Abstract
Objectives
To test the effectiveness of the CHAMP among black South Africans in KwaZulu-Natal, South Africa.
Methods
A randomized control trial was conducted in KwaDedangendlale, South Africa, among youths (ages 9-13) and their families (245 intervention families rearing 281 children and 233 control families rearing 298 children). The CHAMPSA intervention targeted HIV risk behaviors by strengthening family relationship processes as well as targeting peer influences through enhancing social problem solving and peer negotiation skills for youths.
Results
Among caregivers in the control and experimental conditions, significant intervention group differences were revealed regarding HIV transmission knowledge, less stigma toward HIV-infected people, caregiver monitoring—family rules, caregiver communication comfort, caregiver communication frequency and social networks. Among youths, data revealed that control and experimental groups were significantly different for children in AIDS transmission knowledge and less stigma toward HIV-infected people.
Conclusions
CHAMPSA enhances a significant number individual, family and community protective factors that can help youths avoid risky behaviors leading to HIV-positive status.
Keywords: South Africa, HIV/AIDS, prevention
When the current research project began 5 years ago, South Africa had an estimated 5 million adults and children living with HIV/AIDS.1 Despite numerous deaths, in 2005, this number had increased to an estimated 5.5 million.2 Adolescents and young adults are at a particularly high risk of infection, as they evidence alarmingly high rates of both HIV prevalence and incidence.3-6 For example, the HIV prevalence rate for males 15-19 years of age is 3.2%. For females in the same age range, it is 9.4%. For males 20-24 years, the HIV prevalence rate is 6.0%; the female rate is 23.9%.3 As South-African youths are at particularly serious risk for HIV exposure, prevention efforts with preadolescent children prior to sexual debut are important to ensure that newly sexually active cohorts do not become infected.
Recent studies suggest that behavioral interventions developed in western countries may be effectively implemented as a means of reducing the spread of HIV in South Africa.7,8 The current study examines an adaptation of the Collaborative HIV Adolescent Mental Health Program (CHAMP),9 which was developed in the United States, as a means of HIV prevention in South Africa. This adaptation of the CHAMP Family Program, entitled CHAMP South Africa (CHAMPSA), followed the same format as the CHAMP Family Program implemented in the United States. Specifically, within the CHAMP Family Program youth HIV risk behaviors are impacted by strengthening family relationship processes, as well as targeting peer influences through enhancing social problem-solving and peer negotiation skills for youths. Given the evidence of the important protective role that families can play in reducing risk behavior in adolescents,9-12 there is a clear need for programs that strengthen the protective roles of families toward reducing HIV infection risk in South-African adolescents. In addition to these protective factors, ethnographic information gathered to adapt CHAMP to South Africa13-15 suggested that the dynamics of child abuse, stigma, grief from loss (from AIDS), and social capital were important risk and protective factors to consider. Thus, CHAMPSA was designed to benefit from pro-social peer and support networks by using multiple-family groups.9,16-19
Given the success of the CHAMP Family Program in the United States,9,20 we hypothesize South-African adolescents in the CHAMPSA experimental condition will evidence enhanced outcomes on study measures relative to the youths in the comparison condition.
Theoretical Basis
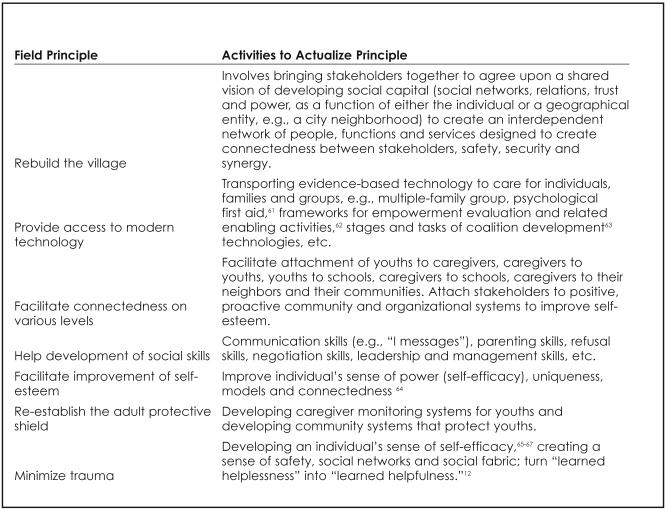
The Theory of Triadic Influence (TTI)21 was used to guide the CHAMPSA program. Specifically, 7 community field principles were developed from the TTI12,22,23 (Figure 1) to underpin CHAMPSA. These 7 field principles were designed to guide academic/community partnerships to actualize the TTI and to base their intervention on sound scientific theory. Bell9 suggests these 7 universal field principles of behavior change have been found to be effective in promoting resiliency and behavior change in youths in a number of community-based projects.12,24,25
Figure 1. Seven field principles derived from the Theory of Triadic Influence9,22-24.
