Abstract
BACKGROUND
Stroke is a leading cause of death and disability, and poses a significant burden of care for those who survive.
OBJECTIVES
To estimate the incidence of hospitalization for stroke and describe the impact of age, sex and comorbidity on in-hospital mortality, length of stay and readmission rates.
METHODS
Health insurance numbers were used to link acute care hospitalizations across Canada in 1999/2000 for stroke patients with no discharges for a stroke within the preceding five years. Patients were followed up for one year from the date of their initial admission.
RESULTS
The numbers of men (15,367) and women (16,740) in the study were similar. The incidence of all types of stroke (International Classification of Diseases, ninth revision, codes 430, 431 and 434/436) for hospitalized men and women was 14.4 per 10,000, with a 15-fold rise from 8.7 for the age group of 45 to 64 years to 131.9 per 10,000 for the age group 80 years and older. For the index episode, stroke patients spent an average of 21.0 days in the hospital, and 18.2% died in the hospital within 28 days. Of those who survived the first episode, 10.3% were readmitted to the hospital within one year with a recurrent stroke, and overall 37.1% were readmitted for any cause (including stroke). Among these stroke patients, hypertension was codiagnosed in 35%; diabetes in 17%; arrhythmia in 15%; ischemic heart disease in 13.6%; and congestive heart failure in 5%.
CONCLUSIONS
Hospital records linked by patient identification can produce more accurate national estimates of patients hospitalized with stroke than any current countrywide surveillance system.
Keywords: Cerebrovascular disorders, Length of stay, Medical record linkage, Mortality
Abstract
CONTEXTE
Les accidents vasculaires cérébraux (AVC) sont une cause importante d’incapacité et de mortalité et exigent beaucoup de soins chez les patients qui y survivent.
BUTS
Évaluer l’incidence des hospitalisations liées aux AVC et déterminer l’incidence de l’âge, du sexe et des maladies concomitantes sur la mortalité intrahospitalière, la durée du séjour et les réadmissions.
MÉTHODE
Nous avons utilisé les numéros d’assurance maladie pour établir un lien entre les hospitalisations de courte durée enregistrées au Canada, en 1999–2000, chez les patients ayant subi un AVC et les absences de congé en raison d’un AVC au cours des cinq années précédentes. Les patients ont fait l’objet d’un suivi de un an à partir de la date de la première hospitalisation.
RÉSULTATS
Les hommes (15 367) et les femmes (16 740) était en nombre comparable dans l’étude. L’incidence des AVC, tous types confondus, selon la Classification internationale des maladies, 9e édition (codes 430, 431 et 434–436), chez les hommes et les femmes hospitalisés était de 14,4 pour 10 000 personnes; toutefois, cette incidence était multipliée par 15 chez les patients âgés, qui passait de 8,7 dans la tranche d’âge de 45 à 64 ans à 131,9 pour 10 000 personnes dans la tranche d’âge de 80 ans et plus. En ce qui concerne l’épisode de référence, les patients ont passé en moyenne 21,0 jours à l’hôpital et 18,2 % d’entre eux sont morts à l’hôpital au cours des 28 premiers jours. Parmi ceux qui ont survécu au premier épisode, 10,3 % ont été hospitalisés de nouveau au cours de l’année qui a suivi pour un autre AVC et, dans l’ensemble, 37,1 % des patients ont été hospitalisés de nouveau pour différentes causes, y compris pour un AVC. Ont été diagnostiqués en même temps que les AVC l’hypertension (35 %), le diabète (17 %), l’arythmie (15 %), une cardiopathie ischémique (13,6 %) et l’insuffisance cardiaque congestive (5 %).
CONCLUSIONS
Les archives hospitalières liées à l’identité des patients peuvent fournir un portrait estimatif plus précis des patients hospitalisés pour un AVC à l’échelle du pays que tout autre système de surveillance actuellement en place au Canada.
In Canada, as in most industrialized countries, cardiovascular diseases are the leading cause of death and disability. In 1999, stroke was responsible for 8.5% of all deaths in women and 5.6% of all deaths in men (1). The overall mortality rate was 47.8 per 100,000 people. For those who survive, stroke becomes a chronic condition and is estimated to be the leading cause of long-term disability in Canadian adults. Prevalence estimates for 2003 suggest that 4.5% of the population 65 years and older had a previous stroke that still affects their life (2). In 2003, a high proportion of patients who had had a stroke reported having activity restrictions (76%) or needing help with daily living (69%), and only 37% reported good or better health.
The economic burden of stroke is substantial. On the basis of hospital separation data and mortality statistics, it is estimated that in 1998, the total cost of stroke in Canada was $2.4 billion (3). Demographic projections suggest that the incidence of stroke will increase (1).
Establishing community surveillance of stroke and related cardiovascular diseases has been a challenge (4–6). In addition to enhancing our understanding of the epidemiology of stroke, monitoring and surveillance are crucial for health care planning, audit and resource management (7,8). A substantial proportion of the total resource expenditure on stroke is incurred during the initial period of hospitalization. The development of acute interventions, such as thrombolytic treatment, as well as the demonstrated efficacy and effectiveness of coordinated multidisciplinary stroke-unit care, define a continuing need for stroke patients to be admitted to the hospital. In turn, this requires accurate statistical data on hospitalized stroke patients.
