Abstract
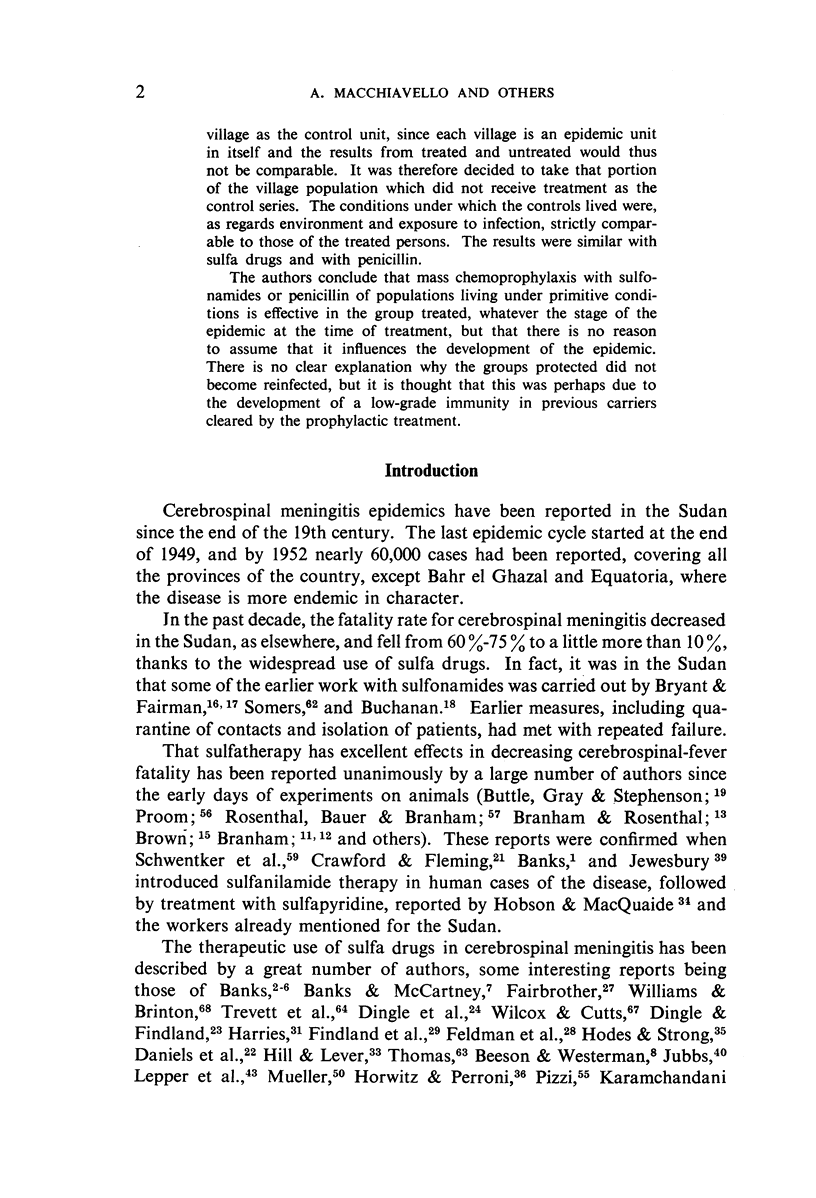
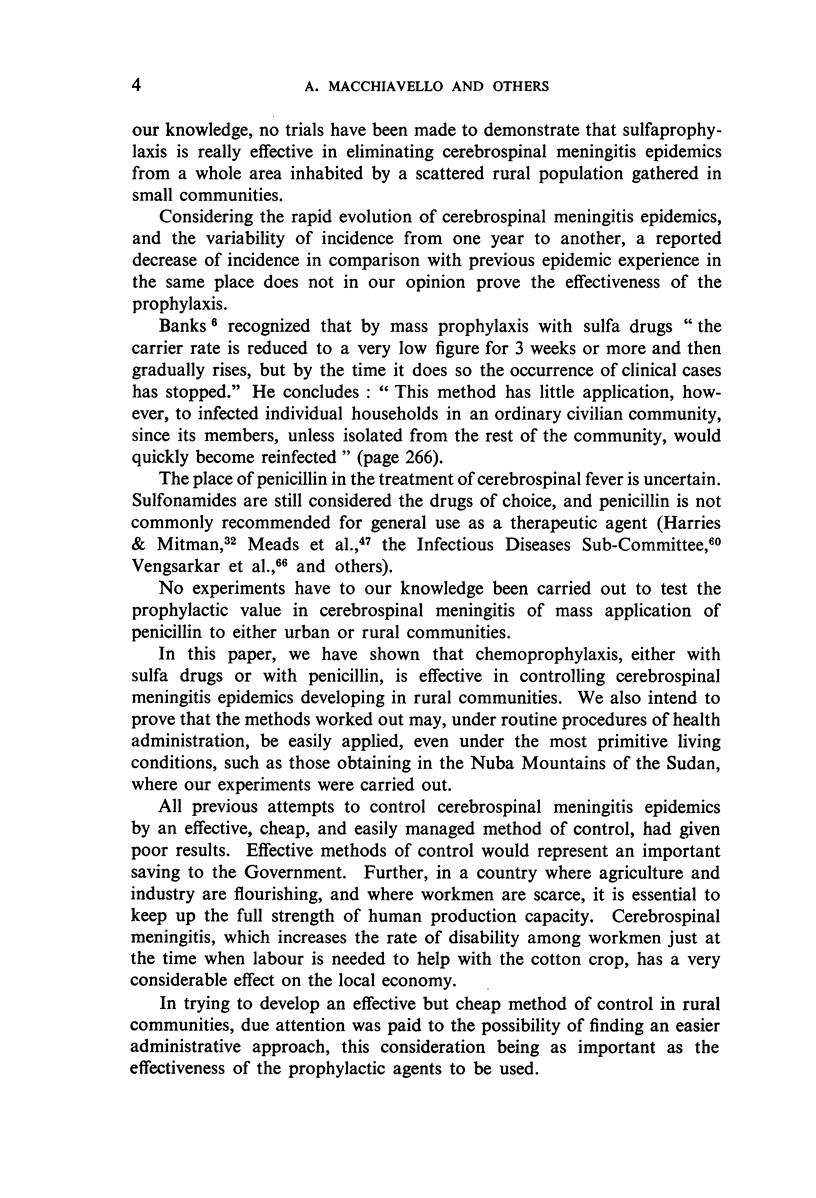
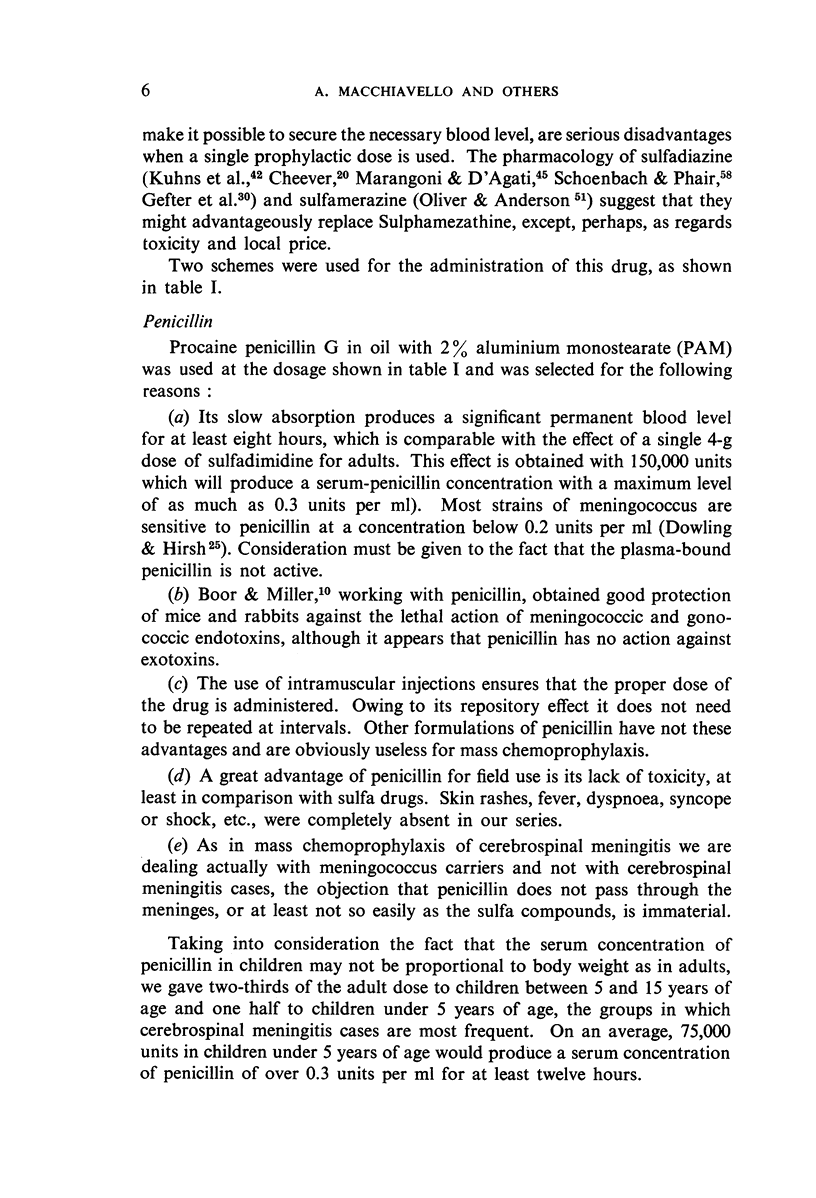
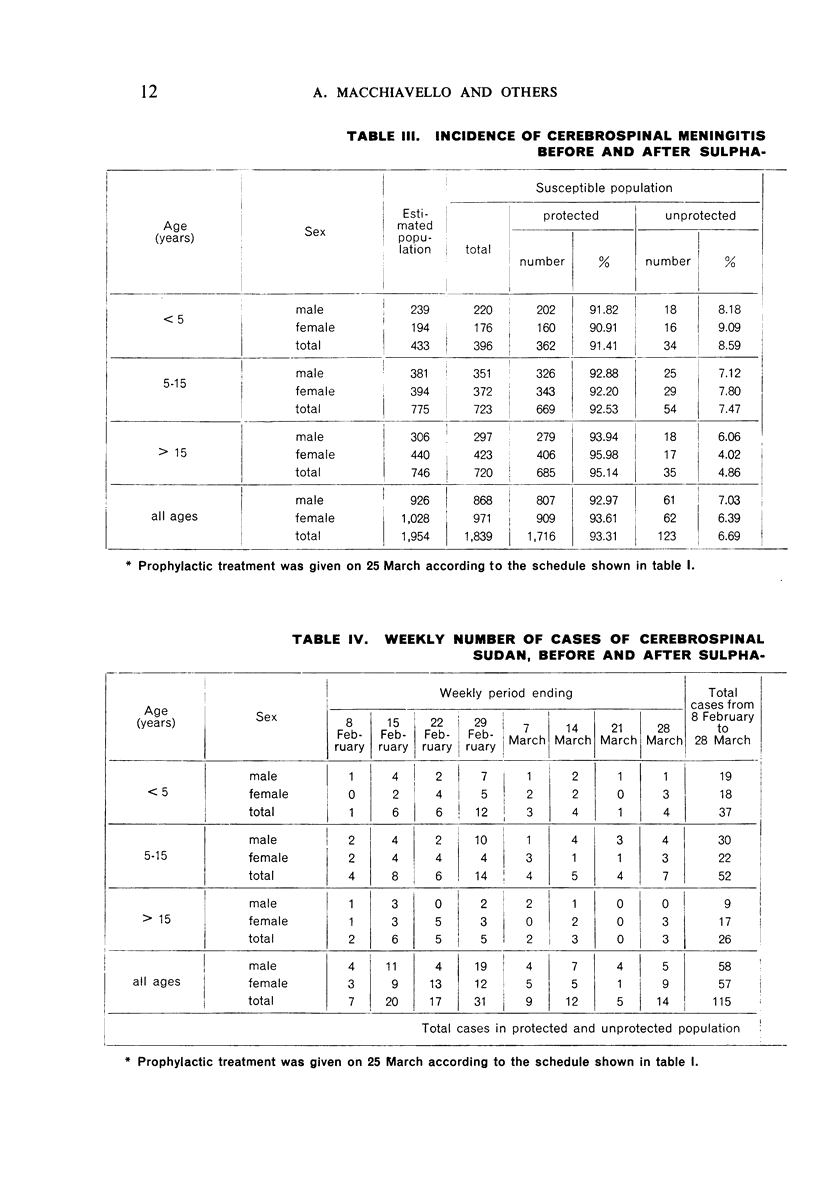
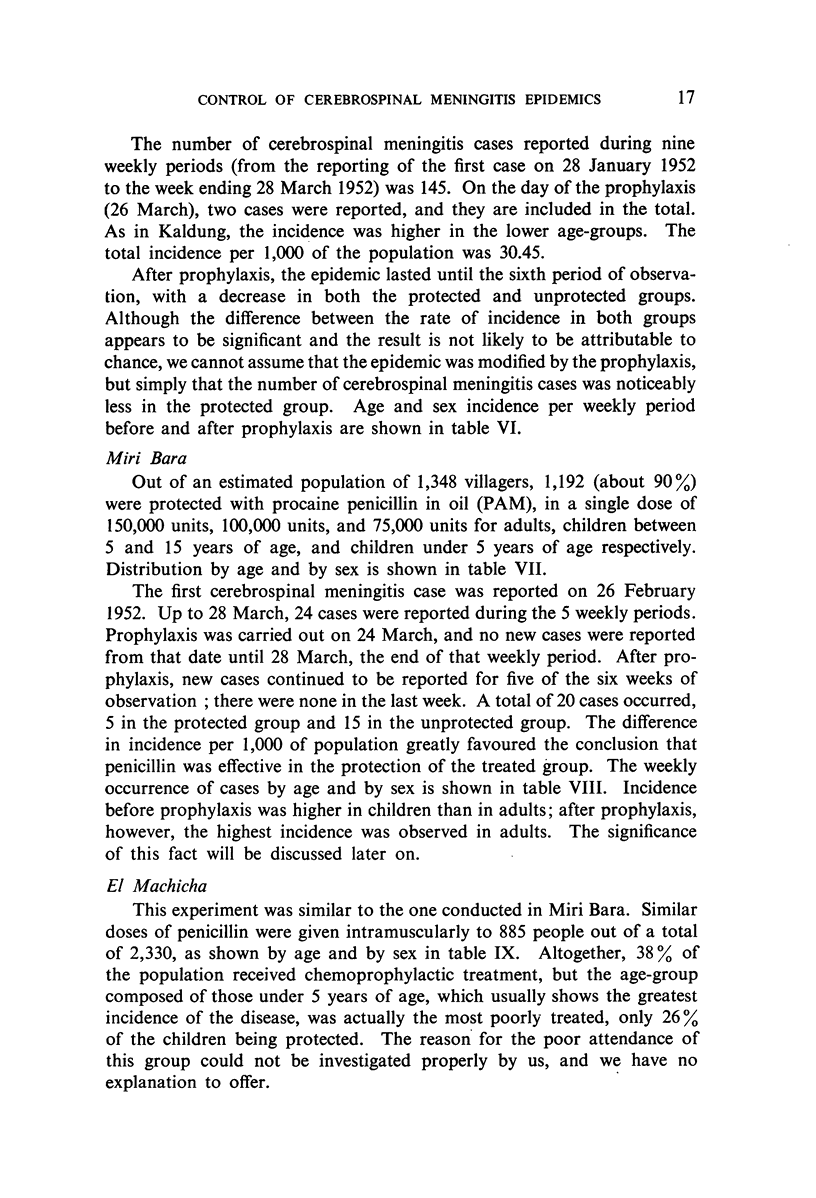
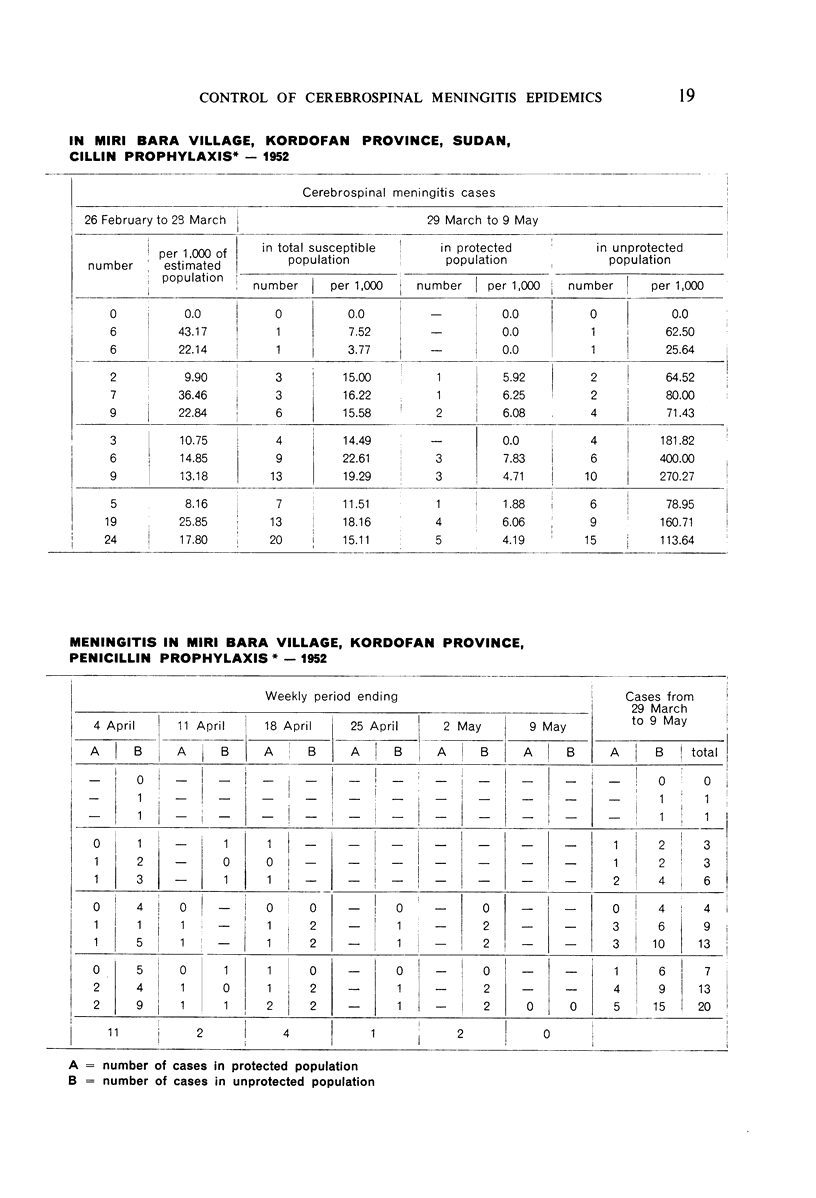
Four villages in Kordofan Province of the Sudan were selected by the authors to determine the effectiveness of mass prophylactic treatment with sulfa drugs and penicillin in controlling cerebrospinal meningitis epidemics in rural areas with highly primitive living conditions. Sulfadimidine was given orally in two of the villages, and procaine penicillin G in oil with 2% aluminium monostearate (PAM) was given intramuscularly in the other two. The population of the villages was classified by age and by sex and given the following prophylactic doses: in Kaldung village, where 93% of the population was treated, 4 g of sulfadimidine were given to persons over 15 years of age, 2.5 g to those between 15 and 5, and 1.5 g to those under 5; in Korongo Abdulla, the same age-groups received 2.0 g, 1.0 g, and 0.5 g, respectively, and 34% of the population was treated; in El Machicha and Miri Bara villages, PAM was given to 38% and 90% of the respective populations in the dosage of 150,000 units to those over 15 years of age, 100,000 units to those between 15 and 5, and 75,000 to those under 5.