Adaptation of CHAMP for South Africa
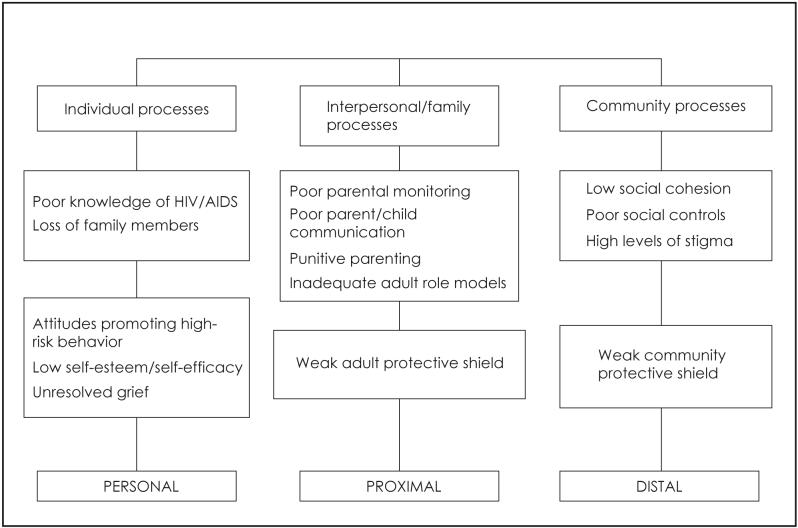
Two distinct stages characterized the adaptation of CHAMP for the South-African context. The first stage was an ethnographic process of adapting the U.S. CHAMP for the South-African context and is described elsewhere.13,14 This stage created the first manual. Synergy between ethnographic data and TTI led CHAMPSA to develop a person/situation-centered matrix representing individual, interpersonal/family and community levels of influence (Figure 2). These levels of influence were the targets of CHAMPSA. The second stage involved piloting the adapted manual on 94 families and used formative evaluation involving focus group discussions with participants about each session to inform the final CHAMPSA, cartoon-based, graphic prevention manual.15,17
Figure 2. Person-/situation-centered matrix and levels of influence.
METHODS
Study Site and Sample
The current study was conducted in KwaDedangendlale, which is 40 km outside of Durban on the eastern seaboard of South Africa. KwaDedangendlale’s population is black South Africans. Among the current sample, the majority of the 478 caregivers speak Zulu, 64% are Christian, and 59% are unemployed. Migration rates are low, with 74% of the sample living in the area for ≥5 years. Province-wide HIV infection rates are high. For example, in 2006 the antenatal clinic HIV rate was 39.1% positive.26 Forty-nine percent of caregivers in the current sample reported receiving a pension/disability grant, and 67% reported receiving a child support grant. Nineteen percent of caregivers reported having no formal education, 46% had a level of education between grades 1-5, and 35% reported having a formal education between grades 6-12. Among the 557 children that comprised the current sample, 59% were female and the average child was 11 (SD=2.9; range=9-13) years old. Sixty-four percent of children attended either fourth or fifth grade, while 13% attended either second or third grade, and 23% attended either sixth or seventh grade.
Community Engagement
CHAMPSA was initiated understanding the importance of working with community members in the design, delivery and evaluation of a HIV prevention initiative.9,27 When CHAMP was first introduced in South Africa, a steering committee was initially formed, comprising researchers and traditional and political leaders from the target site. This steering committee oversaw the entry of the CHAMPSA program into the area as well as the initial adaptation and piloting of the CHAMPSA manualized intervention. Following the piloting and revisions to the first manual, a CHAMPSA collaborative advisory board was formed comprising the original steering committee as well as trained parent facilitators who had been exposed to the pilot intervention. This collaborative advisory board oversaw the main study.
School Selection and Randomization
Schools were randomly assigned to an experimental or control condition through the following process. A meeting of schools in 1 of 4 school sites was called by the CHAMPSA board member responsible for that area. Typically, the meeting would comprise teachers and principals. CHAMPSA staff would then explain the CHAMPSA program and schools were then requested to indicate if they wished to participate. A school was then assigned an experimental school status on the basis of a random pick of all the participating schools. A second pick was done of the remaining schools in the area for a control school. The schools were all public schools with similar resource allocation by the education department. Three schools used in piloting the intervention were excluded, and 2 schools refused participation (total number of KwaDedangendlale primary schools is 25). Each school received a school improvement stipend of $1,000. The intervention was free of charge, while a stipend of $8 was given to each family for attending each session and $30 for attending all 10 sessions.
Participants
Participants were students enrolled in second-to-seventh-grade classes in the 20 primary schools located within the 4 community areas (Molweni, KwaNyusawa, KwaNgcolosi and Qadi) of KwaDedangendlale. Potential study participants were required to meet the following criteria: children between the ages of 9-13 years old, being reared by an adult caregiver age >18 years that fulfills parenting responsibilities, enrolled in school, and indicated agreement to participate in the study via caregiver consent and child assent. As 30% of study youths lived with a caregiver other than a parent, the adults in the youths’ lives are referred to as caregivers rather than parents in this report. Data were collected over 4 years (May 2003 to April 2006) from a total of 579 youths and 478 caregivers in KwaDedangendlale.
Intervention
The final adapted CHAMPSA manualized program [AmaQhawe (Champions) program], comprises 10-90-minute sessions delivered over 10 weekends. Given the amount of time families are required to devote to the program, they were paid a stipend of $8 for each session attended as well as $30 incentive for attending all 10 sessions. The sessions were designed to increase HIV knowledge and decrease stigma surrounding HIV infections; increase authoritative parenting, caregiver decision-making and caregiver monitoring of children; increase family frequency and comfort discussing hard-to-discuss subjects (e.g., sexuality and risky behaviors); increase connectedness to caregiver social networks; decrease neighborhood disorganization, and increase social control and cohesion. The manual introduces these skills through dramatic depiction in a cartoon-based storyline. In addition to teaching application of these skills, to avoid negative parenting strategies and increase youths’ social skills, the CHAMPSA program provides the necessary group context for caregivers collectively to renegotiate caregiver norms and practices towards health-enhancing alternatives.18 Together with the formation of the collaborative board, these processes provide the opportunity for the program to strengthen the “community protective shield” and “rebuild the village,” promoting ownership and sustainability of these efforts on completion of the project.22 The existing school-based HIV prevention curriculum served as the control condition for the proposed study. The vast majority of youths in the study were exposed to this prevention curriculum consisting of HIV prevention messages delivered by school teachers or health educators.
