Abstract
During exercise, defects in calcium (Ca2+) release have been proposed to impair muscle function. Here, we show that during exercise in mice and humans, the major Ca2+ release channel required for excitation–contraction coupling (ECC) in skeletal muscle, the ryanodine receptor (RyR1), is progressively PKA-hyperphosphorylated, S-nitrosylated, and depleted of the phosphodiesterase PDE4D3 and the RyR1 stabilizing subunit calstabin1 (FKBP12), resulting in “leaky” channels that cause decreased exercise tolerance in mice. Mice with skeletal muscle-specific calstabin1 deletion or PDE4D deficiency exhibited significantly impaired exercise capacity. A small molecule (S107) that prevents depletion of calstabin1 from the RyR1 complex improved force generation and exercise capacity, reduced Ca2+-dependent neutral protease calpain activity and plasma creatine kinase levels. Taken together, these data suggest a possible mechanism by which Ca2+ leak via calstabin1-depleted RyR1 channels leads to defective Ca2+ signaling, muscle damage, and impaired exercise capacity.
Keywords: muscle fatigue, calcium channel, calstabin, exitation–contraction coupling, rycals
Skeletal muscle contraction is activated by sarcoplasmic reticulum (SR) Ca2+ release via the type 1 skeletal muscle ryanodine receptor (RyR1). Depolarization of the transverse (T)-tubule membrane activates the dihydropyridine receptor voltage sensor (Cav1.1) that in turn activates RyR1 channels via a direct protein–protein interaction causing the release of SR Ca2+ stores. Ca2+ binds to troponin C allowing actin-myosin cross-bridging to occur and sarcomere shortening. RyR1 Ca2+ release channels are composed of macromolecular complexes consisting of a homotetramer of 560-kDa RyR1 subunits that form scaffolds for proteins that regulate channel function including protein kinase A (PKA) and the phosphodiesterase PDE4D3 (both of which are targeted to the channel via the anchoring protein mAKAP) PP1 (targeted via spinophilin) and calstabin1 (FKBP12) (1, 2).
The binding of calstabin1 to RyR1 stabilizes the closed state of the channel (i.e., prevents a “leak” through the channels) and facilitates coupled gating between neighboring channels that enhances the Ca2+ transient (1, 3). Pharmacologic depletion of calstabin1 from RyR1 (with rapamycin or FK506, both of which bind to calstabin1 and dissociate it from the RyR1 macromolecular complex) uncouples channels from their neighbors and causes a “leak” in the channels (1, 3) and, in intact skeletal muscle, can cause a loss of depolarization-induced contraction (4). Mutation of RyR1 resulting in the loss of calstabin1 binding causes impaired ECC with reduced maximal voltage-gated SR Ca2+ release without affecting the SR Ca2+ store content (5). Genetic deletion of FKBP12 (calstabin1) in mice induced no gross histological or developmental defect in skeletal muscle, although severe developmental cardiac defects were observed that precluded detailed assessment of skeletal muscle function (6). Skeletal muscle-specific knockout of FKBP12 (calstabin1) resulted in reduced voltage-gated SR Ca2+ release (7). In extensor digitorum longus (EDL), reduced maximal tetanic force and a rightward shift in force-frequency relationships were observed however no alteration in SR Ca2+ content or release was reported (7). These data led to the hypothesis that calstabin1 modulates the gain of ECC in fast-twitch skeletal muscle.
PKA phosphorylation at RyR1-S2844 dissociates calstabin1 from the channel and increases its activity (8). RyR1-S2844A mutant channels could not be PKA phosphorylated and did not show the same PKA-dependent increase in open probability. An RyR1-S2844D mutation mimicked PKA phosphorylation of the channel with an increased open probability (8). PDE4D3 colocalizes with RyR1 and RyR2 and controls the local cAMP concentration through degradation (2, 9). The role of PKA phosphorylation of RyR1 remains controversial, however, because other groups have found little or no effect on channel function (10). In vitro S-nitrosylation of unidentified cysteine residue(s) on RyR1 reduces the affinity of calstabin1 for RyR1 (11). RyR1-Cys-3635 and RyR1-Cys-2327 have been suggested to be endogenously modified (12, 13).
