Abstract
We report a case of staphylococcal exanthematous disease in a newborn due to a toxic shock syndrome toxin 1- and SEC-producing methicillin-resistant Staphylococcus aureus strain and alert neonatologists to the probable emergence in France of the neonatal toxic shock syndrome-like exanthematous disease in newborns previously described in Japan. We advise neonatologists to pay careful attention to clinical parameters and to prescribe appropriate tests: platelet count, serum C-reactive protein concentration, and Vβ2-positive T-cell counts.
CASE REPORT
In November 2002, the pediatrics unit of a general hospital in the Centre region of France alerted the Relais Régional d'Hygiène Hospitalière du Centre (RHC) to an unusual exanthematous disease in a newborn caused by a methicillin-resistant Staphylococcus aureus (MRSA) strain.
A 2-day-old infant, born at 38 weeks of gestation (weight, 3,560 g), with no risk factors for hospital-acquired infection, presented a diffuse, systemic macular erythema. Exanthema was associated with pustules, which affected mostly the neck fold, the axillae, the inguinal folds, and the periumbilical area. The pustules rapidly developed into vesicular lesions resembling primary human herpes simplex virus lesions. This infant, born at term, was not febrile (rectal temperature between 36.8 and 37.2°C). Biological investigations were conducted on the day on which exanthema occurred: the infant was not leukopenic (leukocyte count, 12,400/mm3; 47% neutrophils) and had no marked inflammatory syndrome (C-reactive protein [CRP], 6.3 mg/liter; fibrinogen, 2.76 g/liter). Thrombocytopenia did not occur at this time (platelet count, 299,000/mm3). Viral cultures were negative for herpes simplex virus (types 1 and 2). Bacterial cultures of the pustular lesions yielded mecA-positive S. aureus. The isolate produced β-lactamase; was susceptible to all non-β-lactam antibiotics tested, except kanamycin (MIC, 16 μg/ml) and tobramycin (MIC, 12 μg/ml); and showed intermediate sensitivity to fusidic acid (MIC, 6 μg/ml).
The infant was transferred to the neonatal unit of the nearest teaching hospital. Intravenous antibiotic therapy (vancomycin and gentamicin) was initiated on the second day of erythema, together with local skin disinfection. The clinical symptoms of skin lesions regressed within 2 days of starting antibiotic therapy.
A familial enquiry revealed that the mother had a finger onyxis, but she refused swabbing (nasal swab and swabbing of the finger lesion). Thus, a maternal origin for the staphylococcal infection could not be excluded. The infection control team sought potential carriers of the MRSA strain. Cultures of swabs (nasal mucosa) from all personnel in the pediatrics unit revealed that 8 of the 23 staff members carried S. aureus, but all the isolates were mecA negative. Since November 2002, no new MRSA strains have been isolated from the pediatrics unit, implying that the strain has been eliminated.
The existence of regional centers (in this case, the RHC) within the French national system for the surveillance of nosocomial infections increases the efficiency of information transfer between those involved in the prevention of hospital infections, making it possible to issue an alert very quickly. Indeed, the rapidity of this system, which was triggered following the isolation of this unusual strain, made it possible to apply a rigorous containment policy, which may have been crucial in limiting the dissemination of this strain in the healthcare institution. The RHC alerted the Institute de Veille Sanitaire immediately, as this strain was suspected to be a Panton-Valentine leukocidin (PVL)-producing MRSA strain. The isolated strain was also sent directly to the French reference center for staphylococcal toxemia.
Genomic DNA was extracted from staphylococcal cultures and used as a template for amplification with the procedure and primers described by Jarraud et al. (2). Sequences corresponding to the sea to see genes, seh, the sek to sem genes, seo, sep, eta, etb, and tst, encoding SAE to SEE, SEH, SEK to SEM, SEO, SEP, exfoliative toxin A (ETA), ETB, and toxic shock syndrome toxin 1 (TSST-1), respectively, were used as primers for PCR. Seven virulence factor genes were identified in the strains: the tst gene, which encodes TSST-1, and the sec, sed, and sel to sep genes, which encode the SEC, SED, and SEL to SEP enterotoxins, respectively. Genes encoding PVL and ETA and ETB were not detected. Digital analysis of the SmaI macrorestriction pattern (Fig. 1) confirmed that the strain did not belong to the French clonal group of PVL-producing MRSA strains.