Staff Training and Implementation
Community caregivers trained as facilitators delivered the intervention on the weekends. Randomizing conditions to schools in the 4 community areas prevented contamination—a problem discovered in the pilot.15 To ensure fidelity of implementation across schools and times, the intervention was manualized and facilitators were trained, supervised and guided by use of a step-by-step facilitator manual. Training entailed attending detailed workshops covering the purpose and content of each session and participatory experiential methods, including facilitation skills. Prior to delivery of the intervention, facilitators rehearsed the various sessions. Further, the previous week’s activities were reviewed through observing and evaluating each facilitator. These weekly meetings also included debriefing sessions and workshops on stress management, dealing with grief and bereavement, and the importance of boundaries and containment when working as facilitators.
Design and Procedure
A treatment verses no treatment repeated-measures design was used. Measures were obtained before and once after participation in the intervention. Active caregiver consent and student assent were obtained before study participation. The research, a 4-institution collaborative effort (Community Mental Health Council, Inc; Human Sciences Research Council; University of KwaZulu-Natal; and the Mount Sinai School of Medicine), was approved by their institutional review boards.
Assessment and Measures
The General Health Questionnaire,28 a Global Indicator of Well-Being Question, Revised Children’s Manifest Anxiety Scale,29 Child Problem Behavior Checklist,30 AIDS Myth Knowledge,31 AIDS Transmission Knowledge Scale,15 Stigma Scale,15 Parenting Styles Scales (Parental Involvement, Psychological Autonomy, Strictness and Punitive Style),31,32 Family Decision-Making Questionnaire,33 a Caregiver Monitoring Interview consisting of 4 parameters,34-37 two Hard-to-Talk-About Scales (comfort and frequency),38 and Social Capital [3 Social Network Analysis Scales (for each of 3 important people to the caregiver),15 Neighborhood Disorganization Scale, Neighborhood Social Control Scale, and Neighborhood Social Cohesion Scale]39,40 were administered to caregivers and youths.
Data Collection
While considerable attention was paid to cultural and language differences in the wording of particular measures in the community consultation and pilot phases, low literacy levels of caregivers (just under 50% had fifth-grade education) required facilitators to provide assistance by reading aloud the items and responses to adult participants. The data were collected in additional sessions before and after the program sessions.
Statistical Methods
Cronbach’s alpha was used to assess the internal consistency of the items for each scale, before and after the intervention with scales with ratings <0.7 being excluded from analysis. The significance of intervention regarding pretest versus posttest change scores was assessed using a mixed-effects regression model41 that adjusted for the nesting of students within schools. The impact of treatment was estimated adjusting for pretest scores and demographic variables (age, gender and youth group affiliation for child data and education, gender and religion for adult data). Bonferroni correction was applied to adjust significance probabilities (P values) for multiple comparisons. The adjusted probabilities were computed as P*=1-(1-P) k, where P is the raw probability and k is the number of statistical comparisons (i.e., k=21 for adults and k=9 for children). All probability values reported in the results section are adjusted for multiple comparisons as described.
RESULTS
Descriptive Statistics
Ninety-four percent of families who began the CHAMPSA HIV prevention intervention completed the entire program. Twenty children and 14 adults did not finish.
Analysis of Intervention Effects
With only 2 time points (e.g., pre and post), only completer analysis was feasible. With probability set at p<0.05, to achieve 80% power without adjusting for multiple comparisons, we can detect an effect size of 0.25 standard deviation (SD) units. Adjusting for multiple comparisons, 80% power is achieved for an effects size of 0.36 SD units for adults and 0.33 SD units for children. Table 1 highlights the analysis of the adult data and provides unadjusted and adjusted probability values, group means and effect sizes. Following adjustment for multiple comparisons, the following variables exhibited significant intervention effects: HIV transmission knowledge (P*<0.0084, ES=0.631), Less stigma toward HIV-infected people (P*<0.0187, ES=0.403), Caregiver monitoring 3-Family rules (P*<0.0729, ES=0.307), caregiver communication comfort (P*<0.0021, ES=0.407), caregiver communication frequency (P*<0.0412, ES=0.197) and social networks-primary (1) (P*<0.0827, ES=0.265).
Table 1. Parameter estimates for intervention effects on scale change scores—caregiver data.
