Abstract
Objective
Effective treatments for major depressive disorder exist, yet some patients fail to respond, or achieve only partial response. One approach to optimizing treatment success is to identify which patients are more likely to respond best to which treatments. The objective of this investigation was to determine if patient personality characteristics are predictive of response to either cognitive-behavioural therapy (CBT) or pharmacotherapy (PHT).
Method
Depressed patients completed the Revised NEO Personality Inventory, which measures the higher-order domain and lower-order facet traits of the Five-Factor Model of Personality, and were randomized to receive either CBT or PHT.
Result
Four personality traits—the higher-order domain neuroticism and 3 lower-order facet traits: trust, straightforwardness, and tendermindedness—were able to distinguish a differential response rate to CBT, compared with PHT.
Conclusion
The assessment of patient dimensional personality traits can assist in the selection and optimization of treatment response for depressed patients.
Keywords: depression, psychotherapy, pharmacotherapy, personality, treatment selection
Clinical Implications
Personality assessment can play a role in treatment selection.
Matching patient personality with treatment type may maximize response.
Depressed patients with high neuroticism respond best to pharmacotherapy.
Limitations
Results from randomized controlled trials may not generalize to everyday practice.
Results may not extend to other forms of psychotherapy aside from CBT.
Personality results relied exclusively on self-report.
In the last 2 decades, an array of empirically validated pharmacological and psychosocial treatments for MDD were developed.1-3 Despite these advances, substantial proportions of depressed patients do not respond or demonstrate only partial response.4-6 One-third of outcome studies using known effective treatments for MDD produce negative results.7 This inconsistency of treatment outcome across studies was dubbed the unpredictability paradox, and is attributed partly to patient heterogeneity.8 Individual differences in the clinical profiles of depressed patients across investigations, including personality characteristics, are thought to be one potential source of this response variability.9,10 The primary goal of this investigation was to examine the association of the personality traits from the FFM11 with treatment response to 2 widely used and effective treatments for depression—CBT and PHT.
Many investigators have examined the moderating effects of DSM-IV Axis II personality disorders and psychopathological dimensional personality traits on treatment outcome in MDD. This literature was summarized in a narrative review10 and in 2 more recent metaanalytic investigations, which focused exclusively on personality disorders.12,13 Mulder10 concluded that the strongest support for personality disorders as a predictor of treatment outcome for depressed patients comes from “the methodologically weakest studies.”p 368 Indeed, most studies cited were statistically underpowered, and (or) did not employ random assignment or other methods of treatment control. This conclusion was supported in the metaanalysis conducted by Kool et al,12 which included only well-designed RCTs; these investigators found no significant effects of personality disorders on treatment outcome. Although results from a more recent metaanalytic investigation led Newton-Howes et al13 to challenge Kool et al, Newton-Howes et al’s use of less stringent study inclusion criteria seems only to support Mulder’s conclusion that significant effects emerge from methodologically weaker research designs.
Although the review of Mulder10 included selected dimensional personality traits from the Eysenck Personality Questionnaire14 and its precursor, the Maudsley Personality Inventory15 and the TCI16 and its precursor, the Tridimensional Personality Questionnaire,17 investigations that used the NEO PI18 and the later developed NEO PI-R11 were not included. Presumably Mulder did not review the studies using these instruments, which were designed to assess the FFM, because the traits that compose this model were derived from nonclinical populations using mostly nonpsychopathological thematic sources, considered by many to measure only normal personality trait dimensions.19 The NEO inventories include scales that assess accepted personality psychopathological traits (for example, neuroticism and [low] extraversion) that are identical or similar to other instruments and personality traits assessed by them. More importantly, is that the NEO inventories include domains from the FFM not assessed directly by these other instruments that are seemingly good predictors of treatment response. For example, the conscientiousness trait may be related to tighter adherence to treatment protocol; and the agreeableness domain, which contains aspects of interpersonal relatedness, trust, and compliance, may increase therapeutic alliance.
Investigators examining whether the personality traits of the FFM predict treatment response in patients with MDD have reported mixed results. Bagby et al20 found that higher scores on extraversion predicted a positive outcome to various anti-depressant medications, even after controlling for depression severity; Du et al21 found that higher scores on the agreeableness domain predicted response to fluoxetine; whereas Peterson et al22 reported that none of the domain scores from the FFM predicted treatment response in depressed subjects treated with fluoxetine.
Comparatively, fewer investigations have been conducted examining the role of personality in differential response to different types of empirically supported interventions for MDD. Numerous investigations examining potential treatment-specific moderating effects of clinical characteristics, including personality, on treatments for depression have used data from the TDCRP.23 The TDCRP is a multisite study comparing the effectiveness of 3 forms of treatment for depression and a placebo condition—CBT, IPT, PHT plus clinical management, and a placebo plus clinical management. In the first of these investigations, Sotsky et al24 reported that better social functioning and general well-being predicted positive treatment outcome among those treated with IPT. Those with reduced depressogenic cognitions, as measured by the DAS,25 responded more positively to CBT and PHT plus clinical management than those in the placebo condition. In a subsequent analysis, Blatt et al26,27 examined the effects of 2 personality constructs—perfectionism and need for approval—also measured by the DAS, and reported that perfectionism predicted poorer treatment response across all treatment modalities, suggesting no treatment-specific moderating effects for these personality characteristics.