National surveillance of cerebrovascular disease for the past several years has meant examining trends as they unfold from the vital statistics records and the hospital discharge abstracts. These two sources give reasonable estimates of the death rates and hospitalization use due to various categories of coronary and vascular diseases. These rates are valuable in understanding the costs associated with cerebrovascular disease, but they result from both the incident and recurring cases. It has not been possible to separate rehospitalizations from the initial admission event. National incidence rates have not been available from existing data sources. Strategies are being developed to monitor the impact of stroke care in various provinces across Canada, eg, the Ontario Coordinated Stroke Strategy and the Nova Scotia Integrated Stroke Strategy; however, a sustainable national surveillance system is lacking.
We estimated the incidence of first hospitalizations for cerebrovascular diseases in 1999/2000 by linking the hospitalization records for each stroke patient and removing patients with a prior stroke in the previous five years. This does not determine the total incidence of cerebrovascular diseases because patients who are not hospitalized are not counted. Much follow-up and rehospitalization information (which never existed at the national level before) has become available and provides a better estimate of the incidence of hospitalized stroke events.
METHODS
Data sources
The Canadian Institute for Health Information collects hospital discharge records from most acute care hospitals in Canada. The records contain information abstracted from a patient’s hospital chart. Each record contains demographic information (eg, date of birth, sex and postal code), administrative information (eg, scrambled or unscrambled health insurance numbers, dates of admission and separation) and clinical information (eg, diagnoses). The data are based on the April to March fiscal year. At Statistics Canada, the hospital morbidity file was further edited to facilitate linkage. Birth date, sex and death information in records with the same health insurance number were checked for consistency. The resulting Health Person-Oriented Information Database consists of information on hospital separations (discharges or deaths) for the years 1994/95 to 2000/01.
Definition of stroke
Together, the International Classification of Diseases, ninth revision (ICD-9) codes 430 to 438 describe the total burden of cerebrovascular disease. However, these codes include several nonstroke diagnoses such as nontraumatic extradural and subdural hematoma, hypertensive encephalopathy and asymptomatic cerebrovascular occlusive disease, as well as remote stroke. Consequently, the probability of codes 430 to 438 indicating an acute stroke is low and quite variable between studies (9,10). The accuracy of the ICD-9 for identifying acute stroke can be improved by limiting the number of codes (11). For example, in a Canadian study of hospital separation data restricting the codes from 430–438 to 430, 431, 434 and 436 increased the probability of identifying an acute stroke (12). The present study reports on subarachnoid hemorrhage (430), intracerebral hemorrhage (431), cerebral infarction (434, 436) and acute stroke (430, 431, 434 and 436).
Data linkage and estimation of incidence rates
Discharges where a hospital diagnosis of cerebrovascular disease (ICD-9 430, 431, 434+436 and 430+431+434+436) was the dominant diagnosis were used to identify patients 20 years and older, in 1999/2000. All acute-care hospital separations for these patients were linked together by personal patient health numbers. The linkage was performed across the fiscal years of 1994/95 and 2000/01 and was conducted separately within each province. While the magnitude of the inability to follow a patient across provincial boundaries may not be large for some provinces, it can be significant when examining smaller provinces or more local regions, near a border. The first hospitalization with a diagnosis of cerebrovascular disease during the 1999/2000 fiscal year was considered the start of the ‘index episode’. Patients who had been hospitalized for cerebrovascular disease (430, 431, 434 and 436 in any of the 16 diagnoses) in the five years before their admission in 1999/2000 were excluded (washed out). All remaining stroke patients were then followed up for one year to determine any readmission to a hospital, the length of the hospital stay and in-hospital death. All analyses were done with SAS (version 8.0, SAS Institute, USA).
Other descriptors
The length of stay in the hospital during the index episode included transfers to different acute-care hospitals and was obtained by subtracting the date of admission of the first visit from the last separation date of all the visits that were contiguous with the first visit. The length of time to readmission was the time in days between the admission date of the index episode and the first readmission date after it. The denominator for readmission rates was the number of patients that survived the index episode. The length of time to in-hospital death was calculated from the index admission date.
RESULTS
Incidence of stroke
The initial cohort consisted of 36,835 patients of all ages with a discharge diagnosis including any of ICD-9 430, 431, 434 and 436. A five year retrospective record search to identify previous hospital discharges with a diagnosis of stroke (any of ICD-9 430, 431, 434 and 436) in any of the 16 possible diagnostic coding entries resulted in 4210 previous cases, thus reducing the total number in the cohort with an incident case of stroke by 11.43% to 32,625. The estimate of the incident hospital rate changes the most between the index patients and the first washout year, where almost 4% of the patients are removed due to earlier strokes. Between the fourth and fifth years of washout, there is only a 1% decrease in the number of patients (Appendix 1). Patients between the ages of 70 and 85 years and men were most likely to be removed as the number of washout periods increased. After those outside the age range and those from the territories were removed, 32,448 patients remained.