| Items | Estimated Impact | Std Error | P Value | Adjusted P Value P* | Treatment Group (Mean) | Control Group (Mean) | Pooled SD | Effect Size |
|---|---|---|---|---|---|---|---|---|
| General health | 1.75 | 0.79 | 0.0391 | 0.5672 | 0.684 | 2.960 | 7.507 | 0.303 |
| Global indicator of well-being | 0.53 | 0.21 | 0.0199 | 0.3443 | -0.057 | 0.581 | 2.176 | 0.293 |
| Child behavior checklist | 0.97 | 0.93 | 0.3078 | 0.9996 | 1.901 | 3.315 | 9.929 | 0.142 |
| HIV transmission knowledge | 1.07 | 0.25 | 0.0004 | 0.0084 | 0.190 | 1.336 | 1.817 | 0.631 |
| Less stigma toward HIV-infected people | 1.87 | 0.47 | 0.0009 | 0.0187 | 0.207 | 1.991 | 4.427 | 0.403 |
| Caregiver involvement | 0.38 | 0.22 | 0.0962 | 0.8805 | 0.138 | 0.215 | 3.180 | 0.024 |
| Psychological autonomy | -0.07 | 0.63 | 0.9113 | 1.0000 | -0.532 | -0.102 | 5.438 | 0.079 |
| Caregiver strictness | 0.65 | 0.41 | 0.1347 | 0.9521 | 0.036 | 0.538 | 2.927 | 0.171 |
| Punitive parenting | 0.15 | 0.08 | 0.0647 | 0.7545 | 0.088 | 0.239 | 0.825 | 0.184 |
| Family decision making | 1.11 | 0.49 | 0.0360 | 0.5370 | -0.085 | 0.496 | 3.480 | 0.167 |
| Caregiver monitoring 2—knowing where the child is | 0.14 | 0.06 | 0.0177 | 0.3127 | 0.079 | 0.227 | 0.931 | 0.159 |
| Caregiver monitoring 3—family rules | 2.02 | 0.61 | 0.0036 | 0.0729 | 0.849 | 2.742 | 6.157 | 0.307 |
| Caregiver monitoring 4—empathy | 0.27 | 0.16 | 0.1208 | 0.9330 | 0.114 | 0.264 | 1.442 | 0.104 |
| Caregiver communication comfort | 3.10 | 0.58 | 0.0001 | 0.0021 | 1.025 | 3.423 | 5.897 | 0.407 |
| Caregiver communication frequency | 1.98 | 0.55 | 0.0020 | 0.0412 | 1.966 | 2.969 | 5.095 | 0.197 |
| Social networks—primary | 1.67 | 0.51 | 0.0041 | 0.0827 | 0.000 | 1.572 | 5.927 | 0.265 |
| Social networks—secondary | 2.12 | 0.73 | 0.0099 | 0.1886 | -0.496 | 2.382 | 6.352 | 0.453 |
| Social networks—tertiary | 1.19 | 1.29 | 0.3677 | 0.9999 | 1.915 | 1.198 | 8.609 | -0.083 |
| Neighborhood disorganization | -1.07 | 0.45 | 0.0284 | 0.4539 | 0.127 | -0.986 | 3.551 | -0.313 |
| Neighborhood social control | 2.02 | 0.78 | 0.0186 | 0.3258 | 0.502 | 2.261 | 7.780 | 0.226 |
Table 2 highlights the analysis of the child data, revealing that control and experimental groups were significantly different for children following adjustment for multiple comparisons in 2 areas, AIDS transmission knowledge (P*<0.0647; ES=0.496) and less stigma toward HIV-infected people (P*<0.0045; ES=0.698).
Table 2. Parameter estimates for intervention effects on scale change scores—child data.
| Items | Estimated Impact | Std Error | P Value | Adjusted P Value | Treatment Group (Mean) | Control Group (Mean) | Pooled SD | Effect Size |
|---|---|---|---|---|---|---|---|---|
| Revised children’s manifest anxiety | 0.62 | 0.65 | 0.3527 | 0.9800 | 1.00 | 0.23 | 5.12 | 0.15 |
| AIDS transmission knowledge | 0.82 | 0.27 | 0.0074 | 0.0647 | 0.88 | 0.12 | 1.54 | 0.50 |
| Less stigma toward HIV infected people | 3.86 | 0.92 | 0.0005 | 0.0045 | 3.96 | -0.25 | 6.03 | 0.70 |
| Caregiver involvement | 0.48 | 0.35 | 0.1839 | 0.8394 | 1.69 | 0.80 | 4.41 | 0.20 |
| Psychological autonomy | 1.60 | 0.66 | 0.0261 | 0.2118 | 0.45 | -0.93 | 6.00 | 0.23 |
| Caregiver strictness | 0.70 | 0.40 | 0.0982 | 0.6055 | 0.90 | 0.08 | 3.67 | 0.23 |
| Caregiver monitoring 3—family rules | 0.96 | 0.68 | 0.1788 | 0.8302 | 2.54 | 1.83 | 6.43 | 0.11 |
| Caregiver communication comfort | 1.30 | 0.66 | 0.0651 | 0.4544 | 2.08 | 1.58 | 6.48 | 0.08 |
| Caregiver communication frequency | 1.64 | 0.64 | 0.0188 | 0.1570 | 2.24 | 0.93 | 5.42 | 0.24 |
DISCUSSION
CHAMPSA is a family-based, HIV universal prevention intervention based on ethnographic study and health behavior change theory developed from a service/academic/periurban community collaborative partnership. The caregiver results indicate CHAMPSA’s multiple level intervention led to manifold, significant changes with robust effect sizes in the intervention cohort when compared to the control cohort. With respect to individual-level processes, exposure to the program led to an improvement in improvement in AIDS transmission knowledge and less-stigmatizing attitudes towards HIV positive people.
In relation to interpersonal and family processes, the intervention group reported increased comfort and frequency in talking about sensitive issues such as HIV, AIDS, sexuality and substance abuse with their children. Other researchers42,43 have underscored the importance for adults to talk about sex to youths. Further, exposure to the program also resulted in improved caregiver monitoring and control of children’s whereabouts and behavior suggesting improvement in the caregiver “protective shield.”
With regard to community-level processes, the social network analysis-primary (a measure of connectedness to the most meaningful person in caregiver’s life) showed a difference between intervention and control caregivers. This suggests that with regard to support networks, CHAMPSA was successful in strengthening primary support networks, which are central for the development of social capital. Social capital emerges from social networks and can assist individuals and communities through increased social support to cope with daily problems.44 Social networks can provide social capital in the form of social leverage for individuals and groups through facilitating socioeconomic advancement and access to information. Thirdly, social networks can facilitate individual and collective informal social controls, another form of social capital, to help keep neighborhoods safe. Finally, networks can facilitate the development of more formally organized groups to address issues of neighborhood concern, thus the development of social networks forms of the basis of the development of more socially cohesive communities that have greater “collective efficacy”45 to ensure a safer environment. This in turn strengthens the “community protective shield” for youths.
