Abstract
Three isolates of Streptococcus agalactiae highly resistant to multiple fluoroquinolones were isolated in Japan. Compared with susceptible strains of S. agalactiae, these quinolone-resistant strains had double point mutations within the quinolone resistance-determining regions of gyrA and parC; Ser-81 was changed to Leu (TCA → TTA) in the amino acid sequence deduced from gyrA, and Ser-79 was changed to Phe (TCC → TTC) in the amino acid sequence deduced from parC. Comparative sequence analysis revealed the possibility of gene transfer between S. agalactiae and another beta-hemolytic streptococcus, Streptococcus difficile.
Streptococcus agalactiae, a beta-hemolytic group B streptococcus, is an important pathogen causing serious neonatal infections characterized by sepsis and meningitis and also maternal infections. S. agalactiae is also associated with bacteremia, endocarditis, skin and tissue infections, and osteomyelitis in nonpregnant persons (13).
Quinolones were introduced into clinical use in the mid-1980s for the treatment of infections. This class of antibiotics had been very effective for infections caused by streptococci. However, from the mid-1990s, there were many reports describing Streptococcus pneumoniae isolates that were resistant to quinolones (1, 3-6, 10, 15, 17). A highly quinolone-resistant strain of S. pyogenes was also reported (16). Fortunately, almost all S. agalactiae isolates remain susceptible to a number of antibiotics (9, 11). S. agalactiae isolates highly resistant to quinolones have not been reported, though one report stated that for some strains of S. agalactiae, ofloxacin and grepafloxacin MICs were slightly increased (8).
From February to December 2002, we isolated quinolone-resistant S. agalactiae strains in Tottori prefecture in Japan. The majority of quinolone resistance has been thought to be due to point mutations in gyrA and parC, in the internal regions called the quinolone resistance-determining region (QRDR). Therefore, we determined the nucleotide sequences and deduced amino acid sequences of gyrA and parC genes including QRDRs in resistant isolates. These sequences were compared with those of susceptible strains of S. agalactiae and other beta-hemolytic streptococci, including Streptococcus dysgalactiae subsp. equisimilis, which causes streptococcal toxic shock syndrome (14).
Case history.
In this study, we used three isolates from three epidemiologically unrelated patients. The first patient was a newborn male of low birth weight who became infected 20 h after birth. S. agalactiae was the predominant organism in nasal discharge, throat swab, and eye discharge. This strain was given reference number 02Z95 (=GTC1966).
The second patient was a 77-year-old male hospitalized due to an acute aortic dissection. In the hospital, he had been receiving intravenous hyperalimentation. After 1 month in the hospital, he was prescribed antibiotics (vancomycin and arbekacin) to cure a methicillin-resistant Staphylococcus aureus infection around the intravenous catheter. S. agalactiae was obtained from a throat swab after 2 months in the hospital. The number of this isolate was 02Z106 (=GTC1967).
The third patient was a 75-year-old female, admitted to the hospital for insertion of tension-free vaginal tape. On admission, S. agalactiae was detected in her urine. The strain was designated 02Z119 (=GTC2001).
We surveyed all medical records for these three patients to determine whether they had received any quinolones; however, we could not find any information.
The susceptibility testing of these isolates were carried out at the clinical laboratory section of the hospital. The MicroScan Walk Away system (Dade Behring Co., Tokyo, Japan) was used to determine the MICs of 33 antimicrobial agents, including 3 penicillins, 12 cephems, 3 aminoglycosides, 3 macrolides, 3 tetracyclines, 1 quinolone (levofloxacin [LVX]), and 1 glycopeptide (vancomycin). The three S. agalactiae isolates were susceptible to all antimicrobial agents used in this study except LVX (MIC > 8 μg/ml). To confirm the resistance to the quinolones, an E-test (AB Biodisk Sweden) was carried out for six classes of fluoroquinolones: LVX, ciprofloxacin, norfloxacin, ofloxacin, fleroxacin, and sparfloxacin. The MICs for the type strain (GTC1234T [=NCTC 8181T]) and three reference strains of S. agalactiae (GIFU10482, GIFU10483, and GIFU10484) were determined (Table 1). However, three clinical isolates (GTC1966, GTC967, and GTC2001) were not inhibited in these tests, confirming that these isolates were multiply highly quinolone-resistant S. agalactiae strains.