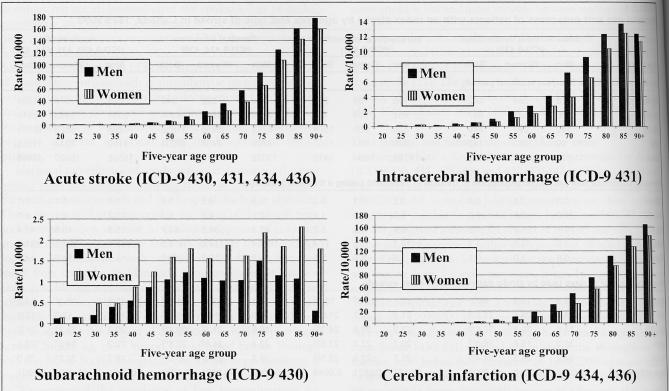
Of the 32,448 strokes that led to a first stroke hospitalization in 1999/2000, 15,528 were for men and 16,920 were for women. The incidence of all acute stroke (ICD-9 430, 431 and 434/436) for hospitalized men and women was 14.4 per 10,000 (Table 1). Incidence rates for cerebral infarction were higher than those for subarachnoid hemorrhage and intracerebral hemorrhage (Table 1). Incidence rates increased with age except for subarachnoid hemorrhage where the pattern was more complex (Figure 1). The incidence of stroke began to rise slowly at approximately 45 years of age for both men and women with an accelerated rise at approximately 70 years of age. There was approximately a 15-fold rise in incidence (from 8.7 to 131.9 per 10,000 people) between the 45 to 64 years age group and the 80 years and older age group in the total population (Table 1). Male rates were higher in every age group except for subarachnoid hemorrhages (ICD-9 430), which were significantly higher in women. Subarachnoid hemorrhages also tended to occur at younger ages.
TABLE 1.
Hospital use and outcomes of patients with an index stroke by age, sex and type of stroke in Canada, 1999/2000
| Subarachnoid hemorrhage (ICD-9 430)
|
Intracerebral hemorrhage (ICD-9 431)
|
Cerebral infarction (ICD-9 434, 436)
|
Acute stroke (ICD-9 430, 431, 434, 436)
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | Men | Women | Both | Men | Women | Both | Men | Women | Both | Men | Women | Both |
|
Incident cases after a five-year washout period | ||||||||||||
| 20–44 | 178 | 264 | 442 | 116 | 84 | 200 | 324 | 322 | 646 | 618 | 670 | 1288 |
| 45–64 | 356 | 531 | 887 | 461 | 304 | 765 | 2716 | 1648 | 4364 | 3533 | 2483 | 6016 |
| 65–79 | 150 | 299 | 449 | 835 | 669 | 1504 | 6283 | 5555 | 11838 | 7268 | 6523 | 13791 |
| ≥80 | 30 | 113 | 143 | 370 | 637 | 1007 | 3709 | 6494 | 10203 | 4109 | 7244 | 11353 |
| Total | 714 | 1207 | 1921 | 1782 | 1694 | 3476 | 13032 | 14019 | 27051 | 15528 | 16920 | 32448 |
|
Hospital incidence rate per 10,000 population in Canada in 1999/2000 (using a five-year washout) | ||||||||||||
| 20–44 | 0.3 | 0.4 | 0.4 | 0.2 | 0.1 | 0.2 | 0.5 | 0.5 | 0.5 | 1.0 | 1.1 | 1.1 |
| 45–64 | 1.0 | 1.5 | 1.3 | 1.3 | 0.9 | 1.1 | 7.9 | 4.7 | 6.3 | 10.2 | 7.1 | 8.7 |
| 65–79 | 1.1 | 1.9 | 1.5 | 6.4 | 4.2 | 5.2 | 47.8 | 34.8 | 40.7 | 55.3 | 40.8 | 47.4 |
| ≥80 | 1.0 | 2.0 | 1.7 | 12.7 | 11.2 | 11.7 | 127.4 | 114.0 | 118.5 | 141.1 | 127.1 | 131.9 |
| Total | 0.6 | 1.0 | 0.9 | 1.6 | 1.5 | 1.5 | 11.8 | 12.1 | 12.0 | 14.1 | 14.7 | 14.4 |
|
Average number of days used by stroke patients within index episode | ||||||||||||
| 20–44 | 18.5 | 19.3 | 19.0* | 12.1 | 20.5† | 15.6‡ | 10.1 | 12.4† | 11.3*‡ | 12.9 | 16.2† | 14.6 |
| 45–64 | 24.6 | 25.4 | 25.0*§ | 21.8 | 19.7 | 21.0‡§ | 15.0 | 15.2 | 15.1*‡ | 16.8 | 17.9 | 17.3 |
| 65–79 | 31.5 | 30.2 | 30.6*§ | 23.3 | 25.6 | 24.3‡§ | 19.6 | 21.3† | 20.4*‡ | 20.2 | 22.2† | 21.2 |
| ≥80 | 28.2 | 15.6 | 18.3*§ | 20.7 | 22.0 | 21.5‡§ | 22.4 | 24.6† | 23.8*‡ | 22.2 | 24.3† | 23.5 |
| Total | 24.7 | 24.3 | 24.4*§ | 21.7 | 22.9 | 22.3‡§ | 19.2 | 21.9† | 20.6*‡ | 19.7 | 22.2† | 21.0 |
| Age difference¶ | 0.0283 | 0.0010 | <0.0001 | 0.0171 | 0.0821 | 0.0048 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
|
Median number of days used by stroke patients within index episode | ||||||||||||
| 20–44 | 12 | 11 | 11.5*§ | 7 | 10† | 7§ | 6 | 7 | 7* | 7 | 9† | 8 |
| 45–64 | 12 | 14 | 13*§ | 9 | 9 | 9§ | 7 | 7 | 7* | 8 | 8 | 8 |
