Abstract
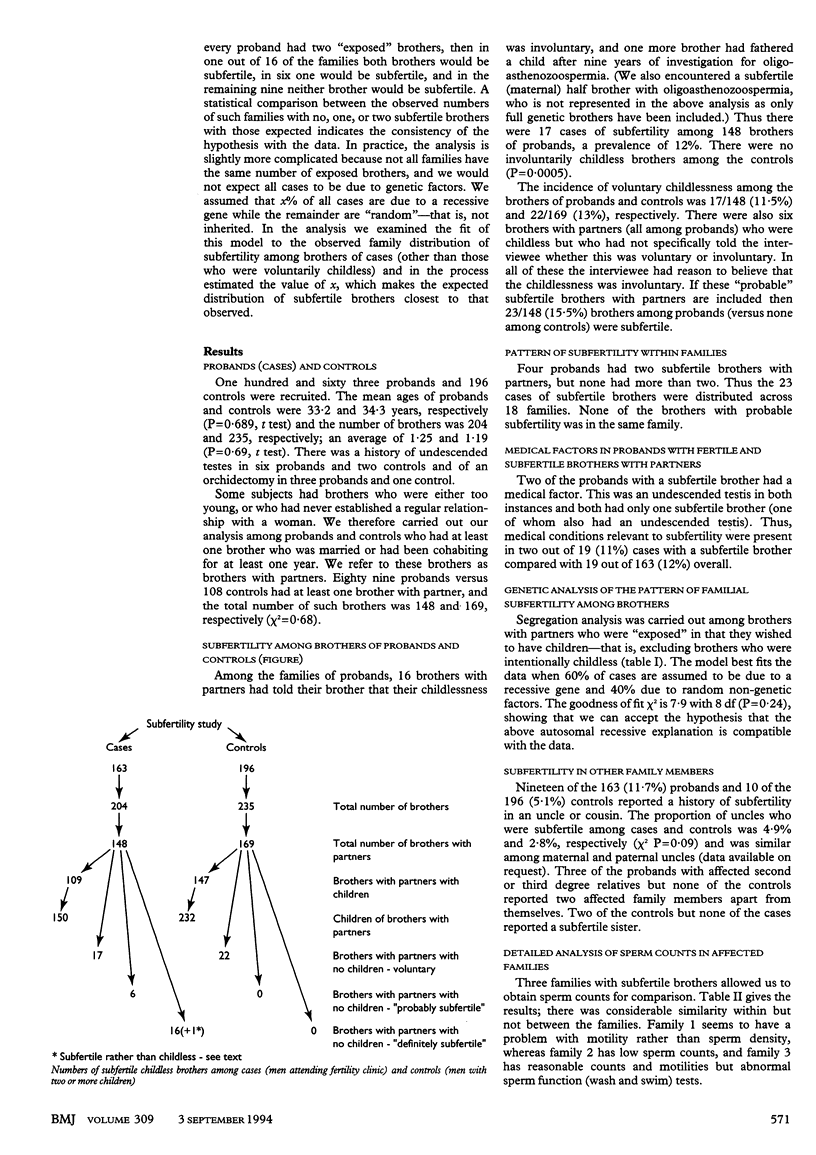
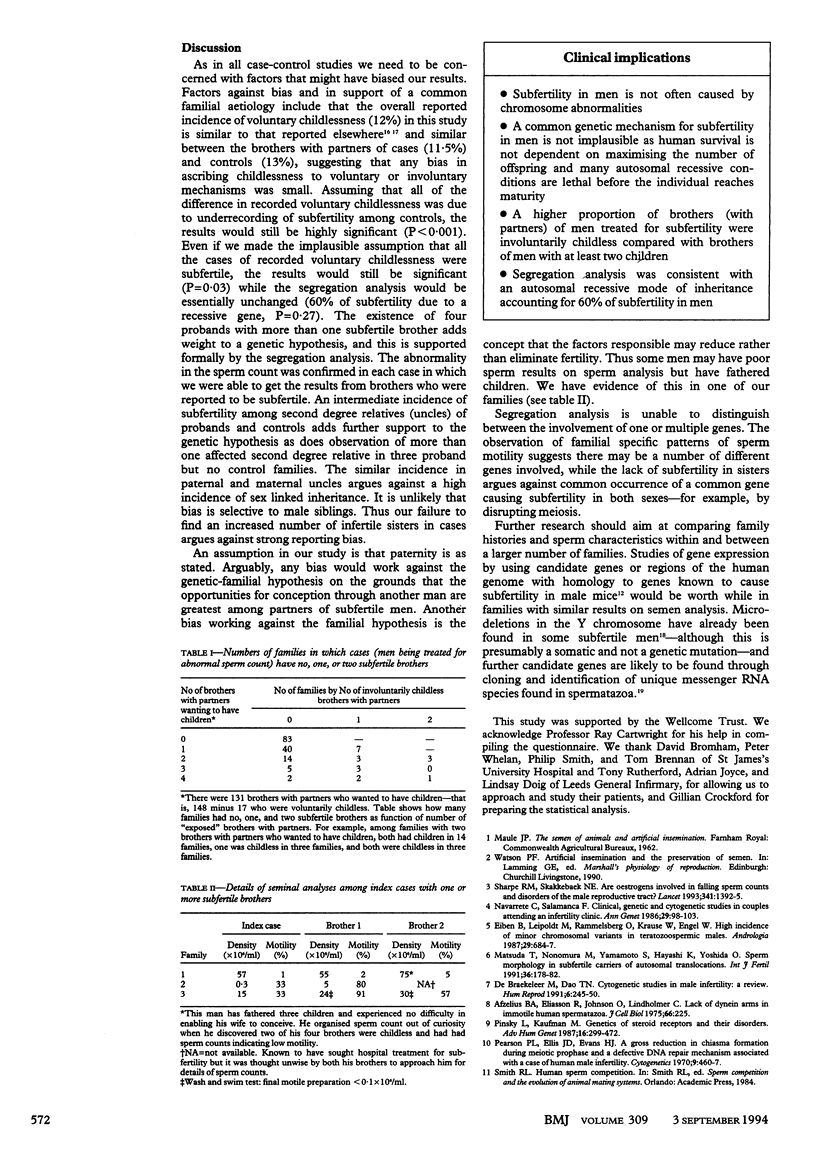
OBJECTIVE--To test the hypothesis that subfertility in men is familial and to examine the distribution of subfertility within families for consistency with a genetic cause. DESIGN--Case-control study and segregation analysis. SETTING--Two teaching hospitals in Leeds. SUBJECTS--Cases (probands) were men with an abnormal sperm count who attended a subfertility clinic and whose partners had no major factor contravening fertility. Controls were fathers of two or more children recruited through vasectomy clinics or a maternity department. MAIN OUTCOME MEASURES--The incidence of involuntary childlessness among brothers with partners and among sisters and second and third degree male relatives. When possible clinical and laboratory details were obtained from involuntarily childless brothers. RESULTS--Seventeen of the 148 (11.5%) brothers of probands but none of the 169 brothers of controls had sought medical advice for childlessness (P < 0.0005). Four probands had more than one involuntarily childless brother. There were six further brothers whose childlessness was thought to be involuntary bringing the total prevalence of subfertility among brothers of probands to 16%. Segregation analysis was consistent with an autosomal recessive mode of inheritance accounting for 60% of subfertility in men. Seventeen of the 346 (4.9%) uncles of probands and 10 of 420 (2.8%) uncles of controls were reported to be involuntarily childless (P = 0.09), but there was no difference in childlessness among sisters. In three families sperm counts from "affected" brothers confirmed the diagnosis and showed considerable similarities within but not between families. CONCLUSION--Subfertility in men has a familial component, and the observations are consistent with an autosomal recessive mode of inheritance in over half the cases. Several different genes are probably involved.