TABLE 1.
MICs (E-test) of quinolones for S. agalactiae and mutations in gyrA and parC
| Strain | Status | MIC (μg/ml)a
|
Codon (amino acid) at:
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| LVX | NOR | FLE | SPX | OFX | CIP | Position 81 in gyrA | Position 79 in parC | ||
| GTC1234 | Type strain | 0.5 | 3 | 3 | 0.38 | 1 | 0.38 | TCA (Ser) | TCC (Ser) |
| GIFU10482 | Reference strain | 0.38 | 3 | 3 | 0.38 | 1 | 0.5 | TCA (Ser) | TCC (Ser) |
| GIFU10483 | Reference strain | 0.5 | 4 | 4 | 0.5 | 1.5 | 0.5 | TCA (Ser) | TCC (Ser) |
| GIFU10484 | Reference strain | 0.75 | 6 | 4 | 0.75 | 1.5 | 0.75 | TCA (Ser) | TCC (Ser) |
| GTC1966 | Clinical isolate | >32 | >256 | >256 | >32 | >32 | >32 | TTA (Leu) | TTC (Phe) |
| GTC1967 | Clinical isolate | >32 | >256 | >256 | >32 | >32 | >32 | TTA (Leu) | TTC (Phe) |
| GTC2001 | Clinical isolate | >32 | >256 | >256 | >32 | >32 | >32 | TTA (Leu) | TTC (Phe) |
LVX, levofloxacin; NOR, norfloxacin; FLE, fleroxacin; SPX, sparfloxacin; OFX, ofloxacin; CIP, ciprofloxacin.
To determine the QRDRs of gyrA and parC, we amplified DNA fragments from chromosomal DNA by PCR using previously reported PCR primers for gyrA and parC (16). However, the primers amplified the target fragments from S. pyogenes but not from S. agalactiae strains (GTC1234, GIFU10482, GIFU10483, and GIFU10484). Therefore, we designed new PCR primers from the region common to S. pyogenes and S. agalactiae: GyrA-forward, 5′ GACAAGTGAAATGAAAACGAG (positions 33 to 53); GyrA-reverse, 5′ CGCTCCATTGACTAATAAATTAGG (positions 484 to 507); ParC-forward, 5′ CAAAACATGTCCCTTGAGGA (positions13 to 32); and ParC-reverse, 5′ CTAGCTTTGGGATGATCAATCAT (positions 577 to 599). After confirmation of a single 474- or 586-bp amplification product of gyrA or parC, respectively, on 1% agarose gels, sequences were determined with an automatic sequencer (model 3100; Applied Biosystems) with a dye terminator reaction kit (Applied Biosystems). DNA and protein sequence comparisons were done with DNASIS software (Hitachi Software Co., Yokohama, Japan).
First, we estimated the specificity of our PCR primers using the type strains of several beta-hemolytic streptococci. Subsequently, our primers for both gyrA and parC could amplify the target fragments from the following species: S. agalactiae (GTC1234T [=NCTC 8181T]), Streptococcus pyogenes (GTC262T [=ATCC 12344T]), Streptococcus equi subsp. equi (GTC269T [=NCTC 9682T]), Streptococcus equi subsp. zooepidemicus (GTC542T [=ATCC 43079T]), Streptococcus iniae (GTC244T [=ATCC 29178T]), Streptococcus canis (GTC423T [=ATCC 43496T]), Streptococcus dysgalactiae subsp. dysgalactiae (GTC431T [=NCFB 2023T]), S. dysgalactiae subsp. equisimilis (GTC842T [=NCFB 1356T]), Streptococcus porcinus (GTC543T [=ATCC 43138T]), and Streptococcus difficile (GTC730T [=ATCC 51487T]). All of these species belong to the pyogenic group of the genus Streptococcus (7). The species of the anginosus group are also beta-hemolytic, although our primers did not amplify fragments from the type strain of each species in this group (S. anginosus GTC268T [=NCTC10713T]; Streptococcus intermedius GTC216T [=ATCC27335T]; and Streptococcus constellatus subsp. constellatus GTC221T [=ATCC27823T]). Because the anginosus group is phylogenetically distant from the pyogenic group (7), the sequences of gyrA and parC may be slightly different from those in S. agalactiae and S. pyogenes.