SR Ca2+ leak has been documented as aberrant calcium sparks in myofibers after intense exercise and in a model of muscular dystrophy (14). We have found that chronic activation of the sympathetic nervous system (SNS) during heart failure is associated with early skeletal muscle fatigue and PKA hyperphosphorylation of RyR1 at Ser-2844 (meaning that, on average, three to four of the four PKA sites in each homotetrameric channel are PKA phosphorylated in heart failure skeletal muscle), calstabin1 depletion from the RyR1 complex, and a gain-of-function channel defect (8). RyR1 dysfunction in skeletal muscle leads to altered local subcellular Ca2+ release events (15). We have further shown that JTV519, a 1,4-benzothiazepine that causes rebinding of calstabins to RyRs, administered in a rodent model of postmyocardial infarction heart failure, resulted in improved skeletal muscle function (16). We propose that remodeling of the RyR1 channel complex causes leaky channels and is a previously uncharacterized mechanism that regulates exercise capacity.
Results
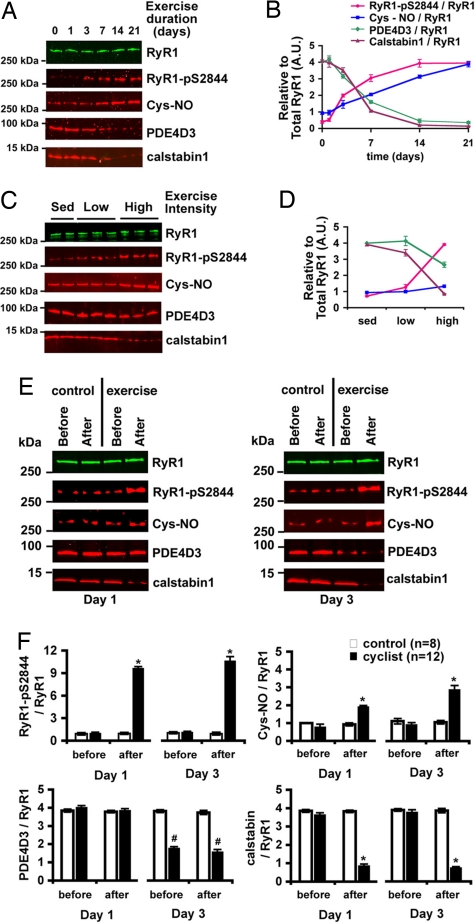
To achieve uniform exercise, mice were placed in a pool and induced to swim twice daily for 3 weeks. After exercise, RyR1 was immunoprecipitated from hind-limb muscle homogenates and immunoblotted for channel complex components. Repeated exercise in the mouse resulted in progressive PKA phosphorylation of RyR1 at Ser-2844 that saturated by 14 days of twice-daily swimming for 90 min (Fig. 1A), and there was a significant increase in S-nitrosylation of free cysteines on RyR1 (Fig. 1A). In addition, the RyR1 macromolecular complex underwent remodeling, characterized by depletion of calstabin1 and PDE4D3 from the channel by day 14 (Fig. 1 A and B). A similar pattern of biochemical changes was seen in the EDL, soleus, tibialis anterior, gastrocnemius, and vastus muscles (data not shown). Only high-intensity exercise resulted in significant channel remodeling (Fig. 1 C and D). RyR1 remodeling persisted after exercise and recovered only partially after 3 days of rest [supporting information (SI) Fig. 5A]. PKA hyperphosphorylation of RyR1 was not due to changes in the amount of PKA or PP1 bound to the RyR1 complex (SI Fig. 5 A and B). Isolated EDL muscle strength was depressed after weeks of exercise, although it was able to recover over several days of rest (SI Fig. 5C). No significant histological evidence of muscle damage was apparent at the light microscopic level in EDL from WT mice following this exercise protocol (SI Fig. 5D). Total calstabin1 levels in whole-muscle homogenate, measured by immunoblot, were not altered during exercise (SI Fig. 5E). Twenty-one days of exercise resulted in an increase in endothelial nitric oxide synthase (eNOS) in EDL muscle (SI Fig. 5F) consistent with previous reports (17), which is a potential cause of increased S-nitrosylation of RyR1. Thus, fatiguing exercise over weeks causes PKA hyperphosphorylation, and S-nitrosylation of RyR1 and remodeling of the RyR1 complex manifested by depletion of PDE4D3 and calstabin1 from the channel.
Fig. 1.
