Abstract
A 5′ nuclease PCR assay for detection of the Yersinia pestis plasminogen activator (pla) gene in human respiratory specimens with simulated Y. pestis infection was developed. An internal positive control was added to the reaction mixture in order to detect the presence of PCR inhibitors that are often found in biological samples. The assay was 100% specific for Y. pestis. In the absence of inhibitors, a sensitivity of 102 CFU/ml of respiratory fluid was obtained. When inhibitors were present, detection of Y. pestis DNA required a longer sample treatment time and an initial concentration of bacteria of at least 104 CFU/ml. The test's total turnaround time was less than 5 h. The assay described here is well suited to the rapid diagnosis of pneumonic plague, the form of plague most likely to result from a bioterrorist attack.
Protecting the population against an act of bioterrorism is a major concern for many governments. Yersinia pestis, the agent of plague, can be viewed as a potential bioweapon due to its ability to cause high rates of morbidity and mortality in humans. The intentional dissemination of plague by terrorists would most likely occur by aerosolization, causing fulminant pneumonia in exposed individuals. Since pneumonic plague is almost always fatal when untreated, clinical microbiology laboratories play a pivotal role in the early detection of this type of infectious agent, thus allowing rapid implementation of effective preventive measures. Availability of a rapid diagnostic procedure using molecular techniques (such as real-time PCR) is essential in the establishment of coordinated laboratory response systems. Several PCR assays have been developed (1, 3-7, 10, 13): the plasmidic plasminogen activator (pla) gene (located on the Y. pestis-specific pPst/pCP1 plasmid [5, 11]) was found to be the most sensitive target, since its copy number can be as high as 186 per bacterium (8). In the present study, we describe a real-time PCR protocol for detection of the Y. pestis pla gene. The assay is based on 5′ exonuclease assay technology coupled with automated DNA extraction and uses a minor groove binder-conjugated small DNA probe for DNA detection via hybridization-triggered fluorescence: subsequent multiplex development can be thus envisaged. Inclusion of an internal positive control (IPC) in each batch assay enabled the detection of endogenous PCR inhibitors.
The primers and the fluorogenic probe for the pla gene (GenBank accession no. M27820) were designed with Primer Express software, version 2.0 (Applied Biosystems, Foster City, Calif.) and were obtained from Applied Biosystems (Warrington, United Kingdom). The nucleotide sequences of the forward and reverse primers were 5′-GAAAGGAGTGCGGGTAATAGGTT-3′ (positions 816 to 838) and 5′-AACCAGCGCTTTTCTA-3′ (positions 869 to 884), respectively. The sequence of the minor groove binder probe was 6-carboxyfluorescein-5′-GACTTGCAGGCC-3′ (positions 840 to 851). PCR amplifications were performed in 25-μl reaction volumes including 1× TaqMan Universal Master Mix (Applied Biosystems) containing dUTP and uracil-N-glycosylase, each primer at a final concentration of 50 nM, the fluorescently labeled probe at a final concentration of 200 nM, and 5 μl of DNA extracted with a MagNA Pure LC DNA isolation kit III (Roche Molecular Biochemicals, Mannheim, Germany) as recommended by the manufacturer (Roche). DNA extracts were automatically distributed by using the MagNA Pure system, thus limiting the risk of contamination by exogenous DNA. The exogenous IPC (PE Applied Biosystems, Foster City, Calif.), consisting of a nonbiological synthetic template DNA and a set of primers and probe targeted to it, was included in every reaction. We constructed the plasmid pYpla (a pUC19 derivative containing a 335-bp PCR product of the pla gene) and used it as a standard for assay calibration. All reactions were performed in duplicate with an ABI Prism SDS 7000 system (Applied Biosystems). Standard amplification parameters were as follows: 50°C for 2 min and 95°C for 10 min, followed by 40 cycles of 95°C for 15 s and 60°C for 1 min. Real-time data were analyzed with SDS software, version 1.0. The cycle threshold (Ct) value was defined as the cycle during which the reporting dye fluorescence first exceeded the threshold. A low Ct value thus corresponded to a high target concentration.