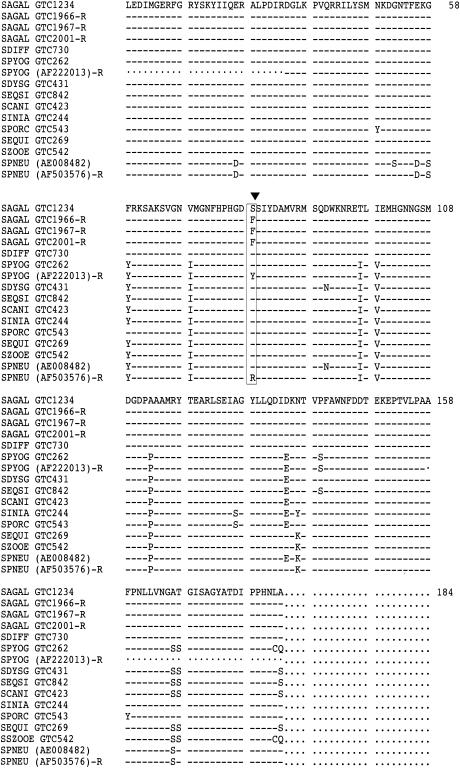
Comparative amino acid sequences deduced from gyrA and parC (including the QRDR) from representative strains of both quinolone-susceptible and -resistant S. agalactiae strains and some other beta-hemolytic streptococci are shown in Fig. 1 and 2, respectively.
FIG. 1.

Comparison of the deduced amino acid sequences of a region of gyrA containing a QRDR from quinolone-susceptible and -resistant strains of S. agalactiae and other beta-hemolytic streptococci. SAGAL, S. agalactiae; SDIFF, S. difficile; SPYOG, S. pyogenes; SDYSG, S. dysgalactiae subsp. dysgalactiae; SEQSI, S. dysgalactiae subsp. equisimilis; SCANI, S. canis; SINIA, S. iniae; SPORC, S. porcinus; SEQUI, S. equi subsp. equi; SZOOE, S. equi subsp. zooepidemicus; SPNEU, S. pneumoniae. “R” following the strain number indicates quinolone resistance. The sequence data for the resistant strain of S. pyogenes (AF222013) and S. pneumoniae (AF503576) were taken from DDBJ. Only amino acids different from those in S. agalactiae GTC1234T are given; dashes indicate amino acid identity, and a dot indicates no sequence information. The amino acids involved in quinolone resistance (▾) are boxed. Quinolone-susceptible strains of S. agalactiae (GIFU10482, GIFU10483, and GIFU10484) shared identical sequences with S. agalactiae GTC1234T.
FIG. 2.
Amino acid sequences deduced from a region of parC containing a QRDR from quinolone-susceptible and -resistant strains of S. agalactiae and other beta-hemolytic streptococci. Symbols and abbreviations are as in Fig. 1.
All four quinolone-susceptible S. agalactiae strains (GTC1234, GIFU10482, GIFU10483, and GIFU10484) shared the same deduced amino acid sequences for the QRDRs of both gyrA and parC. Similarly, three isolates of highly quinolone-resistant strains (GTC1966, GTC1967, and GTC2001) had identical amino acid sequences. However, compared with susceptible strains, these quinolone-resistant S. agalactiae strains carried double point mutations of DNA with the following inferred amino acid substitutions involving the QRDRs of gyrA and parC; Ser-81 to Leu (TCA → TTA) for gyrA and Ser-79 to Phe (codon TCC → TTC) for parC. The mutations at these positions were previously described as contributing to quinolone resistance (4-6, 10, 15-17).
Three major mutation sites have been previously reported for quinolone-resistant streptococci, namely, position 81 in gyrA and positions 79 and 83 in parC. Yokota et al. found that some quinolone-resistant S. pneumoniae strains had other mutations, including Ser-114 to Gly in gyrA and Ser-52 to Gly, Asn-91 to Asp, and Glu-135 to Asp in parC (17). We concluded that these mutations were not related to quinolone resistance, because, as shown in Fig. 1 and 2, many quinolone-susceptible streptococci had the same amino acid sequences.