The RyR1 macromolecular complex undergoes remodeling during repeated exercise. (A) RyR1 complex in EDL muscle after exercise (twice daily swimming) analyzed by immunoprecipitation and immunoblotting for RyR1, RyR1-pS2844, cysteine S-nitrosylation of RyR1 (Cys-NO), and PDE4D3 and calstabin1 bound to the receptor. (B) Densitometric quantification of A, where each value is relative to the total RyR1 immunoprecipitated. RyR1 levels did not significantly change under any exercise condition. (C) Composition of the RyR1 complex in EDL muscle after low-intensity (swimming 15 min twice daily) and high-intensity (90 min twice daily) exercise for 5 days. (D) Densitometric quantification of C. (E) Immunoblot of the RyR1 complex immunoprecipitated from 100 μg of muscle homogenate from individual human thigh biopsies before and after exercise on days 1 and 3 of a cycling protocol (3 h at 70% VO2 max). Control cyclists sat in the exercise room but did not exercise. (F) Quantification by densitometry of E. Bar graphs depict PKA phosphorylation, S-nitrosylation, and PDE4D3, and calstabin1 levels in the RyR1 complex normalized to total RyR1 from control (n = 6) and exercise (n = 12) biopsies on each day. All data are mean ± SEM; *, P < 0.01 after exercise versus before; #, P < 0.01 exercise versus control. In all cases, the product of a single RyR1 immunoprecipitation was separated on a 4–20% gradient polyacrylamide gel, transferred, and probed for both total RyR1 and one or more of the modifications noted. The blots shown are representative of three or more independent experiments.
To assess whether remodeling of the RyR1 channel macromolecular complex observed in exercised mice occurs in humans, thigh muscle biopsies were obtained from trained athletes before and after near-maximum aerobic exercise (Fig. 1E) (18). Exercise resulted in PKA hyperphosphorylation of RyR1, RyR1 S-nitrosylation, and calstabin1 depletion (n = 12 exercise) compared with controls (n = 6) (Fig. 1F). Before exercise on day 3, PKA phosphorylation of RyR1 in the trained cyclists was at or near resting levels, and no significant calstabin1 depletion from the RyR1 complex was observed; however, PDE4D3 was partially depleted from the RyR1 (Fig. 1F). These data suggest that similar remodeling of the RyR1 channel complex observed in mice occurs in highly trained athletes subjected to intense exercise.
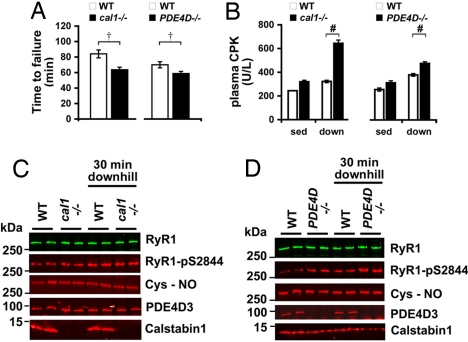
We observed a significant defect in the exercise capacity of both muscle-specific cal1−/− mice and PDE4D−/− mice (predisposed to leaky PKA hyperphosphorylated RyR1 channels) compared with WT littermate controls (Fig. 2A). There was no correlation between exercise capacity and body weight (SI Fig. 6). Twenty-four hours after a downhill exercise regimen (see Materials and Methods for details), creatine phosphokinase (CPK) was significantly elevated consistent with increased muscle damage in both the cal1−/− and PDE4D−/− mice compared with WT (Fig. 2B). Interestingly, after several weeks of daily exercise training, the exercise capacity of WT mice approached that of cal1−/−, presumably because of the progressive depletion of calstabin1 from the RyR1 complex due to PKA hyperphosphorylation of RyR1 that occurs with repeated exercise in WT mice (e.g., Fig. 1). PDE4D−/− mice exhibited a significant increase in calstabin1 depletion from RyR1 after mild exercise (Fig. 2D). Thus, muscle-specific calstabin1- and PDE4D-deficient mice exhibited impaired exercise capacity.
Fig. 2.
Muscle-specific cal1−/− and PDE4D−/− mice have impaired exercise capacity. (A) Treadmill running times of 2-month-old cal1−/− (n = 17) mice and WT (n = 12) littermates and PDE4D−/− (n = 6) mice and WT (n = 6) littermates. (B) Plasma creatine kinase (CPK) levels at rest and after a single downhill eccentric treadmill run (n = 4 mice, in triplicate, at each condition). (C and D) RyR1 immunoprecipitated from EDL muscle from cal1−/− (C) and PDE4D−/− (D) mice and immunoblotted for RyR, RyR1-pS2844, Cys-NO, PDE4D3, and calstabin1. Data presented as mean ± SEM; †, P < 0.05, Wilcoxon rank-sum test; #, P < 0.01, unpaired t test. sed, sedentary; down, downhill.