In a first step, we evaluated the real-time PCR assay with 51 reference strains of pathogenic and nonpathogenic Yersinia species (Y. pestis, 18 strains; Y. pseudotuberculosis, 18; Y. enterocolitica, 8; Y. aldovae, 1; Y. bercovieri, 1; Y. frederiksenii, 1; Y. intermedia, 1; Y. kristensenii, 1; Y. mollaretii, 1; and Y. rohdei, 1) from the French National Yersinia Reference Center (Centre National de Référence des Yersinia, Institut Pasteur, Paris, France) and 26 strains of other bacterial species (Acinetobacter baumannii, 1 strain; Alcaligenes sp., 1; Bacillus anthracis, 1; Citrobacter freundii, 1; Enterobacter aerogenes, 1; Enterobacter cloacae, 1; Enterococcus faecalis, 1; Escherichia coli, 1; Haemophilus influenzae, 1; Haemophilus parainfluenzae, 1; Klebsiella oxytoca, 1; Klebsiella pneumoniae, 2; Proteus mirabilis, 2; Proteus vulgaris, 2; Pseudomonas aeruginosa, 1; Salmonella enterica serovar Typhimurium, 1; Serratia marcescens, 1; Shigella flexneri, 1; Staphylococcus aureus, 1; Staphylococcus epidermidis, 1; Stenotrophomonas maltophilia, 1; Streptococcus agalactiae, 1; group G Streptococcus, 1) from the stock collection of the Bacteriology Laboratory at the Lille University Medical Center (Lille, France). Strains were grown on Columbia agar with 5% defibrinated sheep's blood (bioMérieux, Marcy l'Etoile, France) at 37°C for 18 h. Level 3 and level 2 biosafety rules were followed for work with class 3 and class 2 pathogens, respectively. The assay was found to be (i) Y. pestis specific, since amplicons were generated only with Y. pestis DNA, (ii) reproducible, giving similar Ct values for two separate measurements, and (iii) highly sensitive, allowing detection of as few as 1.5 bacteria per ml. A correlation between the magnitude of the bacterial inoculum (titrated by using conventional cultures) and the Ct value was determined: for bacterial inocula of 150, 15, and 1.5 CFU/ml, Cts were 32 ± 0.044 (standard deviation), 36.5 ± 1.476, and 39.63 ± 1.141, respectively.
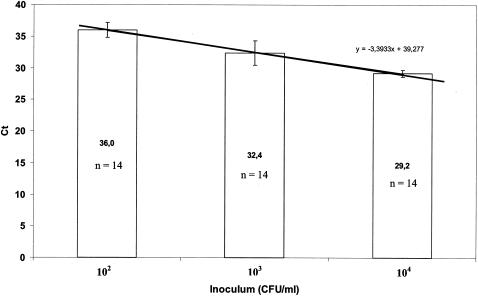
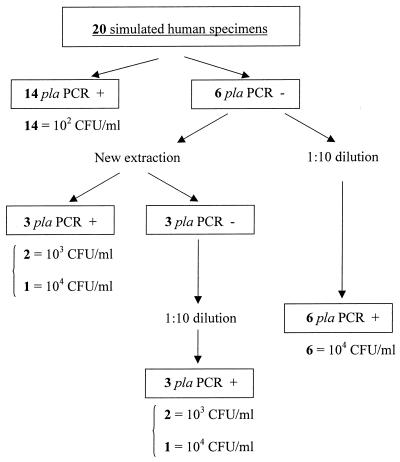
We next performed a study designed to simulate pulmonary infection by inoculating bronchial secretions with live Y. pestis cells. Sputum specimens were collected from 20 patients hospitalized at the Lille University Medical Center and frozen at −80°C until further analysis. When cultured on Columbia chocolate blood agar and prior to the addition of Y. pestis, 10 specimens were found to be sterile, whereas the remaining 10 contained one or more bacterial species (A. baumannii, E. aerogenes, E. coli, P. vulgaris, P. aeruginosa, S. marcescens, and S. aureus). Aliquots of all sputum specimens were inoculated with a calibrated suspension of Y. pestis 6/69 pYV−, ranging between 1 and 104 CFU/ml of biological fluid. Prior to DNA extraction, 100 μl of sputum was treated with dithiothreitol (Sigma-Aldrich, St. Louis, Mo.) to a final concentration of 0.15%: the mixture was then incubated for at least 30 min at 37°C until complete liquefaction was achieved. Next, 130 μl of lysis buffer and 20 μl of proteinase K were added. Samples were incubated at 65°C for 10 min and boiled for 15 min prior to automated DNA extraction and purification. Aliquots of each clinical specimen taken prior to inoculation with Y. pestis were processed simultaneously: unsurprisingly, real-time PCR gave negative results for these 20 samples. Of the deliberately Y. pestis-loaded sputum specimens, 14 were identified as positive by real-time PCR, with Ct values varying linearly (y = 3.3933x + 39.277) with the size of the bacterial inoculum. The Ct values were 36.0 ± 1.163, 32.4 ± 1.93, and 29.2 ± 0.553 for bacterial inocula of 102, 103, and 104 Y. pestis CFU per ml of biological fluid, respectively (Fig. 1). Addition of the exogenous IPC to the reaction mixture did not impair the assay's sensitivity, as similar Ct values were obtained in both the presence and absence of the IPC. Direct microscopic examination of the respiratory specimens and culture were