Full text
PDF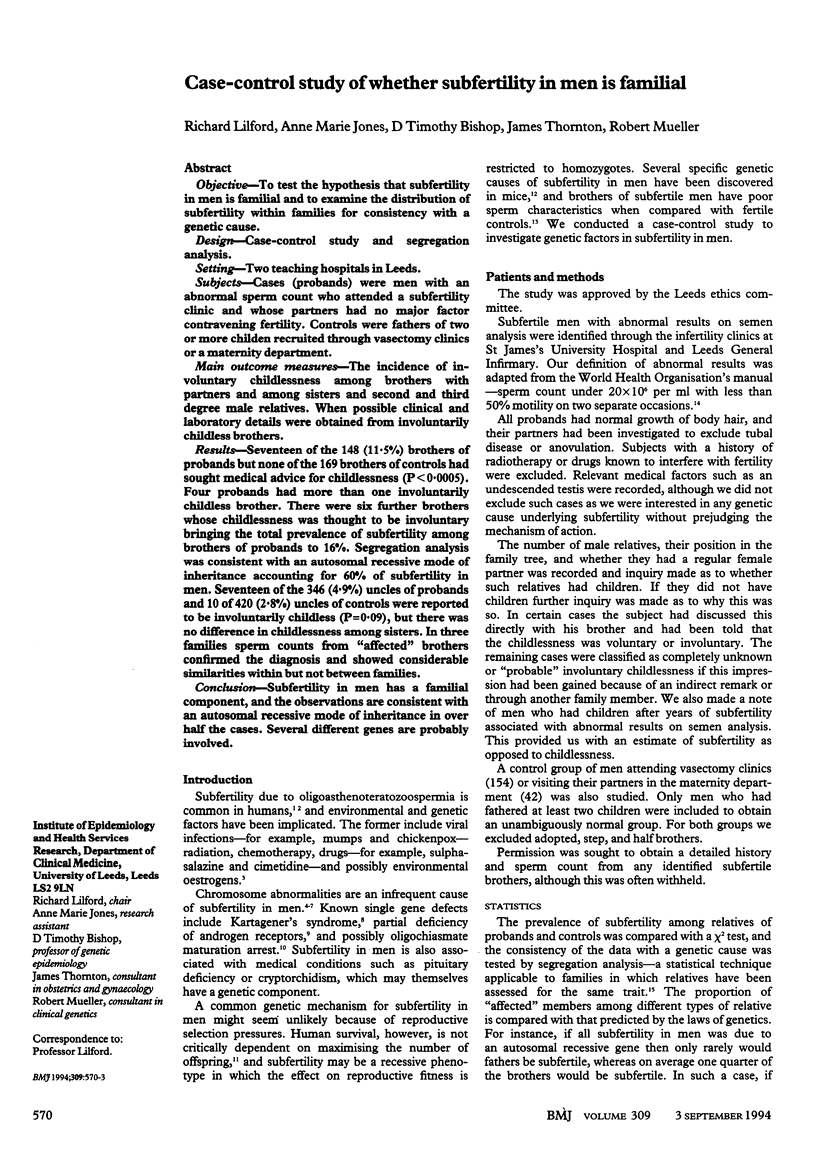

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Afzelius B. A., Eliasson R., Johnsen O., Lindholmer C. Lack of dynein arms in immotile human spermatozoa. J Cell Biol. 1975 Aug;66(2):225–232. doi: 10.1083/jcb.66.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chubb C. Genetically defined mouse models of male infertility. J Androl. 1989 Mar-Apr;10(2):77–88. doi: 10.1002/j.1939-4640.1989.tb00064.x. [DOI] [PubMed] [Google Scholar]
- Czyglik F., Mayaux M. J., Guihard-Moscato M. L., David G., Schwartz D. Lower sperm characteristics in 36 brothers of infertile men, compared with 545 controls. Fertil Steril. 1986 Feb;45(2):255–258. doi: 10.1016/s0015-0282(16)49164-8. [DOI] [PubMed] [Google Scholar]
- De Braekeleer M., Dao T. N. Cytogenetic studies in male infertility: a review. Hum Reprod. 1991 Feb;6(2):245–250. [PubMed] [Google Scholar]
- Eiben B., Leipoldt M., Rammelsberg O., Krause W., Engel W. High incidence of minor chromosomal variants in teratozoospermic males. Andrologia. 1987 Nov-Dec;19(6):684–687. doi: 10.1111/j.1439-0272.1987.tb01929.x. [DOI] [PubMed] [Google Scholar]
- Johnson G., Roberts D., Brown R., Cox E., Evershed Z., Goutam P., Hassan P., Robinson R., Sahdev A., Swan K. Infertile or childless by choice? A multipractice survey of women aged 35 and 50. Br Med J (Clin Res Ed) 1987 Mar 28;294(6575):804–806. doi: 10.1136/bmj.294.6575.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuda T., Nonomura M., Yamamoto S., Hayashi K., Yoshida O. Sperm morphology in subfertile carriers of autosomal translocations. Int J Fertil. 1991 May-Jun;36(3):178–182. [PubMed] [Google Scholar]