In this campaign, some 4,000 people were examined daily and, where necessary, treated by a medical staff of four with five trained assistant dressers. The drugs had a noticeable influence on the number of cases in the protected groups, which showed an incidence of 4.86 cases per 1,000 of the total population of the 4 villages against 17.68 cases per 1,000 in the unprotected groups. The authors point out that in the Sudan it is not possible to take a neighbouring village as the control unit, since each village is an epidemic unit in itself and the results from treated and untreated would thus not be comparable. It was therefore decided to take that portion of the village population which did not receive treatment as the control series. The conditions under which the controls lived were, as regards environment and exposure to infection, strictly comparable to those of the treated persons. The results were similar with sulfa drugs and with penicillin.
The authors conclude that mass chemoprophylaxis with sulfonamides or penicillin of populations living under primitive conditions is effective in the group treated, whatever the stage of the epidemic at the time of treatment, but that there is no reason to assume that it influences the development of the epidemic. There is no clear explanation why the groups protected did not become reinfected, but it is thought that this was perhaps due to the development of a low-grade immunity in previous carriers cleared by the prophylactic treatment.
Full text
PDF

























Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BONETTI DUPONT C. A., LOZA COLOMER J. C. Nuestra experiencia en el tratamiento de la meningitis cerebroespinal epidémica. Sem Med. 1949 Jun 23;56(25):885–899. [PubMed] [Google Scholar]
- Beeson P. B., Westerman E. Cerebrospinal Fever and Sulphonamides. Br Med J. 1943 Apr 24;1(4294):497–500. doi: 10.1136/bmj.1.4294.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boor A. K., Miller C. P. THE EFFECT OF PENICILLIN ON THE LETHAL ACTION OF MENINGOCOCCAL ENDOTOXIN IN EXPERIMENTAL ANIMALS. Science. 1945 Oct 26;102(2652):427–428. doi: 10.1126/science.102.2652.427. [DOI] [PubMed] [Google Scholar]
- Branham S. E. THE MENINGOCOCCUS (NEISSERIA INTRACELLULARIS). Bacteriol Rev. 1940 Jun;4(2):59–96. doi: 10.1128/br.4.2.59-96.1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DOWLING H. F., SWEET L. K. Specific therapy of bacterial infections of central nervous system. J Am Med Assoc. 1949 Mar 19;139(12):755–758. doi: 10.1001/jama.1949.02900290001001. [DOI] [PubMed] [Google Scholar]
- Discussion on the Treatment of Acute Meningitis. Proc R Soc Med. 1945 Aug;38(10):605–612. doi: 10.1177/003591574503801020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbrother R. W. Cerebrospinal Meningitis. The Use of Sulphonamide Derivatives in Prophylaxis. Br Med J. 1940 Dec 21;2(4172):859–862. doi: 10.1136/bmj.2.4172.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harries G. E. Cerebrospinal Fever treated by Chemotherapy. Br Med J. 1942 Oct 10;2(4266):423–425. doi: 10.1136/bmj.2.4266.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jubb A. A. Chemotherapy and Serotherapy in Cerebrospinal Meningitis. Br Med J. 1943 Apr 24;1(4294):501–504. doi: 10.1136/bmj.1.4294.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MATTHEWS J. D. Sequelae of meningococcal meningitis in children. Lancet. 1949 Jul 23;2(6569):149–149. doi: 10.1016/s0140-6736(49)90995-2. [DOI] [PubMed] [Google Scholar]
- Phair J. J., Schoenbach E. B., Root C. M. Meningococcal Carrier Studies. Am J Public Health Nations Health. 1944 Feb;34(2):148–154. doi: 10.2105/ajph.34.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzi M. A Severe Epidemic of Meningococcus Meningitis in Chile, 1941-1942. Am J Public Health Nations Health. 1944 Mar;34(3):231–238. doi: 10.2105/ajph.34.3.231. [DOI] [PMC free article] [PubMed] [Google Scholar]