systematically performed prior to the addition of Y. pestis to the specimen: no relationship was found between the presence of inhibitors and the cellularity of the specimens or the resulting cultures (data not shown). The six specimens that failed to yield amplicons were assumed to contain endogenous inhibitors, as indicated by the fact that the exogenous IPC had not given a signal either. They were further tested by two methods. First, a modified DNA extraction protocol involving an extended lysis step (incubation at 56°C overnight with proteinase K) was set up, and when successful amplification was still lacking, a 10-fold dilution of the DNA extract was performed (Fig. 2). The specimens classed as negative with the standard protocol were positive when this modified protocol was employed. The second method merely involved a 10-fold dilution of the DNA extract. This protocol did give positive results, but the sensitivity was always lower (104 CFU/ml, compared to 103 CFU/ml for the full proteinase K method). In conclusion, under our experimental conditions, as little as 102 Y. pestis per ml of sputum could be detected in the absence of endogenous PCR inhibitors.
FIG. 1.
Mean Ct values plotted against inoculum concentrations.
FIG. 2.
Algorithm of the process used for the 20 simulated human specimens.
The PCR assay described in this work is the first to be applied to human-derived specimens, whereas other studies have reported PCR results from in vitro assays or experimental animal infections (2, 3). The detection of Y. pestis was limited only by the presence of PCR inhibitors in the biological fluids. Hence, when inhibition was observed, we modified the extraction method, which unfortunately increased the overall diagnosis time. The IPC added to the reaction mixture detected the presence of inhibitors and was able to distinguish the true-negative results from uninterpretable results for inhibitor-containing samples.
In terms of the Y. pestis strains used in cultured and human samples, the sensitivity found here was better than that observed by Trebesius et al. (12) with a hybridization step. Our pla PCR assay also appeared to exhibit better sensitivity than that described by Hinnebusch and Schwan (4). We were able to detect as few as 1.5 CFU/ml, as did Iqbal et al. (5), who detected as few as three Y. pestis gene targets. Higgins et al. (3) reported that a Ct value of 25 corresponded to the cutoff for positivity. Our results, together with those published by Iqbal et al. (5), do not agree with this threshold, because we detected true-positive specimens with a Ct value of 36. Pollitzer (9) has pointed out that in pneumonic plague, conventional culturing detects few or no bacteria in sputum samples obtained 24 h prior to the onset of coughing and pneumonia, whereas the sputum is rich in bacteria during the pneumonic period.
In contrast to the conventional technique (which gives results only after 48 h and can monitor the kinetics of bacterial infection only during the actual course of the plague), the advantages of the technique described here (high sensitivity, a detection limit as low as 1.5 bacteria/ml, specificity, and a relatively rapid turnaround time of less than 5 h) enable its use by French reference laboratories for detecting Y. pestis in sputum in the event of a bioterrorist attack. Nevertheless, our experience showed that several guidelines are essential when real-time PCR is used as a diagnostic tool. Each batch must include a calibration range, and each specimen must be tested in duplicate with an IPC. In the event of a Ct value of >36 and/or a discrepancy between two assays, it is necessary to check the original specimen by using an extended lysis DNA extraction. When IPC amplification is not observed, the specimen must be tested again after the DNA extract is diluted 10-fold. Due to its use of a nonfluorescent quencher, this technique can potentially be combined with a fluorescent probe to enable multiplex detection of other biological warfare agents.