With regard to the findings for children, an increase in HIV knowledge in the experimental compared to the control group indicates HIV education in school curriculums and/or community education alone does not transmit optimal knowledge about HIV. Experimental youths also experienced significantly lower levels of stigma toward people with HIV/AIDS promoting greater openness and discussion of HIV/AIDS issues among young people. CHAMPSA had more influence on caregivers developing protective factors at the level of individual, interpersonal and family, and community level than on youths.
Programs that concentrate singularly on one area of change are likely to have less impact, e.g., education only, often resulting in an increase in knowledge without attendant behavioral change. In the United States, primary prevention programs for school-based youths have led to greater AIDS knowledge, more realistic beliefs about susceptibility and self-efficacy, and positive perceptions concerning the benefits and barriers of risk behavior.46-49 However, because many omit family and peer influences,50,51 with few exceptions, they have not dramatically reduced adolescent sexual risk-taking.46-49
Use of community consultants rather than professionals or paraprofessionals as components of the intervention represents certain challenges (e.g., additional training costs and concerns related to the fidelity of the intervention52). By involving community representatives, these impediments can be addressed resulting in benefits, far outweighing obstacles.53-57 Reliance on community consultants enhances ongoing recruitment efforts and family involvement. Having trained community consultants made it possible to move the service/academic/community collaborative, universal prevention research from “science to service” in an efficient manner when the research ended. We obtained a donation from a private nonpharmaceutical source to provide CHAMPSA to 750 families in KwaZulu-Natal in 2007.58 The involvement of community members in every aspect of CHAMPSA, from design of the intervention, pilot-testing, delivery and research, enhances the likelihood CHAMPSA is relevant and capable of delivering HIV universal prevention infrastructure to families in underserved communities.
Limitations
CHAMPSA targeted families before their youths were likely to engage in behaviors we seek to prevent. This is a limitation and strength. CHAMPSA is a researched intervention based on adolescent development suggesting proximal factors at the child, family and community levels that can alter risk trajectories, e.g., true universal prevention. Thus, our reported outcomes are the only ones appropriate given the age of the youths.
Due to a long history of neglect of health and well-being of black South Africans, it is possible that the subjects were so deprived, it was not CHAMPSA, but having any intervention that caused the good outcomes. However, as there are quite a few interventions, e.g., DRAMAIDS, Love Life, etc., we propose it was the uniqueness of CHAMPSA’s small group, depth intervention that made the impact.17
As KwaDedangendlale is a poor area, paying participants to be involved in the study was a motivating factor in their involvement. However, the genuine involvement of local community residents (who signed confidentiality statements) in the design and delivery of the intervention were also very strong motivators of research subjects’ participation. Another strong motivator of participation was, at the outset, the investigators’ clearly expressed objective: if CHAMPSA proved to strengthen already existing protective factors that could protect youths from engaging in HIV risky behaviors, we would provide CHAMPSA as a community service. Thus, by following Covey’s principle59 of “begin with the end in mind,” we created a “shared vision,”60 creating public will to be involved. This is born out by the continued participation of families from the area in the service delivery dissemination phase in which families are not being paid to participate.
The impact of the intervention is measured over a short time span, i.e., 12 weeks, which may reflect the effects of participation in the study; thus, longer-term evaluation of these effects is needed. The relative absence of effects on family processes for children who participated in the CHAMPSA program compared to caregivers is understandable given the focus of the intervention, which was to strengthen the protective role of caregivers.
One of the major limitations of the study is we did not test for youths’ HIV status at the start of the study. Thus, we cannot compare HIV seroprevalence between the control and experimental youths to determine if there was a difference in seroconversion rates between groups. As the study was designed in 2001, the lack of easy access to HIV testing in South Africa, the greater stigma toward HIV-infected persons, and the youth of the students prevented obtaining this useful information. However, considering the robust results of CHAMPSA’s outcome findings and considering the current greater ease in obtaining HIV seroprevalence status, the next task is to replicate the intervention while collecting HIV baseline seroprevalence of youths in the intervention.
CONCLUSIONS
The caregiver data indicate the adapted CHAMPSA program has served to increase the caregiver protective shield for preadolescent children compared to the comparative condition. Due to the universal prevention intervention being conducted in a typical randomized control design, the internal validity of our findings are considered strong, as the major difference in variables impinging on the experimental and control subjects was CHAMPSA. Further, we suggest that, while the target population was largely drawn from the Zulu ethnic group in South Africa, they are generally representative of black South Africans and that the external validity of the findings of the study for the South-African population is generally robust. Further, the findings mirror the CHAMP program in Chicago’s Southside and Westside; the Bronx, NY; and in Trinidad,9,16,20,27 suggesting universality of the CHAMP effects. We suggest that central to ensuring the transportability and universality of the CHAMP program effects is to engage in a community collaborative approach to the adaptation and delivery of CHAMP ensuring cultural relativity in the application of universal principles of strengthening protective factors associated with less-risky behaviors for adolescents. It is also important to use business strategies59,60 on academic research to ensure science goes to service in a timely manner.
Acknowledgments
Financial support: The research project was funded by the National Institute of Mental Health (NIMH) grant #2RO1 MH-01-004 (principal investigator: Bell, Carl C. $2,179,890). The 2007 Collaborative HIV Adolescent Mental Health Program South Africa (CHAMPSA) service funding comes from a donation from a private nonpharmaceutical source and is earmarked for HIV prevention service delivery ($150,000). Neither NIMH nor the donation from the private nonpharmaceutical source had any involvement in the design or conduct of the study; in the collection, management, analysis or interpretation of the data; or preparation, review or approval of the manuscript.
