Abstract
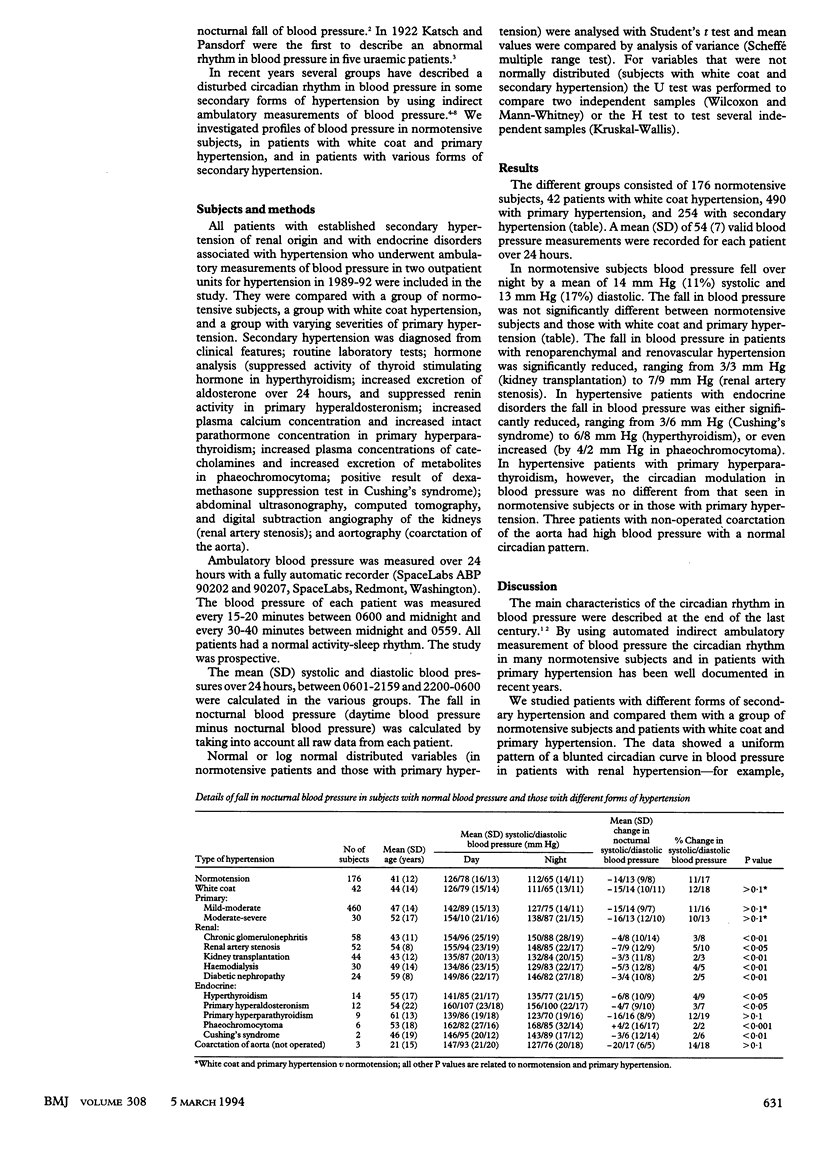
OBJECTIVE--To compare the mean nocturnal blood pressure of patients with various forms of renal and endocrine hypertension with that in patients with primary and white coat hypertension, and normal blood pressure. DESIGN--Ambulatory monitoring of blood pressure over 24 hours in a prospective study. SETTING--Two German centres for outpatients with hypertension and kidney diseases. SUBJECTS--176 normotensive subjects, 490 patients with primary hypertension including mild and severe forms, 42 with white coat hypertension, 208 patients with renal and renovascular hypertension, 43 with hypertension and endocrine disorders, and three with coarctation of the aorta. MAIN OUTCOME MEASURES--Fall in nocturnal blood pressure. RESULTS--Blood pressure in normotensive subjects fell by a mean of 14 mm Hg (11%) systolic and 13 mm Hg (17%) diastolic overnight (2200 to 0600). The falls in patients with primary and white coat hypertension were not significantly different. In all patients with renal and renovascular hypertension, however, the fall was significantly reduced (range of fall from 3/3 mm Hg to 7/9 mm Hg). In patients with hypertension and endocrine disorders the pattern of night time blood pressure was not uniform: patients with hyperthyroidism, primary hyperaldosteronism, and Cushing's syndrome had significantly smaller reductions in blood pressure (6/8, 4/7, 3/6 mm Hg, respectively). In patients with phaeochromocytoma the mean night time blood pressure increased by 4/2 mm Hg. In patients with hypertension, primary hyperparathyroidism, and unoperated coarctation of the aorta the falls in blood pressure were normal. CONCLUSIONS--In normotensive subjects and those with primary hypertension there is usually a reduction in blood pressure at night. In all renal forms of secondary hypertension and in most endocrine forms the reduction in blood pressure is only a third to a half of normal. Patients with primary hyperparathyroidism and unoperated coarctation of the aorta show a normal reduction.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Howell W. H. A CONTRIBUTION TO THE PHYSIOLOGY OF SLEEP, BASED UPON PLETHYSMOGRAPHIC EXPERIMENTS. J Exp Med. 1897 May 1;2(3):313–345. doi: 10.1084/jem.2.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai Y., Abe K., Sasaki S., Minami N., Nihei M., Munakata M., Murakami O., Matsue K., Sekino H., Miura Y. Altered circadian blood pressure rhythm in patients with Cushing's syndrome. Hypertension. 1988 Jul;12(1):11–19. doi: 10.1161/01.hyp.12.1.11. [DOI] [PubMed] [Google Scholar]
- Kem D. C., Weinberger M. H., Gomez-Sanchez C., Kramer N. J., Lerman R., Furuyama S., Nugent C. A. Circadian rhythm of plasma aldosterone concentration in patients with primary aldosteronism. J Clin Invest. 1973 Sep;52(9):2272–2277. doi: 10.1172/JCI107414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Middeke M., Klüglich M., Holzgreve H. Circadian blood pressure rhythm in primary and secondary hypertension. Chronobiol Int. 1991;8(6):451–459. doi: 10.3109/07420529109059181. [DOI] [PubMed] [Google Scholar]
- Middeke M., Mika E., Schreiber M. A., Beck B., Wächter B., Holzgreve H. Ambulante indirekte Blutdrucklangzeitmessung bei primärer und sekundärer Hypertonie. Klin Wochenschr. 1989 Jul 17;67(14):713–716. doi: 10.1007/BF01721289. [DOI] [PubMed] [Google Scholar]
- O'Brien E., Sheridan J., O'Malley K. Dippers and non-dippers. Lancet. 1988 Aug 13;2(8607):397–397. doi: 10.1016/s0140-6736(88)92867-x. [DOI] [PubMed] [Google Scholar]
- Schrader I., Person C., Pfertner U., Buhr-Schinner H., Schoel G., Warneke G., Haupt A., Scheler F. Fehlender nächtlicher Blutdruckabfall in der 24-Stunden Blutdruckmessung: Hinweis auf eine sekundäre Hypertonie. Klin Wochenschr. 1989 Jul 3;67(13):659–665. doi: 10.1007/BF01718026. [DOI] [PubMed] [Google Scholar]