| 65–79 | 14 | 13 | 14*§ | 8 | 10 | 9‡§ | 9 | 10† | 10*‡ | 9 | 10† | 10 |
| ≥80 | 12.5 | 4 | 5*§ | 9 | 11 | 10‡§ | 11 | 13† | 13*‡ | 11 | 13† | 12 |
| Total | 12 | 12 | 12*§ | 8 | 10 | 9‡§ | 8 | 11† | 10*‡ | 9 | 11† | 10 |
| Age difference** | NS | <0.0001 | <0.0001 | NS | NS | NS | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
|
Stroke patients††who were readmitted to the hospital with a stroke diagnosis‡‡within one year from the admission date of their index-episode§§(%) | ||||||||||||
| 20–44 | 3.6 | 5.8† | 4.9*§ | 7.6 | 9.1 | 8.2§ | 9.5 | 5.6† | 7.6* | 7.6 | 6.1† | 6.8 |
| 45–64 | 6.5 | 9.0 | 8.0* | 8.6 | 6.3† | 7.7‡ | 10.9 | 11.6 | 11.1*‡ | 10.2 | 10.6 | 10.4 |
| 65–79 | 11.2 | 9.0 | 9.9* | 11.3 | 11.8 | 11.5 | 11.8 | 11.1 | 11.5* | 11.7 | 11.1 | 11.4 |
| ≥80 | 0.0 | 14.7† | 10.4§ | 10.3 | 7.2† | 8.3‡§ | 10.2 | 8.9† | 9.4‡ | 10.1 | 8.8 | 9.3 |
| Total | 6.4 | 8.4 | 7.6*§ | 10.0 | 9.0 | 9.5‡§ | 11.1 | 10.1† | 10.6*‡ | 10.8 | 9.9† | 10.3 |
| Age difference*** | 0.0764 | 0.0785 | 0.0134 | 0.2211 | 0.8743 | 0.3773 | 0.9103 | 0.1236 | 0.1231 | 0.1125 | 0.8727 | 0.5033 |
|
Stroke patients††readmitted to the hospital for any cause (including any stroke) within one year from the admission date of their index episode (%) | ||||||||||||
| 20–44 | 22.7 | 20.5 | 21.4*§ | 30.4 | 36.4† | 32.9‡§ | 29.8 | 32.3† | 31.1*‡ | 28.1 | 28.3 | 28.2 |
| 45–64 | 26.1 | 23.9 | 24.9*§ | 35.8 | 28.7† | 33.1§ | 31.2 | 35.4† | 32.7* | 31.2 | 32.6† | 31.7 |
| 65–79 | 35.7 | 35.5 | 35.6* | 35.7 | 35.4 | 35.5‡ | 39.8 | 37.7† | 38.8*‡ | 39.4 | 37.5† | 38.5 |
| ≥80 | 42.9 | 38.2† | 39.6§ | 44.9 | 30.5† | 35.7‡§ | 42.4 | 38.7† | 40.0‡ | 42.5 | 38.2† | 39.7 |
| Total | 27.4 | 25.8 | 26.4*§ | 36.7 | 32.5† | 34.7‡§ | 38.2 | 37.7 | 37.9*‡ | 37.6 | 36.6 | 37.1 |
| Age difference*** | 0.0163 | 0.0006 | <0.0001 | 0.0451 | 0.8206 | 0.3209 | <0.0001 | 0.0033 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
|
Stroke patients who died in hospital within 28 days from their index admission date by age, sex and stroke diagnosis (%) | ||||||||||||
| 20–44 | 20.8 | 14.4† | 17.0*§ | 20.7 | 22.6 | 21.5‡§ | 5.9 | 5.0† | 5.4*‡ | 13.0 | 10.9† | 11.9 |
| 45–64 | 17.7 | 23.4† | 21.1*§ | 29.3 | 36.5† | 32.2‡§ | 6.2 | 6.9† | 6.4*‡ | 10.4 | 14.0† | 11.9 |
| 65–79 | 31.3 | 43.5† | 39.4* | 41.9 | 41.1 | 41.6‡ | 11.6 | 12.0 | 11.8*‡ | 15.5 | 16.4† | 16.0 |
| ≥80 | 46.7 | 66.4† | 62.2*§ | 51.1 | 49.5 | 50.1‡§ | 22.2 | 21.8 | 21.9*‡ | 25.0 | 24.9 | 24.9 |
| Total | 22.6 | 30.4† | 27.5*§ | 39.2 | 42.5† | 40.8‡§ | 13.4 | 15.8† | 14.6*‡ | 16.7 | 19.5† | 18.2 |
| Age difference*** | 0.0018 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
Subarachnoid hemorrhage and cerebral infarction percentages significantly different (P<0.05);
Male and female percentages (within each stroke type) significantly different (P<0.05) (Z test for percentages and Wilcoxon two-sample test for medians);
Intracerebral hemorrhage and cerebral infarction percentages significantly different (P<0.05);
Subarachnoid hemorrhage and intracerebral hemorrhage percentages significantly different (P<0.05);
Analysis of variance in a general linear model; **Kruskal-Wallis test for medians;
Denominator population: Those discharged alive after their first episode;
Any visit with a TAB_DIAG=430, 431–438 after the first episode;
Does not have to be the first readmission;
Mantel-Haenszel χ2. ICD-9 International Classification of Diseases, ninth revision. NS Not significant
Figure 1).