REFERENCES
- 1.UNAIDS . 2004 Report on the global AIDS epidemic. UNAIDS; Geneva: 2004. [Google Scholar]
- 2.UNAIDS . Overview of the global AIDS epidemic. In: UNAIDS, editor. 2006 Report on the Global AIDS Epidemic. UNNAIDS; Geneva, Switzerland: 2006. pp. 8–43. [Google Scholar]
- 3.Shishana O, Rehle T, Simbayi LC, et al. South African National HIV Prevalence, HIV Incidence, Behaviour and Communication Survey, 2005. HSRC Press; Cape Town, South Africa: 2005. [Google Scholar]
- 4.Dorrington RE, Johnson RF, Bradshaw D, et al. National and Provincial indicators for 2006. Centre for Actuarial Research, South African Medical Research Council and Actuarial Society of South Africa; Cape Town, SA: 2006. The Demographic Impact of HIV/AIDS in South Africa. [Google Scholar]
- 5.Eaton L, Flisher AJ, Aaro LE. Unsafe sexual behavior in South African youth. Soc Sci Med. 2003;56:149–165. doi: 10.1016/s0277-9536(02)00017-5. [DOI] [PubMed] [Google Scholar]
- 6.Ramjee G, Williams B, Gouws E, et al. The Impact of Incident and Prevalent Herpes Simplex Virus-2 Infection on the Incidence of HIV-1 Infection Among Commercial Sex Workers in South Africa. J Acquir Immune Defic Syndr. 2005;39(3):333–339. doi: 10.1097/01.qai.0000144445.44518.ea. [DOI] [PubMed] [Google Scholar]
- 7.Wechsberg WM, Luseno WK, Lam WK, et al. Substance Use, Sexual Risk, and Violence: HIV Prevention Intervention with Sex Workers in Pretoria. AIDS Behav. 2006;10(2):131–137. doi: 10.1007/s10461-005-9036-8. [DOI] [PubMed] [Google Scholar]
- 8.Karnell AP, Cupp PK, Zimmerman RS, et al. Efficacy of an American alcohol and HIV prevention curriculum adapted for use in South Africa: Results of a pilot study in five township schools. AIDS Educ Prev. 2006;18(4):295–310. doi: 10.1521/aeap.2006.18.4.295. [DOI] [PubMed] [Google Scholar]
- 9.McKay MM, Chasse KT, Paikoff R, et al. Family-level Impact of the CHAMP Family Program: a Community Collaborative Effort to Support Urban Families and Reduce Youth HIV Risk Exposure. Fam Process. 2004;43(1):79–93. doi: 10.1111/j.1545-5300.2004.04301007.x. [DOI] [PubMed] [Google Scholar]
- 10.Paikoff RL, Parfenoff SH, Greenwood GL, et al. Parenting, parent-child relationships, and sexual possibility situations among urban African American preadolescents: Preliminary findings and implications for HIV prevention. J Fam Psychol. 1997;11:11–22. [Google Scholar]
- 11.Pequegnat W, Szapocznik J, editors. Working with families in the era of HIV/AIDS. Sage; Thousand Oaks, CA: 2000. [Google Scholar]
- 12.Bell CC. Cultivating Resiliency in Youth. J Adolescent Health. 2001;29:375–381. doi: 10.1016/s1054-139x(01)00306-8. [DOI] [PubMed] [Google Scholar]
- 13.Paruk Z, Petersen I, Bhana A, et al. In: Manfredi R, editor. A focused ethnographic study to inform the adaptation of the NIMH funded CHAMP project in South Africa; XIV International AIDS Conference; Bologna: Moduzzi Editore. 2002.pp. 295–298. [Google Scholar]
- 14.Paruk Z, Petersen I, Bhana A, et al. Containment and contagion: How to strengthen families to support youth HIV prevention in South Africa. Afr J AIDS Res (AJAR) 2005;4(1):57–63. doi: 10.2989/16085900509490342. [DOI] [PubMed] [Google Scholar]
- 15.Bhana A, Petersen I, Mason A, et al. Children and youth at risk: Adaptation and pilot study of the CHAMP (AmaQhawe) programme in South Africa. Afr J AIDS Res (AJAR) 2004;3(1):33–41. doi: 10.2989/16085900409490316. [DOI] [PubMed] [Google Scholar]
- 16.McKay M, Baptiste D, Coleman D, et al. Preventing HIV risk exposure in urban communities: The CHAMP family program in Working with Families in the Era of HIV/AIDS. In: Pequegnat W, Szapocznik J, editors. Community Collaborative Partnerships: The Foundation for HIV Prevention Research. Haworth Press; Binghamton, NY: 2000. pp. 67–87. [Google Scholar]
- 17.Petersen I, Mason A, Bhana A, et al. Mediating social representations using targeted micro media in the form a cartoon narrative in the context of HIV/AIDS: The AmaQhawe Family Project (CHAMP) in South Africa. J Health Psychol. 2006;11(2):197–208. doi: 10.1177/1359105306061180. [DOI] [PubMed] [Google Scholar]
- 18.McKay MM, Harrison ME, Gonzales J, et al. Multiple-family groups for urban children with conduct difficulties and their families. Psychiatr Serv. 2002;53(11):1467–1468. doi: 10.1176/appi.ps.53.11.1467. [DOI] [PubMed] [Google Scholar]
- 19.McKay M, Quintana E, Kim L, et al. Multiple family groups: An alternative for reducing disruptive behavioral difficulties of urban children. Res Soc Work Pract. 1999;9:414–428. [Google Scholar]
- 20.Madison S, McKay MM, Paikoff R, et al. Basic Research and Community Collaboration: Necessary Ingredients for the Development of a Family-based HIV Prevention Program. AIDS Educ Prev. 2000;12(4):281–298. [PubMed] [Google Scholar]
- 21.Flay BR, Petraitis J. The theory of triadic influence: a new theory of health behavior with implications for preventive interventions. In: Albrecht GS, editor. Advances in Medical Sociology, Vol. IV: A Reconsideration of models of health behavior change. JAI Press; Greenwich, CT: 1994. pp. 19–44. [Google Scholar]
- 22.Bell CC, Flay B, Paikoff R. Strategies for Health Behavioral Change. In: Chunn J, editor. The Health Behavioral Change Imperatives: Theory, Education and Practice in Diverse Populations. Kluwer Academic/Plenum Publishers; New York, NY: 2002. pp. 17–40. [Google Scholar]
- 23.Bell CC. [Accessed 01/24/08];Exposure To A Traumatic Event Does Not Automatically Put A person On A Path To Develop PTSD: The Importance of Protective Factors To Promote Resiliency. 2006 Gift From Within [serial online] www.giftfromwithin.org/html/promote.html.