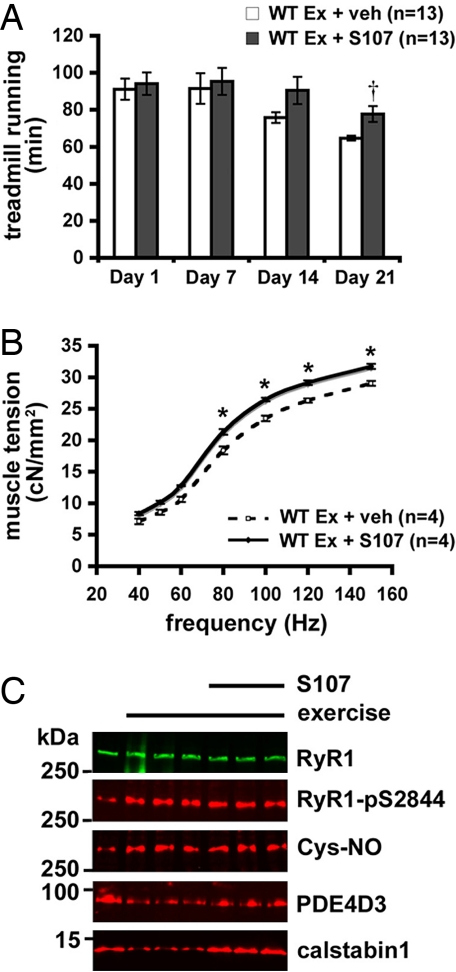
We tested the effect of a drug the prevents depletion of calstabin1 from the RyR1 complex on exercise capacity. Derivatives of JTV519, a 1,4-benzothiazepine, were screened to identify compounds that enhance the binding affinity of calstabin1 to PKA phosphorylated and/or S-nitrosylated RyR, are specific for RyR1 (e.g., had no significant activity against other ion channels including HERG and voltage-gated Ca2+ channels), and have favorable drug-like properties (e.g., orally available, well absorbed, and stable). One compound that met these criteria, S107 (for synthesis, see SI Scheme 1), was selected (see SI Table 1)
Age- and sex-matched WT mice were randomized for implantation of osmotic pumps containing either S107 or vehicle. Treatment with S107 at 2.5 μg/hr or vehicle was initiated 4 days before the beginning of a 3-week daily swimming protocol. Exercise capacity was assessed once a week using a level treadmill run to exhaustion during the nocturnal cycle of the mouse. Fig. 3A shows that calstabin1 rebinding because of S107 treatment had no acute effect on WT exercise performance, but during daily exercise over 3 weeks, the S107 treated WT mice were relatively protected against a decline in treadmill exercise capacity that occurred in vehicle-treated mice (running time in minutes on day 21: 77.7 ± 4.6 exercise plus S107, n = 13 vs. 64.7 ± 1.4 exercise plus vehicle, n = 13; P < 0.05 Wilcoxon rank-sum test).
Fig. 3.
Pharmacologic prevention of calstabin1 depletion from the RyR1 complex improves in vivo exercise capacity. (A) Time to failure during treadmill assays on indicated days of a 28-day treatment trial with S107. (B) Force–frequency curves of EDL muscle isolated immediately after the 21st day of exercise and isometrically stimulated in an oxygenated muscle bath. Forces (cN) are normalized to muscle cross-sectional area. (C) RyR1 immunoprecipitated from EDL and immunoblotted for RyR, RyR1-pS2844, Cys-NO, PDE4D3, and calstabin1. Data are presented as mean ± SEM; †, P < 0.05, Wilcoxon rank-sum test WT + S107 vs. WT + vehicle (veh); *, P < 0.05, unpaired t test. ex, exercise.
EDL muscles from S107-treated mice showed increased force production at stimulation frequencies >80 Hz (Fig. 3B). Exercise resulted in PKA phosphorylation and calstabin1 depletion from immunoprecipitated RyR1. Calstabin1 depletion from RyR1 was reversed by S107 treatment (Fig. 3C). S107 did not significantly improve exercise capacity in muscle-specific calstabin1-deficient mice (data not shown). Taken together, these data suggest that reducing SR Ca2+ leak with a drug that inhibits calstabin1 depletion from RyR1 can protect against muscle damage, enhance muscle function, and improve exercise capacity.