Rate of first hospitalization for stroke by age and sex per 10,000 in Canada, 1999/2000. ICD-9 International Classification of Diseases, ninth revision
Hospital use
The mean number of days in the hospital for the incident stroke episode for all stroke patients was 21.0 days (95% CI 20.6 to 21.4). Women had a slightly longer stay (22.2 days, 95% CI 21.7 to 22.7) than men (19.7 days, 95% CI 19.2 to 20.2). Differences were comparable for all types of stroke; however, the length of stay was longest for subarachnoid strokes at 24.7 days (95% CI 21.8 to 27.5) for men and at 24.3 days (95% CI 22.1 to 26.6) for women. The mean number of days for acute stroke increased with age. The median number of days in the hospital for all types of stroke was 10 days (nine days for men and 11 days for women) (Table 1).
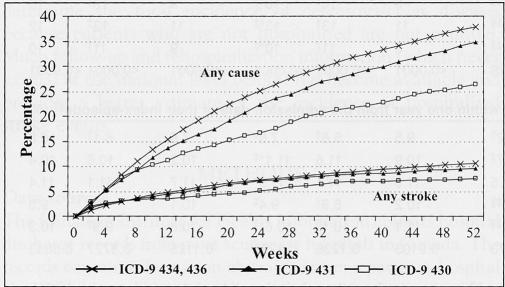
Rehospitalizations were more likely for causes other than that of a recurrent stroke, regardless of the type of incident stroke. Depending on the type of initial stroke, 6% to 10% of patients were readmitted within one year because of a recurrent stroke and from 25% to 37% of patients were readmitted for other causes (Figure 2). The median time to readmission was shorter among patients younger than 80 years for recurrent stroke than for any cause. This difference was more marked in men than women (Table 2). Median times to readmission because of a recurrent stroke or for any cause increased with increasing age. Median times to a recurrent stroke did not differ significantly across the provinces; however, for any cause, there were significant differences (P<0.002) with a median low of 88 days in Alberta to a high of 125 days in British Columbia.
Figure 2).
Cumulative percentage of first rehospitalization for stroke and first rehospitalization for any cause by type of incident stroke in Canada, 1999/2000. Denominator population: Those discharged alive after their first episode. Note: The stroke readmission is not always for the first readmission of the patient. ICD-9 International Classification of Diseases, ninth revision
TABLE 2.
Median time to readmission within one year by cause, age and sex*
| Median time to readmission within one year, any cause
|
Median time to readmission within one year, any stroke
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age (years) | Patients (n) | Median (days) | 25th percentile | 75th percentile | Age (years) | Patients (n) | Median (days) | 25th percentile | 75th percentile |
| 20–44 | 319 | 88 | 29 | 200 | 20–44 | 77 | 47 | 12 | 115 |
| 45–64 | 1667 | 105 | 41 | 204 | 45–64 | 545 | 80 | 28 | 187 |
| 65–79 | 4328 | 116 | 51 | 210 | 65–79 | 1284 | 104 | 39 | 200 |
| ≥80 | 3177 | 108 | 51 | 205 | ≥80 | 743 | 108 | 43 | 205 |
| P<0.00001 | P<0.00001 | ||||||||
| Men | Men | ||||||||
| 20–44 | 151 | 78 | 27 | 201 | 20–44 | 41 | 44 | 10 | 101 |
| 45–64 | 981 | 106 | 40 | 207 | 45–64 | 322 | 70 | 27 | 174 |
| 65–79 | 2349 | 116 | 50 | 208 | 65–79 | 700 | 94 | 30 | 196.5 |
| ≥80 | 1228 | 106 | 52 | 204.5 | ≥80 | 292 | 111 | 46.5 | 198 |
| P<0.01 | P<0.00004 | ||||||||
| Women | Women | ||||||||
| 20–44 | 168 | 95.5 | 31.5 | 199.5 | 20–44 | 36 | 48 | 14 | 154 |
| 45–64 | 686 | 103.5 | 41 | 197 | 45–64 | 223 | 99 | 31 | 196 |
| 65–79 | 1979 | 117 | 53 | 216 | 65–79 | 584 | 112 | 48 | 209 |
| ≥80 | 1949 | 111 | 50 | 205 | ≥80 | 451 | 107 | 40 | 206 |
| P<0.001 | P<0.01 | ||||||||
The population included only those discharged alive after their first episode; the Kruskal-Wallis test was used to test for differences between age groups
Comorbid conditions
Comorbid conditions were prevalent among stroke patients: hypertension was diagnosed in 35% of patients; diabetes in 17% of patients; arrhythmia in 15% of patients; ischemic heart disease in 14% of patients; and congestive heart failure in 5% of patients (Table 3). Both hypertension and diabetes are predisposing factors for the development of a stroke, the former for both occlusive and hemorrhagic strokes, and the latter for an occlusive stroke. Both conditions are preventable or modifiable with control for hypertension having been shown to reduce the risk of a stroke (13).
TABLE 3.