- 24.Bell CC, McKay MM. Constructing a Children’s Mental Health Infrastructure Using Community Psychiatry Principles. J Leg Med. 2004;25(1):5–22. doi: 10.1080/01947640490361808. [DOI] [PubMed] [Google Scholar]
- 25.Project Liberty [Accessed 01/24/08];The Project Liberty homepage. www.projectliberty.state.ny.us/
- 26.Department of Health . National HIV and syphilis antenatal sero-prevalence survey in South Africa. National Department of Health; Pretoria, South Africa. Pretoria, South Africa: 2006. [Google Scholar]
- 27.Baptiste DR, Paikoff RL, McKay MM, et al. Collaborating with an urban community to develop an HIV and AIDS prevention program for black youth and families. Behav Modif. 2005;29(2):370–416. doi: 10.1177/0145445504272602. [DOI] [PubMed] [Google Scholar]
- 28.Pevalin DJ. Multiple applications of the GHQ-12 in a general population sample: an investigation of long-term retest effects. Soc Psychiatry Psychiatr Epidemiol. 2000;35:508–512. doi: 10.1007/s001270050272. [DOI] [PubMed] [Google Scholar]
- 29.Reynolds CR, Richmond BO. Revised Children’s Manifest Anxiety Scale. Western Psychological Services; Los Angeles, CA: 1985. [Google Scholar]
- 30.Achenbach TM, Edelbrock CS. Behavioral problems and competencies reported by parents of normal and disturbed children aged four through sixteen. Monogr Soc Res Child Dev. 1981;46(1):1–82. [PubMed] [Google Scholar]
- 31.Steinberg L, Lamborn SD, Darling N, et al. Over-time changes in adjustment and competence among adolescents from authoritative, authoritarian, indulgent, and neglectful families. Child Dev. 1994;65:754–770. doi: 10.1111/j.1467-8624.1994.tb00781.x. [DOI] [PubMed] [Google Scholar]
- 32.Steinberg L, Lamborn SD, Dornbusch SM, et al. Impact of parenting practices on adolescent achievement: Authoritative parenting, school involvement, and encouragement to succeed. Child Dev. 1992;63:1266–1281. doi: 10.1111/j.1467-8624.1992.tb01694.x. [DOI] [PubMed] [Google Scholar]
- 33.Robin AL, Foster SL. Negotiating Parent-Adolescent Conflict: a Behavioral Family Systems Approach. Guilford; New York, NY: 1989. [Google Scholar]
- 34.Skinner HA, Steinhauer PD, Santa Barbara J. The Family Assessment Measure. Can J Commun Ment Health. 1983;2(2):91–105. [Google Scholar]
- 35.Loeber R, Strouthamer-Loeber M, Costello A, et al. Grant proposal (funded), Office of Juvenile Delinquency Prevention. 1986. Progression in anti-social and delinquent child behavior. [Google Scholar]
- 36.Moos RH, Moos BS. Family Environment Scale manual. 3rd ed. Consulting Psychologists Press; Palo Alto, CA: 1994. [Google Scholar]
- 37.Gorman-Smith D, Tolan PH, Zelli A, et al. The relation of family functioning to violence among inner-city minority youth. J Fam Psychol. 1996;10:115–129. [Google Scholar]
- 38.Levy SR, Lampman C, Handler A, et al. Young adolescent attitudes toward sex and substance use: implications for AIDS prevention. AIDS Educ Prev. 1993;5(4):340–351. [PubMed] [Google Scholar]
- 39.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 40.Sampson RJ, Raudenbush SW. Systematic social observation of public spaces: A new look at disorder in urban neighborhoods. AJS. 1999;105:603–651. [Google Scholar]
- 41.Hedeker D, Gibbons RD. Longitudinal Data Analysis. Wiley; New York, NY: 2006. [Google Scholar]
- 42.Collins PY, Mestry K, Wainberg ML, et al. Training South African mental health care providers to talk about sex in the era of AIDS. Psychr Serv. 2006;57(11):1644–1647. doi: 10.1176/appi.ps.57.11.1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilson HW, Donenberg G. Quality of parent communication about sex and its relationship to risky sexual behavior among youth in psychiatric care: a pilot study. J Child Psychol Psychiatry. 2004;45(2):387–395. doi: 10.1111/j.1469-7610.2004.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carpiano RM. Toward a neighborhood resource-based theory of social capital for health: can Bourdieu and sociology help? Soc Sci Med. 2006;62:165–175. doi: 10.1016/j.socscimed.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 45.Zolotor AJ, Runyan DK. Social capital, family violence, and neglect. Pediatrics. 2006;117:1124–1131. doi: 10.1542/peds.2005-1913. [DOI] [PubMed] [Google Scholar]
- 46.Jemmott JB, Jemmott LS, Braverman PK, et al. HIV/STD Risk Reduction Interventions for African American and Latino Adolescent Girls at an Adolescent Medicine Clinic: a Randomized Controlled Trial. Arch Pediatr Adolesc Med. 2005;159(5):440–449. doi: 10.1001/archpedi.159.5.440. [DOI] [PubMed] [Google Scholar]