Acknowledgments
We thank Elisabeth Carniel and Michel Simonet for helpful discussions and comments on improving the manuscript.
REFERENCES
- 1.Campbell, J., J. Lowe, S. Walz, and J. Ezzell. 1993. Rapid and specific identification of Yersinia pestis by using a nested polymerase chain reaction procedure. J. Clin. Microbiol. 31:758-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Engelthaler, D. M., K. L. Gage, J. A. Montenieri, M. Chu, and L. G. Carter. 1999. PCR detection of Yersinia pestis in fleas: comparison with mouse inoculation. J. Clin. Microbiol. 37:1980-1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Higgins, J. A., J. Ezzell, B. J. Hinnebusch, M. Shipley, E. A. Henchal, and M. S. Ibrahim. 1998. 5′ nuclease PCR assay to detect Yersinia pestis. J. Clin. Microbiol. 36:2284-2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hinnebusch, B. J., and T. G. Schwan. 1993. New method for plague surveillance using polymerase chain reaction to detect Yersinia pestis in fleas. J. Clin. Microbiol. 31:1511-1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iqbal, S. S., J. P. Chambers, M. T. Goode, J. J. Valdes, and R. R. Brubaker. 2000. Detection of Yersinia pestis by pesticin fluorogenic probe-coupled PCR. Mol. Cell. Probes 14:109-114. [DOI] [PubMed] [Google Scholar]
- 6.Neubauer, H., H. Meyer, J. Prior, A. Hensel, and W. Splettstosser. 2000. A combination of different polymerase chain reaction (PCR) assays for the presumptive identification of Yersinia pestis. J. Vet. Med. B 47:573-580. [DOI] [PubMed] [Google Scholar]
- 7.Norkina, O. V., A. N. Kulichenko, A. L. Gintsburg, I. V. Tuchkov, Y. A. Popov, M. U. Aksenov, and I. G. Drosdov. 1994. Development of a diagnostic test for Yersinia pestis by the polymerase chain reaction. J. Appl. Bacteriol. 76:240-245. [DOI] [PubMed] [Google Scholar]
- 8.Parkhill, J., B. W. Wren, N. R. Thomson, R. W. Titball, M. T. G. Holden, M. B. Prentice, M. Sebaihia, K. D. James, C. Churcher, K. L. Mungall, S. Baker, D. Basham, S. D. Bentley, K. Brooks, A. M. Cerdeño-Tárraga, T. Chillingworth, A. Cronin, R. M. Davies, P. Davis, G. Dougan, T. Feltwell, N. Hamlin, S. Holroyd, K. Jagels, A. V. Karlyshev, S. Leather, S. Moule, P. C. F. Oyston, M. Quail, K. Rutherford, M. Simmonds, J. Skelton, K. Stevens, S. Whitehead, and B. G. Barrell. 2001. Genome sequence of Yersinia pestis, the causative agent of plague. Nature 413:523-527. [DOI] [PubMed] [Google Scholar]
- 9.Pollitzer, R. 1954. Methods of laboratory diagnosis. W. H. O. Monogr. Ser. 22:229-230.
- 10.Radnedge, L., S. Gamez-Chin, P. M. McCready, P. L. Worsham, and G. L. Andersen. 2001. Identification of nucleotide sequences for the specific and rapid detection of Yersinia pestis. Appl. Environ. Microbiol. 67:3759-3762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sodeinde, O. A., and J. D. Goguen. 1988. Genetic analysis of the 9.5-kilobase virulence plasmid of Yersinia pestis. Infect. Immun. 56:2743-2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trebesius, K., D. Harmsen, A. Rakin, J. Schmelz, and J. Heesemann. 1998. Development of rRNA-targeted PCR and in situ hybridization with fluorescently labeled oligonucleotides for detection of Yersinia species. J. Clin. Microbiol. 36:2557-2564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsukano, H., K. Itoh, S. Suzuki, and H. Watanabe. 1996. Detection and identification of Yersinia pestis by polymerase chain reaction (PCR) using multiplex primers. Microbiol. Immunol. 40:773-775. [DOI] [PubMed] [Google Scholar]