- Miller D., Tang P. Z., Skinner C., Lilford R. Differential RNA fingerprinting as a tool in the analysis of spermatozoal gene expression. Hum Reprod. 1994 May;9(5):864–869. doi: 10.1093/oxfordjournals.humrep.a138607. [DOI] [PubMed] [Google Scholar]
- Navarrete C., Salamanca F. Clinical, genetic and cytogenetic studies in couples attending an infertility clinic. Ann Genet. 1986;29(2):98–103. [PubMed] [Google Scholar]
- Pearson P. L., Ellis J. D., Evans H. J. A gross reduction in chiasma formation during meiotic prophase and a defective DNA repair mechanism associated with a case of human male infertility. Cytogenetics. 1970;9(6):460–467. doi: 10.1159/000130115. [DOI] [PubMed] [Google Scholar]
- Pinsky L., Kaufman M. Genetics of steroid receptors and their disorders. Adv Hum Genet. 1987;16:299–472. doi: 10.1007/978-1-4757-0620-8_5. [DOI] [PubMed] [Google Scholar]
- Sharpe R. M., Skakkebaek N. E. Are oestrogens involved in falling sperm counts and disorders of the male reproductive tract? Lancet. 1993 May 29;341(8857):1392–1395. doi: 10.1016/0140-6736(93)90953-e. [DOI] [PubMed] [Google Scholar]
- Templeton A., Fraser C., Thompson B. The epidemiology of infertility in Aberdeen. BMJ. 1990 Jul 21;301(6744):148–152. doi: 10.1136/bmj.301.6744.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt P., Chandley A. C., Hargreave T. B., Keil R., Ma K., Sharkey A. Microdeletions in interval 6 of the Y chromosome of males with idiopathic sterility point to disruption of AZF, a human spermatogenesis gene. Hum Genet. 1992 Jul;89(5):491–496. doi: 10.1007/BF00219172. [DOI] [PubMed] [Google Scholar]


