch H, et al. A prospective multicentre study on the safety of long-term intensive plasmapheresis in donors (SIPLA) Vox Sang. 2006;91:162–73. doi: 10.1111/j.1423-0410.2006.00794.x. [DOI] [PubMed] [Google Scholar]
- 7.Newman BH, Newman DT, Ahmad R, Roth AJ. The effect of whole-blood donor adverse events on blood donor return rates. Transfusion. 2006;46:1374–9. doi: 10.1111/j.1537-2995.2006.00905.x. [DOI] [PubMed] [Google Scholar]
- 8.France CR, France JL, Roussos M, et al. Mild reactions to blood donation predict a decreased likelihood of donor return. Transf Apher Sci. 2004;30:17–22. doi: 10.1016/j.transci.2003.08.014. [DOI] [PubMed] [Google Scholar]
- 9.Zervou EK, Ziciadis K, Karabini F, et al. Vasovagal reactions in blood donors during or immediately after blood donation. Transfus Med. 2005;15:389–94. doi: 10.1111/j.1365-3148.2005.00600.x. [DOI] [PubMed] [Google Scholar]
- 10.Newman BH. Blood donor complications after whole-blood donation. Curr Opin Hematol. 2004;11:339–45. doi: 10.1097/01.moh.0000142105.21058.96. [DOI] [PubMed] [Google Scholar]
- 11.Newman BH. Vasovagal reaction rates and body weight: findings in high- and low-risk populations. Transfusion. 2003;43:1084–8. doi: 10.1046/j.1537-2995.2003.00478.x. [DOI] [PubMed] [Google Scholar]
- 12.Guerra MJ, Vaz MJ, Silva O. Adverse reactions of blood donation. Servir. 2002;50:232–5. [PubMed] [Google Scholar]
- 13.Tomita T, Takayanagi M, Kiwada K, et al. Vasovagal reactions in apheresis donors. Transfusion. 2002;42:1561–6. doi: 10.1046/j.1537-2995.2002.00241.x. [DOI] [PubMed] [Google Scholar]
- 14.Newman BH, Pichette S, Pichette D, Dzaka E. Adverse effects in blood donors after whole-blood donation: a study of 1000 blood donors interviewed 3 weeks after whole-blood donation. Transfusion. 2003;43:598–603. doi: 10.1046/j.1537-2995.2003.00368.x. [DOI] [PubMed] [Google Scholar]
- 15.Hanson SA, France CR. Predonation water ingestion attenuates negative reactions to blood donation. Transfusion. 2004;44:924–8. doi: 10.1111/j.1537-2995.2004.03426.x. [DOI] [PubMed] [Google Scholar]
- 16.Karger R, Slonka J, Junck H, et al. Extracorporeal blood volume of donors during automated intermittent-flow plasmapheresis and its relevance to the prevention of circulatory reactions. Transfusion. 2003;43:1096–106. doi: 10.1046/j.1537-2995.2003.00455.x. [DOI] [PubMed] [Google Scholar]
- 17.Carrasquilla G. Immediate adverse reactions to donation: frequency and characterization. Biomedica. 2001;21:224–7. [PubMed] [Google Scholar]
- 18.Perseghin P, Capra M, Baldini V, et al. Bradykinin production during donor plasmapheresis procedures. Vox Sang. 2001;81:24–8. doi: 10.1046/j.1423-0410.2001.00058.x. [DOI] [PubMed] [Google Scholar]
- 19.Committee on trauma. Advanced trauma life support student manual. Chicago: American College of Surgeons; 1989. p. 57. [Google Scholar]
- 20.Strauss RG. Mechanisms of adverse effects during hemapheresis. J Clin Apher. 1996;11:160–4. doi: 10.1002/(SICI)1098-1101(1996)11:3<160::AID-JCA7>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 21.Ditto B, France CR. Vasovagal symptoms mediate the relationship between predonation anxiety and subsequent blood donation in female volunteers. Transfusion. 2006;46:1006–10. doi: 10.1111/j.1537-2995.2006.00835.x. [DOI] [PubMed] [Google Scholar]
- 22.Krumholz A, Ness PM, Hauser WA, et al. Adverse reactions in blood donors with a history of seizures or epilepsy. Transfusion. 1995;35:470–4. doi: 10.1046/j.1537-2995.1995.35695288764.x. [DOI] [PubMed] [Google Scholar]
- 23.Ogata H, Iinuma N, Nagashima K, et al. Vasovagal reactions in blood donors. Transfusion. 1980;20:679–83. doi: 10.1046/j.1537-2995.1980.20681057157.x. [DOI] [PubMed] [Google Scholar]
- 24.Gorodetskii VM. Reactions observed in blood donors and patients during cytapheresis on the blood cell separator. Ter Arkh. 1978;50:129–31. [PubMed] [Google Scholar]
- 25.Ingerslev J. Safety of plasma derivatives. Haemostasis. 1994;24:311–23. doi: 10.1159/000217119. [DOI] [PubMed] [Google Scholar]
- 26.Bellitti P, Valeriano R, Gasperi M, et al. Cortisol and heart rate changes in first- and fourth-time donors. Vox Sang. 1994;67:42–5. doi: 10.1111/j.1423-0410.1994.tb05036.x. [DOI] [PubMed] [Google Scholar]
- 27.Westphal RG. Health risks to cytapheresis donors. Clin Haematol. 1984;13:289–301. [PubMed] [Google Scholar]
- 28.Pisciotto P, Sataro P, Blumberg N. Incidence of adverse reactions in blood donors taking antihypertensive medications. Transfusion. 1982;22:530–1. doi: 10.1046/j.1537-2995.1982.22683068620.x. [DOI] [PubMed] [Google Scholar]
- 29.Sandler SG, Nusbacher J. Health risk of leukapheresis donors. Haematologia (Budap) 1982;15:57–69. [PubMed] [Google Scholar]
- 30.Bonomo P, Garozzo G, Bennardello F. The selection of donors in multicomponent collection management. Transfus Apher Sci. 2004;30:55–9. doi: 10.1016/j.transci.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Despotis GJ, Goodnough LT, Dynis M, et al. Adverse events in platelet apheresis donors: a multivariate analysis in a hospital-based program. Vox Sang. 1999;77:24–32. doi: 10.1159/000031070. [DOI] [PubMed] [Google Scholar]