Patients with a comorbidity in the index episode by sex and type of stroke in Canada, 1999/2000
| Subarachnoid hemorrhage (ICD-9 430)
|
Intracerebral hemorrhage (ICD-9 431)
|
Cerebral infarction (ICD-9 434, 436)
|
Acute stroke (ICD-9 430, 431, 434, 436)
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ICD-9 codes | Men (%) | Women (%) | Both (%) | Men (%) | Women (%) | Both (%) | Men (%) | Women (%) | Both (%) | Men (%) | Women (%) | Both (%) | |
| Hypertension | 401, 402, 403, 404, 405 | 17.0 | 24.3* | 21.6†‡ | 43.0 | 41.2 | 42.1†§ | 33.0 | 37.5* | 35.3‡§ | 33.4 | 36.9* | 35.2 |
| Diabetes | 250 | 4.6 | 5.1 | 5.0†‡ | 12.5 | 9.6* | 11.1†§ | 20.9 | 17.5* | 19.1‡§ | 19.2 | 15.8* | 17.4 |
| Arrhythmias | 426, 427 | 7.7 | 6.7 | 7.1†§ | 11.0 | 10.2 | 10.6†§ | 14.8 | 17.6* | 16.3‡§ | 14.1 | 16.1* | 15.1 |
| Ischemic heart disease | 410–414 | 5.2 | 4.5 | 4.7†‡ | 10.4 | 7.7* | 9.1†§ | 16.7 | 13.0* | 14.8‡§ | 15.5 | 11.8* | 13.6 |
| Other stroke | 432, 433, 435, 437, 438 | 16.8 | 21.7* | 19.9†§ | 9.8 | 9.9 | 9.8†§ | 14.4 | 11.0* | 12.7‡§ | 14.0 | 11.7* | 12.8 |
| Congestive heart failure | 428 | 1.3 | 3.2* | 2.5‡ | 2.6 | 3.3 | 2.9§ | 5.0 | 6.1* | 5.6‡§ | 4.6 | 5.6* | 5.1 |
| Peripheral vascular disease | 440–447 | 2.2 | 3.7 | 3.2 | 2.7 | 2.5 | 2.6§ | 4.1 | 3.1* | 3.6§ | 3.8 | 3.1* | 3.4 |
| Diseased heart valve | 394, 395, 396, 397, 398, 424 | 0.1 | 0.7 | 0.5‡ | 0.5 | 1.3* | 0.9§ | 1.7 | 2.5* | 2.1‡§ | 1.5 | 2.3* | 1.9 |
| Myocardial infarct | 410 | 0.8 | 1.4 | 1.2‡ | 2.0 | 1.5 | 1.8 | 1.9 | 1.9 | 1.9‡ | 1.8 | 1.8 | 1.8 |
| Complication of heart disease | 429 | 0.4 | 0.4 | 0.4†‡ | 1.2 | 1.2 | 1.2†§ | 2.2 | 1.6* | 1.9‡§ | 2.0 | 1.6* | 1.7 |
| Atherosclerosis | 440 | 0.7 | 0.8 | 0.7‡ | 1.0 | 0.9 | 1.0§ | 1.7 | 1.3* | 1.5‡§ | 1.6 | 1.2* | 1.4 |
| Cardiomyopathy | 422, 425 | 0.1 | 0.0 | 0.1‡ | 0.3 | 0.2 | 0.3 | 0.7 | 0.4* | 0.5‡ | 0.7 | 0.3* | 0.5 |
| Pulmonary heart disease | 415, 416, 417 | 0.8 | 0.5 | 0.6 | 0.8 | 0.5 | 0.7§ | 0.3 | 0.5* | 0.4§ | 0.4 | 0.5 | 0.5 |
| Alcohol abuse, alcoholism | 3050, 3039 | 1.0 | 0.0* | 0.4 | 0.6 | 0.1* | 0.4§ | 0.3 | 0.1* | 0.2§ | 0.3 | 0.1* | 0.2 |
Male and female percentages (within each stroke type) significantly different (P<0.05) (Z test);
Subarachnoid hemorrhage and intracerebral hemorrhage percentages significantly different (P<0.05);
Subarachnoid hemorrhage and cerebral infarction percentages significantly different (P<0.05);
Cerebral infarction and intracerebral hemorrhage percentages significantly different (P<0.05). ICD-9 International Classification of Diseases, ninth revision
When these comorbid conditions were examined in a logistic regression, age and ‘other stroke’ were the most important predictors for readmission to the hospital within one year. For death during the index episode, age and comorbid cardiovascular conditions, especially myocardial infarction, were the most predictive. Results from a regression analysis indicate that age, diabetes, other stroke, congestive heart failure, myocardial infarction, pulmonary heart disease and alcoholism increased the length of stay of the first episode.
In-hospital mortality
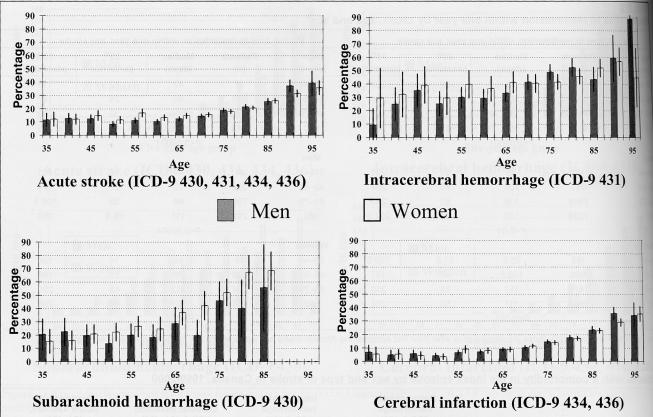
The patient fatality for stroke, defined as death occurring within 28 days of the index stroke, was 16.7% for all patients and both sexes combined. By using the most responsible diagnosis of the last visit (if within 28 days), stroke was estimated to be the cause of all these in-hospital deaths. After approximately 60 years of age, patient fatality increased with age for both men and women (Figure 3). Intracerebral hemorrhage at 40.8% had the highest 28 day patient fatality rate overall (Table 1).