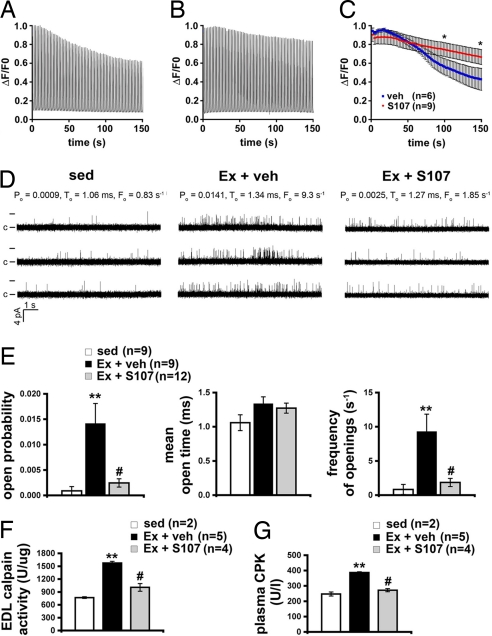
Immediately after the last session of the 3-week swimming/running exercise protocol flexor digitorum brevis (FDB) muscle fibers were enzymatically dissociated and loaded with the Ca2+ indicator fluo-4. Individual muscle fibers were imaged by using a Zeiss LSM 5 Live confocal microscope during field stimulation at 1 Hz and during a fatiguing protocol consisting of repeated 300-ms-long 120-Hz tetani every 2 seconds for 200 seconds. Representative calcium ΔF/F0 traces during the fatiguing stimulation protocol are shown for a FDB fiber isolated from a vehicle- (Fig. 4A) and S107-treated mouse (Fig. 4B). FDB fibers from S107-treated mice exhibited a delayed decline in peak tetanic Ca2+ transients (Fig. 4C). Muscle fibers with slower kinetics of Ca2+ release and reuptake are less prone to fatigue. Therefore, we also assessed the kinetics of Ca2+ release and reuptake during single twitches at 1 Hz. The distribution of 50% reuptake times (τ) showed no significant differences between vehicle and S107 treatment (SI Fig. 7), indicating no shift in the Ca2+ reuptake kinetics of the FDB fibers. These data indicate that treatment with S107 improves Ca2+ handling in muscle fibers and reduces muscle fatigue.
Fig. 4.
Stabilization of RyR1 channels slows muscle fatigue and reduces damage. (A) Representative trace of fluorescence (ΔF/F0) from a vehicle-treated FDB fiber loaded with fluo-4 normalized to the peak during repeated 300-ms, 120-Hz field-stimulated tetani at 0.5 Hz. Isolated cells were continuously perfused with Hepes-buffered Tyrodes solution at room temperature. (B) Representative (ΔF/F0) Ca2+ tetanic trace from an S107-treated FDB fiber. (C) Mean peak tetanic Ca2+ normalized to the peak during fatiguing stimulation (n = 6, vehicle; n = 9, S107). *, P < 0.05 unpaired t test. (D) Representative traces of RyR1 channel activity at 90 nM [Ca2+]cis from sedentary mice (sed, Left), mice exercised and treated with vehicle (Ex + veh, Center), and mice exercised and treated with S107 (Ex + S107, Right). Single channel openings are plotted as upward deflections; the open and closed (c) states of the channel are indicated by horizontal bars at the beginning of the traces. Channel open probability (Po), mean open time (To) and frequency of openings (Fo) are shown above each group of traces and represent average values from all experiments. (E) Average values of Po (Left), To (Center), and Fo (Right) of RyR1 from sedentary mice (sed, n = 9) and exercised mice treated either with vehicle (Ex + veh, n = 9) or S107 (Ex + S107, n = 12). (F) Calpain activity levels in EDL homogenates. (G) Plasma creatine kinase (CPK) activity levels in sedentary and exercised mice with, and without, calstabin1 rebinding with S107. Data are presented as mean ± SEM; **, P < 0.01 compared with sed; #, P < 0.01 compared with Ex + veh.
To determine whether the biochemical changes in the RyR1 macromolecular complex identified during exercise result in changes in RyR1 channel activity, single-channel function of RyR1 in SR microsomes from the hind-limb muscle of sedentary mice (sed), mice repeatedly exercised and treated with vehicle (Ex + veh), and mice repeatedly exercised and treated with S107 (Ex + S107) were determined in planar lipid bilayers. RyR1 channels were continuously measured for at least 10 min at 90 nM [Ca2+]cis (Fig. 4D). Channels from exercised mice treated with vehicle displayed significantly higher open probabilities compared with channels from sedentary mice (P < 0.01, t test, Ex + veh, n = 9 vs. sed, n = 9) (Fig. 4E) or compared with those treated with S107 (P < 0.005, t test, Ex + S107, n = 12 vs. Ex + veh, n = 9). Thus, RyR1 channels from exercised animals, exhibited “leaky” channel behavior (increased open probability) and channels from animals treated with S107 were not leaky.