FIG. 1.
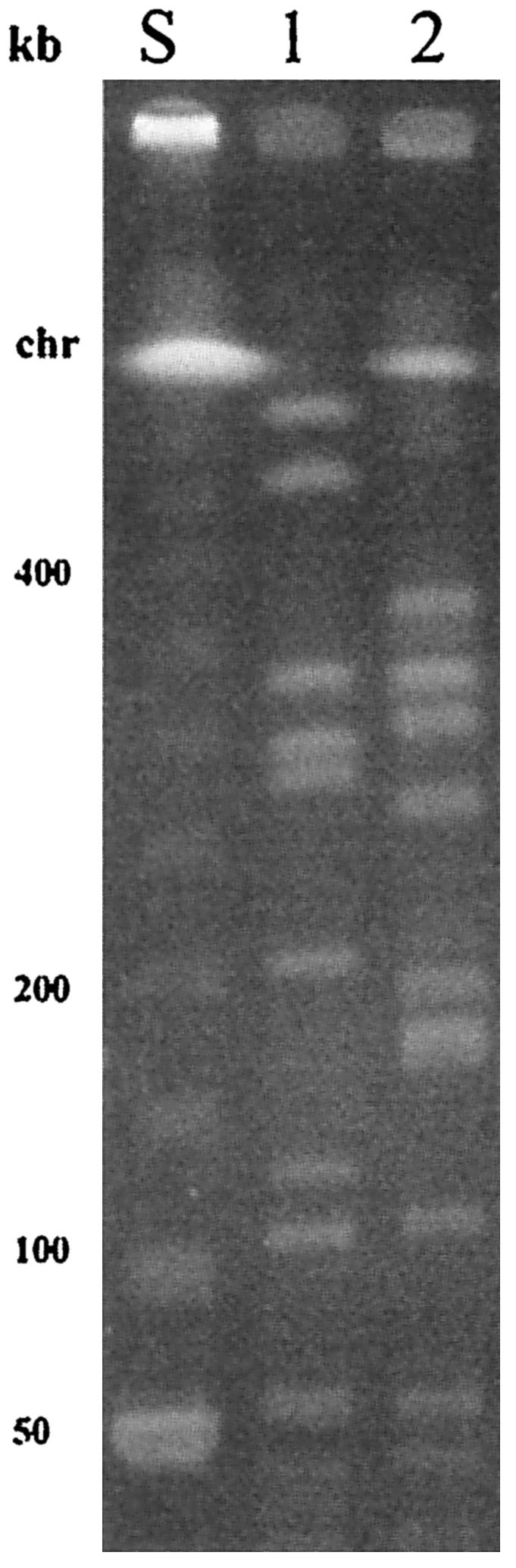
SmaI macrorestriction patterns of a TSST-1-producing MRSA strain isolated from skin lesions of a neonate (lane 1) and of the PVL-producing MRSA strain that emerged in France in 2000 (lane 2). Lane S shows size markers. chr, chromosome.
The clinical appearance of the lesions observed in this case, together with the unusual features of the MRSA strain and the production of TSST-1 and SEC toxins, raised the possibility of neonatal toxic shock syndrome-like exanthematous disease (NTED) in this infant. Takahashi et al. (4) set the following clinical criteria for NTED diagnosis: (i) exanthema and (ii) exclusion of known disease processes plus (iii) at least one of the following three signs: thrombocytopenia (low platelet count, <150,000/mm3), a low-positive serum CRP value (positive CRP, >1.0 mg/dl), and fever (rectal temperature of >38°C). In the case presented, the infant fulfilled criteria i and ii. For definitive diagnosis, rechecking platelet count and serum CRP value after 48 h of progression and investigating the change in anti-TSST-1 antibody titers between two paired serum samples and the change in Vβ2-positive T-cell counts by fluorescence-activated cell sorting analysis should have been sufficient. Indeed, expansion of the Vβ2-positive T-cell populations in the acute phase or the deletion of such T cells in the recovery phase implies that the patient has NTED (3). As this disease has not previously been reported in France or elsewhere in Europe, we did not carry out these investigations.