Figure 3.
) Percentage and 95% CI of patients with a first hospitalization for acute stroke who died in hospital within 28 days by age, sex and stroke diagnosis in Canada, 1999/2000. ICD-9 International Classification of Diseases, ninth revision
DISCUSSION
Record linkage of administrative databases provided a convenient and economical estimate of the incidence of stroke in the Canadian population. Provided that the proportion of acute stroke patients not admitted to the hospital is constant over time, following the mortality and the incidence of hospitalized cases by using record linkage methods, provided an expedient means of evaluating the impact of prevention and stroke care.
Several limitations to the present study are acknowledged. First, it should be noted that a hospital readmission after a stroke may be elective (eg, for a procedure), or unanticipated (eg, for an acute problem). The nature of the readmission is not coded in all provinces in Canada; therefore, the rates of urgent or emergent hospitalizations cannot be compared across provinces or regions. Another limitation is the inability to follow a patient across provincial boundaries for procedures and outcomes that occur out of province. While the magnitude of this problem may not be large for some provinces, it can be significant when examining smaller provinces or more local regions, near border.
While analyzing hospital data is a standard method for epidemiological studies, patients with stroke who have not been treated in a hospital are excluded. Thus, our data underestimate the true incidence of stroke by focusing on the more acute and severely symptomatic patients who are hospitalized. Although it is believed that the overwhelming majority of stroke patients are hospitalized, the addition of physician claims data and emergency room data in future studies may challenge this premise (14).
Intra- and interprovincial variations in the coding of hospital discharge data may affect the results, limiting regional comparability (15). Varying error rates in the discharge records were found in a study of California hospitals, resulting in a range from 0.2 to 2.2 expected 30-day deaths per 100 admissions (16). In Australia, incidence rates on the east coast were considerably different from those found in a west coast study, the differences believed to be due to variable inclusion criteria and coding inaccuracies (17). Comparable Canadian studies need to be performed before actual differences in incidence can be declared.
Our washout period of five years may have resulted in an overestimation of the true number of first hospitalizations. However, the decreased yield between the fourth and fifth years appear to introduce an error of 1% or less if continued beyond five years.
Finally, the validity of the medical diagnosis was not examined. Although the diagnosis of stroke itself may be valid, identifying the type of stroke may be less accurate depending on the use of diagnostic technologies (18).
CONCLUSIONS
The record linkage method of using hospital separation data for surveillance purposes is a convenient and feasible tool to monitor cerebrovascular trends. With a longer collection period, our longitudinal hospitalization data could contribute trends of incidence over time, and a longer follow-up period, to the enterprise of national stroke surveillance. Annual reporting of descriptive patterns based on hospital in-patient data, such as reported here, could be part of a national surveillance system. As forthcoming hospital separation databases are linked, a longer washout period will improve the accuracy of estimates of incidence. The present study provides an overview of the recent epidemiology of cerebrovascular disease in Canada, showing that stroke occurrences including incident cases as well as recurrences increase with age, particularly after 70 years. Given the aging of the Canadian population, the burden of stroke is expected to increase. Future studies will examine time trends and more detailed regional differences, if possible, at the level of regional health units. While the ideal surveillance of stroke incidence in Canada has not be carried out and may not even be feasible, at least periodic prospective studies of stroke incidence in a defined Canadian population could be undertaken to provide a measure of the validity of incidence estimates based on linkage of administrative records.