Surprisingly, S. agalactiae exhibited sequences different from those of other beta-hemolytic streptococci: S. agalactiae strains had Met in position 132 of the gyrA product, whereas all other beta-hemolytic streptococci in this study had Leu (Fig. 1). All beta-hemolytic streptococci and even S. pneumoniae strains have same amino acid at positions 69, 97, 99, and 113 of the parC product (Ile, Ile, Val, and Pro, respectively); however, S. agalactiae strains (seven strains including the type strain) and the type strain of S. difficile have different amino acids (Val, Thr, Ile, and Ala, respectively, at these positions) (Fig. 2). We cannot easily explain why only S. agalactiae and S. difficile have different amino acids at these positions. According to a FASTA homology search (12) on the DDBJ website (http://www.ddbj.nig.ac.jp), there was no more closely related organism than beta-hemolytic streptococci (data not shown). At this time, we do not expect that the genes were transferred from other organisms.
We were also surprised that S. agalactiae and S. difficile shared identical amino acid sequences of QRDRs in both gyrA and parC (Fig. 1 and 2). There were numerous silent nucleotide base substitutions, especially in parC: for example, only two amino acid differences were found between S. equi subsp. equi and S. equi subsp. zooepidemicus, although there were 21 silent base substitutions (data not shown). In the case of S. agalactiae and S. difficile, only one base difference was found. Strains of S. agalactiae have been isolated from homeothermic animals, including humans, whereas S. difficile has been isolated from poikilothermic animals, such as fish (2). Horizontal gene transfer is one possible explanation for the presence of the same sequences in these two species.
Munoz and Campa had reported that parC was the primary target of quinolones in S. pneumoniae (10). In this study we isolated three resistant strains of S. agalactiae, with the same point mutation in both gyrA and parC. We cannot tell which gene is the primary target of the quinolones in S. agalactiae on the basis of our isolates; further study is needed.
Nucleotide sequence accession numbers.
The nucleotide sequences of gyrA and parC for each strain were deposited in DDBJ under the following respective accession numbers: AB101448 and AB101464 for S. agalactiae GTC1234T; AB101449 and AB101465 for S. agalactiae GTC1966; AB101450 and AB101466 for S. agalactiae GTC1967; AB101451 and AB101467 for S. agalactiae GTC2001; AB101452 and AB101468 for S. agalactiae GIFU10482; AB101453 and AB101469 for S. agalactiae GIFU10483; AB101454 and AB101470 for S. agalactiae GIFU10484; AB101455 and AB101471 for S. pyogenes GTC262T; AB101456 and AB101472 for S. dysgalactiae subsp. dysgalactiae GTC431T; AB101457 and AB101473 for S. dysgalactiae subsp. equisimilis GTC842T; AB101458 and AB101474 for S. canis GTC423T; AB101459 and AB101475 for S. iniae GTC244T; AB101460 and AB101476 for S. porcinus GTC543T; AB101461 and AB101477 for S. equi subsp. equi GTC269T; AB101462 and AB101478 for S. equi subsp. zooepidemicus GTC542T; and AB101463 and AB101479 for S. difficilis GTC730T.
REFERENCES
- 1.Brueggemann, A. B., S. L. Coffman, P. Rhomberg, H. Huynh, L. Almer, A. Nilius, R. Flamm, and G. V. Doern. 2002. Fluoroquinolone resistance in Streptococcus pneumoniae in United States since 1994-1995. Antimicrob. Agents Chemother. 46:680-688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hardie, J. M., and R. A. Whiley. 1995. The genus Streptococcus, p. 55-124. In B. J. B. Wood and W. H. Holzapfel (ed.), The genera of lactic acid bacteria. Blackie Academic & Professional, Glasgow, United Kingdom.