- 47.Jemmott JB, Jemmott LS, Fong GT. Reductions in HIV risk associations’ sexual behaviors among Black male adolescents: effects of an AIDS prevention intervention. Am J Public Health. 1992;82:372–377. doi: 10.2105/ajph.82.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jemmott JB, Jemmott LS. Increasing condom-use intentions among sexually active Black adolescent women. Nurs Res. 1992;41:273–279. [PubMed] [Google Scholar]
- 49.Jemmott JB, Jemmott LS, Fong GT. Abstinence and safer sex HIV risk-reduction interventions for African American Adolescents: A Randomized Control Trial. JAMA. 1998;279:1529–1536. doi: 10.1001/jama.279.19.1529. [DOI] [PubMed] [Google Scholar]
- 50.Hutchinson MK, Cooney TM. Patterns of parent-teen sexual risk communication: Implications for intervention. Fam Relat. 1998;47(2):185–194. [Google Scholar]
- 51.Romer D, Black M, Ricardo I, et al. Social influences on the sexual behavior of youth at risk of HIV exposure. Am J Public Health. 1994;84(6):977–985. doi: 10.2105/ajph.84.6.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Atkins MS, Frazier SL, Birman D, et al. School-Based Mental Health Services for Children Living in High Poverty Urban Communities. Adm Policy Ment Health. 2006;33(2):146–159. doi: 10.1007/s10488-006-0031-9. [DOI] [PubMed] [Google Scholar]
- 53.Boyd-Franklin N, Aleman J, Jean-Gilles MM, et al. Cultural sensitivity and competence: African-American, Latino, and Haitian families with HIV/AIDS. In: Boyd-Franklin N, Steiner GL, Boland MG, editors. Children, families and HIV/AIDS: Psychosocial and therapeutic issues. Guilford Press; New York, NY: 1995. pp. 53–77. [Google Scholar]
- 54.Fullilove MT, Fullilove RE., III . Understanding sexual behaviors and drug use among African-Americans: a case study of issues for survey research in Methodological Issues. In: Ostrow DG, Kessler RC, editors. AIDS Behavioral Research. Plenum Press; New York, NY: 1993. pp. 117–132. [Google Scholar]
- 55.Holden GW, Lavigne VV, Cameron AM. Probing the continuum of effectiveness in parent training: Characteristics of parents and preschoolers. J Clin Child Adolesc Psychol. 1990;19(1):2–8. [Google Scholar]
- 56.Kreibick T. Caretakers’ support group. In: Boyd-Franklin N, Steiner GL, Boland MG, editors. Children, families, and HIV/AIDS: Psychosocial and therapeutic issues. Guilford Press; New York, NY: 1995. pp. 167–178. [Google Scholar]
- 57.Wyatt GE, Williams JK, Myers HF. African-American sexuality and HIV/AIDS: Recommendations for future research. J Natl Med Assoc. 2008;100(1):44–51. doi: 10.1016/s0027-9684(15)31173-1. [DOI] [PubMed] [Google Scholar]
- 58.Bell CC. Teens’ Sexual Risk Taking: Early Intervention a Must - Perspective: Beginning at the End. Clin Psych News. 2006;34(7):44. [Google Scholar]
- 59.Covey CR. Principle-Centered Leadership. Simon & Schuster; New York, NY: 1992. [Google Scholar]
- 60.Senge P. The Fifth Discipline. Doubleday; New York, NY: 1994. [Google Scholar]
- 61.National Child Traumatic Stress Network. National Center for PTSD [Accessed 01/24/08];Psychological First Aid - Field Operations Guide. (2nd ed.). 2006 July; www.medicalreservecorps.gov/File/MRC_Resources/MRC_PFA.doc.
- 62.Fetterman DM, Kattarian SJ, Wandersman A. Empowerment Evaluation: Knowledge and Tools for Self-Assessment & Accountability. Sage Publications; Thousand Oaks, CA: 1995. [Google Scholar]
- 63.Florin P, Mitchell R, Stevenson J. Identifying training and technical assistance needs in community coalitions: A developmental approach. Heath Ed Res. 1993;8(3):417–432. doi: 10.1093/her/8.3.417. [DOI] [PubMed] [Google Scholar]
- 64.Bean R. The Four Conditions of Self-Esteem: a New Approach for Elementary and Middle Schools. 2nd ed. ETR Associates; Santa Cruz, CA: 1992. [Google Scholar]
- 65.Bryant R, Guthrie RM. Factor for Posttraumatic Stress: a Study of Trainee Firefighters. Psychol Sci. 2005;16(10):749–752. doi: 10.1111/j.1467-9280.2005.01608.x. [DOI] [PubMed] [Google Scholar]
- 66.Regehr C, Hill J, Glancy GD. Individual predictors of traumatic reactions in firefighters. SJ Nerv Ment Dis. 2000;188:333–339. doi: 10.1097/00005053-200006000-00003. [DOI] [PubMed] [Google Scholar]
- 67.Heinrichs M, Wagner D, Schoch W, et al. Predicting posttraumatic stress symptoms from pretrauma risk factors: a 2-year prospective follow-up in firefighters. Am J Psychiatry. 2005;162(12):2276–2286. doi: 10.1176/appi.ajp.162.12.2276. [DOI] [PubMed] [Google Scholar]