ACKNOWLEDGEMENTS
The authors thank Dr Stephen Phillips, who reviewed an earlier draft of the manuscript and provided invaluable comments and advice
APPENDIX 1
Five year washout history by type of stroke*
| ICD-9 code | Years of washout | Total patients washed out (n) | Patients left (n) | Washed out (%) | Difference (%) |
|---|---|---|---|---|---|
| 430 | Index (0) | 2090 | 0.00 | ||
| One | 76 | 2014 | 3.64 | 3.64 | |
| Two | 89 | 2001 | 4.26 | 0.62 | |
| Three | 104 | 1986 | 4.98 | 0.72 | |
| Four | 112 | 1978 | 5.36 | 0.38 | |
| Five | 117 | 1973 | 5.60 | 0.24 | |
| 431 | Index (0) | 4065 | 0.00 | ||
| One | 261 | 3804 | 6.42 | 6.42 | |
| Two | 353 | 3712 | 8.68 | 2.26 | |
| Three | 416 | 3649 | 10.23 | 1.55 | |
| Four | 480 | 3585 | 11.81 | 1.57 | |
| Five | 514 | 3551 | 12.64 | 0.84 | |
| 434, 436 | Index (0) | 30,958 | 0.00 | ||
| One | 1317 | 29,641 | 4.25 | 4.25 | |
| Two | 2269 | 28,689 | 7.33 | 3.08 | |
| Three | 2910 | 28,048 | 9.40 | 2.07 | |
| Four | 3372 | 27,586 | 10.89 | 1.49 | |
| Five | 3793 | 27,165 | 12.25 | 1.36 | |
| 430, 431, 434, 436 | Index (0) | 36,835 | 0.00 | ||
| One | 1440 | 35,395 | 3.91 | 3.91 | |
| Two | 2497 | 34,338 | 6.78 | 2.87 | |
| Three | 3216 | 33,619 | 8.73 | 1.95 | |
| Four | 3750 | 33,085 | 10.18 | 1.45 | |
| Five | 4210 | 32,625 | 11.43 | 1.25 |
All ages and territories. ICD-9 International Classification of revision
REFERENCES
- 1.Heart and Stroke Foundation of Canada. The Growing Burden of Heart Disease and Stroke in Canada 2003. Ottawa: Heart and Stroke Foundation of Canada; 2003. [Google Scholar]
- 2.Statistics Canada, Health Statistics Division. Canadian Community Health Survey (CCHS) Cycle 2.1 (2003) Ottawa: Statistics Canada; 2003. [Google Scholar]
- 3.Public Health Agency of Canada (PHAC) Economic Burden of Illness in Canada, 1998. Ottawa: Public Works and Government Services Canada; 2002. [Google Scholar]
- 4.Gillum RF. Community surveillance for cardiovascular disease. Methods, problems, applications – a review. J Chronic Dis. 1978;31:87–94. doi: 10.1016/0021-9681(78)90093-0. [DOI] [PubMed] [Google Scholar]
- 5.Bonita R, Beaglehole R, North JD. The long-term monitoring of cardiovascular disease: Is it feasible? Community Health Stud. 1983;7:111–6. doi: 10.1111/j.1753-6405.1983.tb00400.x. [DOI] [PubMed] [Google Scholar]
- 6.Wielgosz AT. Establishing surveillance of cardiovascular disease in Canada. Can J Cardiol. 1992;8:249–51. [PubMed] [Google Scholar]
- 7.Bonita R, Beaglehole R. Monitoring stroke. An international challenge. Stroke. 1995;26:541–2. doi: 10.1161/01.str.26.4.541. [DOI] [PubMed] [Google Scholar]
- 8.Weir N, Dennis MS Scottish Stroke Outcomes Study Group. Towards a national system for monitoring the quality of hospital-based stroke services. Stroke. 2001;32:1415–21. doi: 10.1161/01.str.32.6.1415. [DOI] [PubMed] [Google Scholar]
- 9.Davenport RJ, Dennis MS, Warlow CP. The accuracy of the Scottish Morbidity Record (SMR1) data for identifying hospitalised stroke patients. Health Bull (Edinb) 1996;54:402–5. [PubMed] [Google Scholar]
- 10.Liu L, Reeder B, Shuaib A, Mazagri R. Validity of stroke diagnosis on hospital discharge records in Saskatchewan, Canada: Implications for stroke surveillance. Cerebrovasc Dis. 1999;9:224–30. doi: 10.1159/000015960. [DOI] [PubMed] [Google Scholar]
- 11.Leibson CL, Naessens JM, Brown RD, Whisnant JP. Accuracy of hospital discharge abstracts for identifying stroke. Stroke. 1994;25:2348–55. doi: 10.1161/01.str.25.12.2348. [DOI] [PubMed] [Google Scholar]
- 12.Phillips SJ, Cameron KA, Chung CR. Stroke surveillance revisited. Can J Cardiol. 1993;9(Suppl D):124D–5D. [Google Scholar]
- 13.Straus SE, Majumdar SR, McAlister FA. New evidence for stroke prevention: Scientific review. JAMA. 2002;288:1388–95. doi: 10.1001/jama.288.11.1388. [DOI] [PubMed] [Google Scholar]
- 14.Anderson CS, Jamrozik KD, Burvill PW, Chakera TM, Johnson GA, Stewart-Wynne EG. Ascertaining the true incidence of stroke: Experience from the Perth Community Stroke Study, 1989–1990. Med J Aust. 1993;158:80–4. doi: 10.5694/j.1326-5377.1993.tb137528.x. [DOI] [PubMed] [Google Scholar]
- 15.Yiannakoulias N, Svenson LW, Hill MD, et al. Incident cerebrovascular disease in rural and urban Alberta. Cerebrovasc Dis. 2004;17:72–8. doi: 10.1159/000073903. [DOI] [PubMed] [Google Scholar]
- 16.Green J, Wintfeld N. How accurate are hospital discharge data for evaluating effectiveness of care? Med Care. 1993;31:719–31. doi: 10.1097/00005650-199308000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Thrift AG, Dewey HM, Macdonell RA, McNeil JJ, Donnan GA. Stroke incidence on the east coast of Australia: The North East Melbourne Stroke Incidence Study (NEMESIS) Stroke. 2000;31:2087–92. doi: 10.1161/01.str.31.9.2087. [DOI] [PubMed] [Google Scholar]
- 18.Ellekjaer H, Holmen J, Kruger O, Terent A. Identification of incident stroke in Norway: Hospital discharge data compared with a population-based stroke register. Stroke. 1999;30:56–60. doi: 10.1161/01.str.30.1.56. [DOI] [PubMed] [Google Scholar]