Ca2+ released into the cytosol via leaky RyR1 channels may activate calpain, Ca2+-dependent neutral proteases (19, 20). After repeated exercise, EDL muscle exhibited elevated calpain activity compared with sedentary controls, whereas calpain activity was significantly reduced in S107-treated mice (Fig. 4F). Evidence of protection against muscle damage was further provided by measurement of plasma CPK activity levels that were elevated in the exercised mice, but reduced close to the levels observed in sedentary controls in the S107-treated mice (Fig. 4G).
Discussion
Our data suggest that remodeling of the RyR1 macromolecular complex during exercise, consisting of PKA hyperphosphorylation at Ser-2844, RyR1 S-nitrosylation, PDE4D3 depletion, and calstabin1 depletion, likely plays a role in determining exercise capacity. Exercise promotes numerous positive effects, from improvement in cardiovascular performance to increased glucose uptake and normalization of fuel metabolism (21, 22). On the other hand, exhausting exercise, such as that performed by a marathon runner or a long-distance cyclist, results in significant muscle damage and can impair task performance for days or weeks (23–25), although the mechanisms underlying this impairment in exercise capacity are not understood.
We identified biochemical changes in the RyR1 macromolecular complex consistent with leaky RyR1/Ca2+ release channels. Both muscle-specific deficiency of calstabin1 (cal1−/−) or PDE4D3 (PDE4D−/−) resulted in exercise defects in mice linking the observed remodeling of the RyR1 complex, characterized by calstabin1 and PDE4D3 depletion from the RyR1 complex, to impaired exercise performance. The Ca2+ channel stabilizer S107, which preserves binding of calstabin1 to RyR1 during exercise, improved exercise capacity in WT but not in cal1−/− mice, demonstrating that the drug's mechanism of action requires calstabin1.
We propose that SR Ca2+ leak via RyR1 channels could result in muscle damage during intense exercise by activating calpain. Indeed, calpain activation and CPK levels were elevated after exercise and were reduced significantly by treatment with S107, suggesting that correction of leaky RyR1 may protect against muscle damage during exercise (Fig. 4). Our data do not exclude the possibility that other Ca2+-dependent pathways such as caspases, contribute to the damage induced by leaky RyR1 channels.
In summary, during exercise, remodeling of the RyR1 macromolecular complex results in leaky channels (because of depletion of calstabin1 from the channel complex) that play a role in limiting exercise capacity. The same physiological mechanisms that impair exercise capacity during chronic exercise are likely beneficial during acute exercise (including PKA phosphorylation and S-nitrosylation of RyR1, both of which activate the channel and may increase ECC gain).
Materials and Methods
Synthesis of S107.
S107 was synthesized according to a previously described method (26) and fully characterized for specificity for RyR (see SI Methods).
Animals and Drug Delivery.
Muscle-specific cal1−/− (7) and PDE4D−/− (27) mice were generously provided by S. Hamilton (Baylor College of Medicine, Houston) and M. Conti (Stanford University, Stanford, CA), respectively. Eight-week-old, weight-matched, C57BL/6J littermate mice were randomized to dosing with either S107 or vehicle (H2O) as described in SI Methods. All experiments were conducted in accord with protocols approved by the Institutional Animal Care and Use Committee of Columbia University.
Exercise Models.
A combined daily swimming and once-weekly treadmill running protocol was used to achieve uniform daily exercise and to assess exercise capacity as described in SI Methods.
Human Exercise Protocol.
The human exercise study was approved by the institutional review board (IRB) of Appalachian State University, and the IRB of Columbia University approved the use of muscle biopsies. Briefly, human subjects underwent an intensive cycling protocol consisting of three consecutive days of cycling for 3 hours at 70% VO2max (18). See SI Methods for details.
Muscle Preparation.
Immediately after the final exercise session, mice were euthanized by carbon dioxide inhalation and cervical dislocation, and tissues were isolated for analysis including isometric force and Ca2+ measurements.
Single-Channel Recording and Data Acquisition.
SR vesicles from skeletal muscle of sedentary mice and mice repeatedly exercised and treated with either vehicle or S107 were prepared as described (8), and RyR1 single-channel measurements were performed by using planar lipid bilayers as described (1) (see also SI Methods for details).
Analysis of Ryanodine Receptor Complex.
Immunoprecipitation and analysis of the RyR1 complex was as described (2, 28) and detailed in SI Methods.
Analyses of Calpain Activity and Creatine Phosphokinase Levels.
Tissue calpain activity (Calbiochem) and plasma creatine phosphokinase levels (Pointe Scientific) were measured by using standard kits. For details see SI Methods.
Statistics.