Discussion.
In 1998, Takahashi et al. (3) suggested that an emerging exanthematous disease affecting newborns in Japan, involving isolates that produced unusual virulence factors, TSST-1, and enterotoxins, should be named NTED (3, 4). The potentially highly virulent MRSA strains involved differ from the PVL-producing MRSA strains that emerged in France in 2000 (1) and in The Netherlands (5). TSST-1- and SEC-producing MRSA strains associated with NTED have not yet been described in Europe.
In France, nosocomial infections have been monitored at the supraregional level since 1992, by five coordinating centers (Centres de Coordination de la Lutte contre les Infections Nosocomiales [CCLINs]). A national network (Réseau d'Alerte, d'Investigation et de Surveillance des Infections Nosocomiales) brings together the CCLINs and the National Institute for Public Health Surveillance (Institut de Veille Sanitaire). Antibiotic resistance is monitored by national reference centers for the species concerned (Centres Nationaux de Référence) and the Observatoire National de l'Epidémiologie de la Résistance Bactérienne aux Antibiotiques. The RHC is the monitoring center for the Centre region and is part of the West France CCLIN. Under this system, the RHC has been monitoring multidrug-resistant bacteria in the Centre region of France since 2000. It is notified of all unusual clinical cases of infectious disease and of bacterial isolates displaying unusual antibiotic resistance phenotypes.
Neonates fulfilling the clinical criteria for NTED were observed in 26% (19 of 74) of major neonatal care units in Japan in 1995 and in 71% (63 of 89) of such units in 1998, indicating that the incidence of NTED in Japan has been increasing (3). There is apprehension that NTED will become widespread throughout the world, because MRSA has been spreading on a global level. This report aims to alert neonatologists to the probable emergence of NTED in Europe and advises them as to the necessary biological investigations to be conducted in such clinical cases.
Acknowledgments
We thank J.-C. Laborie for helpful discussions.
REFERENCES
- 1.Dufour, P., Y. Gillet, M. Bes, G. Lina, F. Vandenesch, D. Floret, J. Etienne, and H. Richet. 2002. Community-acquired methicillin-resistant Staphylococcus aureus infections in France: emergence of a single clone that produces Panton-Valentine leukocidin. Clin. Infect. Dis. 35:819-824. [DOI] [PubMed] [Google Scholar]
- 2.Jarraud, S., G. Cozon, F. Vandenesch, M. Bes, J. Etienne, and G. Lina. 1999. Involvement of enterotoxins G and I in staphylococcal toxic shock syndrome and staphylococcal scarlet fever. J. Clin. Microbiol. 37:2446-2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Takahashi, N., H. Kato, K. Imanishi, K. Miwa, S. Yamanami, H. Nishida, and T. Uchiyama. 2000. Immunopathophysiological aspects of an emerging neonatal infectious disease induced by a bacterial superantigen. J. Clin. Investig. 106:1409-1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takahashi, N., H. Nishida, H. Kato, K. Imanishi, Y. Sakata, and T. Uchiyama. 1998. Exanthematous disease induced by toxic shock syndrome toxin 1 in the early neonatal period. Lancet 351:1614-1619. [DOI] [PubMed] [Google Scholar]
- 5.Tiemersma, E., W. Wannet, E. op de Coul, A. de Neeling, and M. van de Laar. 17April2003. Introduction of surveillance of infections with Staphylococcus aureus containing the Panton-Valentine leukocidin gene in the Netherlands. Eurosurv. Wkly. 2003 7:020417. [Online.] http://www.eurosurv.org. [Google Scholar]