- 3.Hooper, D. C. 2002. Fluoroquinolone resistance among Gram-positive cocci. Lancet Infect. Dis. 2:530-538. [DOI] [PubMed] [Google Scholar]
- 4.Janoir, C., V. Zeller, M. D. Kitzis, N. J. Moreau, and L. Gutmann. 1996. High-level fluoroquinolone resistance in Streptococcus pneumoniae requires mutations in parC and gyrA. Antimicrob. Agents Chemother. 40:2760-2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jorgensen, J. H., L. M. Weigel, M. J. Ferraro, J. M. Swenson, and F. C. Tenover. 1999. Activities of newer fluoroquinolones against Streptococcus pneumoniae clinical isolates including those with mutations in the gyrA, parC, and parE loci. Antimicrob. Agents Chemother. 43:329-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jorgensen, J. H., L. M. Weigel, J. M. Swenson, C. G. Whitney, M. J. Ferraro, and F. C. Tenover. 2000. Activities of clinafloxacin, gatifloxacin, gemifloxacin, and trovafloxacin against recent clinical isolates of levofloxacin-resistant Streptococcus pneumoniae. Antimicrob. Agents Chemother. 44:2962-2968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kawamura, Y., X. G. Hou, F. Sultana, H. Miura, and T. Ezaki. 1995. Determination of 16S rRNA sequences of Streptococcus mitis and Streptococcus gordonii and phylogenetic relationships among members of the genus Streptococcus. Int. J. Syst. Bacteriol. 45:406-408. [DOI] [PubMed] [Google Scholar]
- 8.Leven, M., W. Goossens, S. De Wit, and H. Goossens. 2000. In vitro activity of gemifloxacin compared with other antimicrobial agents against recent clinical isolates of streptococci. J. Antimicrob. Chemother. 45(Suppl. S1):51-53. [DOI] [PubMed] [Google Scholar]
- 9.Matsumbara, K., Y. Nishiyama, K. Katayama, G. Yamamoto, M. Sugiyama, T. Murai, and K. Baba. 2001. Change of antimicrobial susceptibility of group B streptococci over 15 years in Japan. J. Antimicrob. Chemother. 48:579-582. [DOI] [PubMed] [Google Scholar]
- 10.Munoz, R., and A. G. De La Campa. 1996. ParC subunit of DNA topoisomerase IV of Streptococcus pneumoniae is a primary target of fluoroquinolones and cooperates with DNA gyrase A subunit in forming resistance phenotype. Antimicrob. Agents Chemother. 40:2252-2257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murdoch, D. R., and L. B. Reller. 2001. Antimicrobial susceptibilities of group B streptococci isolated from patients with invasive disease: 10-year perspective. Antimicrob. Agents Chemother. 45:3623-3624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pearson, W. R., and D. J. Lipman. 1988. Improved tools for biological sequence comparison. Proc. Natl. Acad. Sci. USA 85:2444-2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruoff, K. L., R. A. Whiley, and D. Beighton. 1999. Streptococcus, p. 283-296. In P. R. Murray, E. J. Baron, H. A. Pfaller, F. C. Tenover, and R. H. Yolken (ed.), Manual of clinical microbiology, 7th ed. ASM Press, Washington, D.C.
- 14.Sachse, S., P. Seidel, D. Gerlach, E. Gunther, J. Rodel, E. Straube, and K. H. Schmidt. 2002. Superantigen-like gene(s) in human pathogenic Streptococcus dysgalactiae subsp. equisimilis: genomic localisation of the gene encoding streptococcal pyrogenic exotoxin G (speGdys). FEMS Immunol. Med. Microbiol. 34:159-167. [DOI] [PubMed] [Google Scholar]
- 15.Weigel, L. M., G. J. Anderson, R. R. Facklam, and F. C. Tenover. 2001. Genetic analyses of mutations contributing to fluoroquinolone resistance in clinical isolates of Streptococcus pneumoniae. Antimicrob. Agents Chemother. 45:3517-3523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yan, S. S., M. L. Fox, S. M. Holland, F. Stock, V. J. Gill, and D. P. Fedorko. 2000. Resistance to multiple fluoroquinolones in a clinical isolate of Streptococcus pyogenes: identification of gyrA and parC and specification of point mutations associated with resistance. Antimicrob. Agents Chemother. 44:3196-3198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yokota, S., K. Sato, O. Kuwahara, S. Habadera, N. Tsukamoto, H. Ohuchi, H. Akizawa, T. Himi, and N. Fujii. 2002. Fluoroquinolone-resistant Streptococcus pneumoniae strains occur frequently in elderly patients in Japan. Antimicrob. Agents Chemother. 46:3311-3315. [DOI] [PMC free article] [PubMed] [Google Scholar]