Data are presented as mean ± SEM. An independent t test with a significance level of 0.05 was used to test differences between cal1−/− and WT, and PDE4D−/− and WT. To test differences in single-channel properties between sedentary, Ex + veh, and Ex + S107, a Bonferroni adjustment for multiple comparisons was used, and a pairwise significance level of 0.015 was used. The distributions of treadmill running-time data were found in several cases to be asymmetric. Therefore, Wilcoxon rank sum tests were used to compare treadmill running data with a significance level of 0.05.
Supplementary Material
ACKNOWLEDGMENTS.
We thank Susan Hamilton (Baylor College of Medicine, Houston), for muscle-specific FKBP12 (calstabin1)-deficient mice and helpful discussions and Bi-Xing Chen and Chiso Nwokafor for technical assistance. This work was supported by a grant from the Defense Advanced Research Projects Agency and an American Heart Association Scientist Development grant (to S.E.L.). A.R.M. and S.R. are consultants for a start-up company, ARMGO Pharma, Inc., that is targeting RyR1 to improve exercise capacity.
Footnotes
Conflict of interest statement: A.R.M. and D.W.L. are on the scientific advisory board and own shares in ARMGO Pharma, Inc., a start-up company that is developing RyR targeted drugs for clinical use in the treatment of heart failure and sudden death. S.R. is a consultant for ARMGO Pharma, Inc.
This article contains supporting information online at www.pnas.org/cgi/content/full/0711074105/DC1.
References
- 1.Brillantes AB, et al. Stabilization of calcium release channel (ryanodine receptor) function by FK506-binding protein. Cell. 1994;77:513–523. doi: 10.1016/0092-8674(94)90214-3. [DOI] [PubMed] [Google Scholar]
- 2.Marx SO, et al. Phosphorylation-dependent regulation of ryanodine receptors: A novel role for leucine/isoleucine zippers. J Cell Biol. 2001;153:699–708. doi: 10.1083/jcb.153.4.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marx SO, Ondrias K, Marks AR. Coupled gating between individual skeletal muscle Ca2+ release channels (ryanodine receptors). Science. 1998;281:818–821. doi: 10.1126/science.281.5378.818. [DOI] [PubMed] [Google Scholar]
- 4.Lamb GD, Stephenson DG. Effects of FK506 and rapamycin on excitation–contraction coupling in skeletal muscle fibres of the rat. J Physiol. 1996;494:569–576. doi: 10.1113/jphysiol.1996.sp021514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Avila G, Lee EH, Perez CF, Allen PD, Dirksen RT. FKBP12 binding to RyR1 modulates excitation–contraction coupling in mouse skeletal myotubes. J Biol Chem. 2003;278:22600–22608. doi: 10.1074/jbc.M205866200. [DOI] [PubMed] [Google Scholar]
- 6.Shou W, et al. Cardiac defects and altered ryanodine receptor function in mice lacking FKBP12. Nature. 1998;391:489–492. doi: 10.1038/35146. [DOI] [PubMed] [Google Scholar]
- 7.Tang W, et al. Altered excitation–contraction coupling with skeletal muscle specific FKBP12 deficiency. FASEB J. 2004;18:1597–1599. doi: 10.1096/fj.04-1587fje. [DOI] [PubMed] [Google Scholar]
- 8.Reiken S, et al. PKA phosphorylation activates the calcium release channel (ryanodine receptor) in skeletal muscle: Defective regulation in heart failure. J Cell Biol. 2003;160:919–928. doi: 10.1083/jcb.200211012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lehnart S, et al. Phosphodiesterase 4D deficiency in the ryanodine-receptor complex promotes heart failure and arrhythmias. Cell. 2005;123:25–35. doi: 10.1016/j.cell.2005.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stange M, Xu L, Balshaw D, Yamaguchi N, Meissner G. Characterization of recombinant skeletal muscle (Ser-2843) and cardiac muscle (Ser-2809) ryanodine receptor phosphorylation mutants. J Biol Chem. 2003;278:51693–51702. doi: 10.1074/jbc.M310406200. [DOI] [PubMed] [Google Scholar]
- 11.Aracena P, Tang W, Hamilton S, Hidalgo C. Effects of S-glutathionylation and S-nitrosylation on calmodulin binding to triads and FKBP12 binding to type 1 calcium release channels. Antioxid Redox Signal. 2005;7:870–881. doi: 10.1089/ars.2005.7.870. [DOI] [PubMed] [Google Scholar]
- 12.Stamler JS, Meissner G. Physiology of nitric oxide in skeletal muscle. Physiol Rev. 2001;81:209–237. doi: 10.1152/physrev.2001.81.1.209. [DOI] [PubMed] [Google Scholar]
- 13.Aracena P, Sanchez G, Donoso P, Hamilton SL, Hidalgo C. S-glutathionylation decreases Mg2+ inhibition and S-nitrosylation enhances Ca2+ activation of RyR1 channels. J Biol Chem. 2003;278:42927–44293. doi: 10.1074/jbc.M306969200. [DOI] [PubMed] [Google Scholar]
- 14.Wang X, et al. Uncontrolled calcium sparks act as a dystrophic signal for mammalian skeletal muscle. Nat Cell Biol. 2005;7:525–530. doi: 10.1038/ncb1254. [DOI] [PubMed] [Google Scholar]
- 15.Ward CW, et al. Defects in ryanodine receptor calcium release in skeletal muscle from post-myocardial infarct rats. FASEB J. 2003;17:1517–1519. doi: 10.1096/fj.02-1083fje. [DOI] [PubMed] [Google Scholar]
- 16.Wehrens XH, et al. Enhancing calstabin binding to ryanodine receptors improves cardiac and skeletal muscle function in heart failure. Proc Natl Acad Sci USA. 2005;102:9607–9612. doi: 10.1073/pnas.0500353102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fukai T, et al. Regulation of the vascular extracellular superoxide dismutase by nitric oxide and exercise training. J Clin Invest. 2000;105:1631–1639. doi: 10.1172/JCI9551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nieman DC, et al. Quercetin reduces illness but not immune perturbations after intensive exercise. Med Sci Sports Exercise. 2007;39:1561–1569. doi: 10.1249/mss.0b013e318076b566. [DOI] [PubMed] [Google Scholar]
- 19.Belcastro AN. Skeletal muscle calcium-activated neutral protease (calpain) with exercise. J Appl Physiol. 1993;74:1381–1386. doi: 10.1152/jappl.1993.74.3.1381. [DOI] [PubMed] [Google Scholar]
- 20.Berchtold MW, Brinkmeier H, Muntener M. Calcium ion in skeletal muscle: Its crucial role for muscle function, plasticity, and disease. Physiol Rev. 2000;80:1215–1265. doi: 10.1152/physrev.2000.80.3.1215. [DOI] [PubMed] [Google Scholar]
- 21.Pollock ML, et al. Resistance exercise in individuals with and without cardiovascular disease: Benefits, rationale, safety, and prescription. An advisory from the Committee on Exercise, Rehabilitation, and Prevention, Council on Clinical Cardiology, American Heart Association. Circulation. 2000;101:828–833. doi: 10.1161/01.cir.101.7.828. [DOI] [PubMed] [Google Scholar]
- 22.Goodyear LJ, Kahn BB. Exercise, glucose transport, and insulin sensitivity. Annu Rev Med. 1998;49:235–261. doi: 10.1146/annurev.med.49.1.235. [DOI] [PubMed] [Google Scholar]
- 23.Balnave CD, Thompson MW. Effect of training on eccentric exercise-induced muscle damage. J Appl Physiol. 1993;75:1545–1551. doi: 10.1152/jappl.1993.75.4.1545. [DOI] [PubMed] [Google Scholar]
- 24.O'Reilly KP, et al. Eccentric exercise-induced muscle damage impairs muscle glycogen repletion. J Appl Physiol. 1987;63:252–256. doi: 10.1152/jappl.1987.63.1.252. [DOI] [PubMed] [Google Scholar]
- 25.Komulainen J, Vihko V. Exercise-induced necrotic muscle damage and enzyme release in the four days following prolonged submaximal running in rats. Pflügers Arch. 1994;428:346–351. doi: 10.1007/BF00724517. [DOI] [PubMed] [Google Scholar]
- 26.Wehrens XH, et al. Protection from cardiac arrhythmia through ryanodine receptor-stabilizing protein calstabin2. Science. 2004;304:292–296. doi: 10.1126/science.1094301. [DOI] [PubMed] [Google Scholar]
- 27.Jin SL, Richard FJ, Kuo WP, D'Ercole AJ, Conti M. Impaired growth and fertility of cAMP-specific phosphodiesterase PDE4D-deficient mice. Proc Natl Acad Sci USA. 1999;96:11998–12003. doi: 10.1073/pnas.96.21.11998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marx SO, et al. PKA phosphorylation dissociates FKBP12.6 from the calcium release channel (ryanodine receptor): Defective regulation in failing hearts. Cell. 2000;101:365–376. doi: 10.1016/s0092-8674(00)80847-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.