In a naturalistic treatment outcome study, Rector et al28 did report personality by treatment moderating effects. In this study, depressed patients were treated with either CBT or PHT; the personality construct of self-criticism, as measured by the Depressive Experiences Questionnaire,29 predicted poorer response to CBT but not PHT. McBride et al30 reported outcome from 2 psychotherapy treatment cells extracted from a larger RCT treatment of depression investigation; patients who scored higher on attachment avoidance, as measured by the Relationship Scales Questionnaire,31 showed greater reduction in depression severity with CBT, compared with IPT. A similar set of personality by type of psychotherapy outcome were reported recently by Joyce et al.32 In a RCT depression trial in which participants were randomized to receive either CBT or IPT, investigators reported that the presence of high levels of avoidant and schizoid personality disorder symptoms, as measured by SCID-II,33 were associated with poorer outcome to IPT, compared with CBT. These authors also found that higher scores on the personality trait of harm avoidance, measured with the TCI,16 were associated with a poorer outcome in IPT but not CBT.
The goal of the current investigation was to continue this line of research examining the interaction between personality and treatment type in the prediction of differential treatment response using 2 well known and effective treatments for MDD—CBT and PHT—using a comprehensive taxonomy of universal personality traits that is currently the most predominant and frequently used dimensional model of personality—the FFM.11 Despite its widespread use, to date no study has examined personality and its treatment-specific moderating effects using the FFM. A common shortcoming in studies examining personality and treatment outcome is the lack of statistical power.10 We combined data from 2 RCTs, which included CBT and PHT treatment cells. The combined sample size (n = 275) generated enough power to detect at least moderate effect sizes, considered the minimal effect to be clinically meaningful.34
Method
Subjects
The sample comprised 105 men and 175 women (mean age 41.9 years, SD 11.90), who participated in one of 2 randomized trials (Trial A/Trial B) at the CAMH. Both trials had the approval of the Research Ethics Board at the CAMH. A proportion (16.7%) of the data from Trial A is used in a previous manuscript.30
Inclusion criteria for both trials were: aged between 18 and 70 years; minimum of 8 years of education; verbal fluency in English; capacity to give written informed consent; meet the diagnostic criteria for a DSM-IV major depressive episode, assessed with the Structured Clinical Interview for DSM-IV, Axis I Disorders, Version 2.0—Patient Version35; and willing to be randomized. Exclusion criteria were: presence or history of bipolar disorder, psychotic disorders, or substance use disorders; presence of borderline or antisocial personality disorder, as assessed by the SCID-II; current treatment with antidepressant medication or previous treatment with electroconvulsive therapy; or concurrent active medical illness.
Subjects were solicited through advertisements in local media. In Trial A, 307 were assessed following a telephone screen. Among these, 131 were excluded because they did not meet inclusion criteria; an additional 4 met the criteria but chose not to participate. Among the remaining 171, 56 were randomized to CBT, 57 to IPT, and 59 to PHT. Of these, 36 completed CBT, 38 IPT, and 32 PHT. As Trial B did not include an IPT condition, we did not include this treatment arm. In Trial B, 301 were assessed following an initial telephone screen. Among these, 141 were excluded because they did not meet inclusion criteria. Among the remaining 160, 90 were randomized to CBT and 70 to PHT; 69 completed CBT and 37 completed PHT.
Measures
Hamilton Depression Rating Scale
The HDRS is a semi-structured, clinician-rated interview designed to assess severity of depression; currently, it is the most widely used measure of depression severity in clinical trials.36,37
Revised NEO Personality Inventory
The NEO PI-R is a self-report questionnaire designed to assess the FFM.11 This instrument yields scale scores for 5 higher-order personality domains—neuroticism, extraversion, openness-to-experience, agreeableness, and conscientiousness—as well as the 30 lower-order facet traits (6 per each domain) (Table 1).
Table 1.
Features of individuals scoring high and low on measures of FFM domains and facets
| FFM domains and facets | High | Low |
|---|---|---|
| Neuroticism | Sensitive, emotional | Secure, hardy |
| Anxiety | Fearful, worrying | Calm, relaxed |
| Angry hostility | Irritable, impatient | Easygoing, gentle |
| Depression | Pessimistic, moody | Contented, self-confident |
| Self-consciousness | Shy, timid | Self-assured, poised |
| Impulsiveness | Loud, hasty | Satisfied, relaxed |
| Vulnerability | Panicky, dependent | Efficient, alert |
| Extraversion | Outgoing, active | Reserved, serious |
| Warmth | Friendly, cheerful | Aloof, formal |
| Gregariousness | Sociable, outgoing | Withdrawn, reclusive |
| Assertiveness | Aggressive, forceful | Tentative, passive |
| Activity | Energetic, determined | Leisurely, unperturbed |
| Excitement seeking | Daring, spunky | Faint-hearted, uninterested |
| Positive emotions | Jolly, spontaneous | Nonexuberant, low-spirited |
| Openness | Innovative, inquisitive | Practical, traditional |
| Fantasy | Dreamy, imaginative | Prosaic, realistic |
| Aesthetics | Artistic, original | Uninterested, objective |
| Feelings | Excitable, insightful | Apathetic, indifferent |
| Actions | Adventurous, versatile | Mild, routine-oriented |
| Ideas | Inventive, curious | Traditional, dogmatic |
| Values | Unconventional, flirtatious | Conservative, cautious |
| Agreeableness | Compassionate, affable | Hardheaded, skeptical |
| Trust | Naive, forgiving | Suspicious, wary |
| Straightforwardness | Sincere, frank | Clever, shrewd |
| Altruism | Generous, kind | Selfish, unwilling |
| Compliance | Meek, docile | Headstrong, intolerant |
| Modesty | Humble, self-effacing | Proud, haughty |
| Tendermindedness | Sympathetic, soft-hearted | Obstinate, logical |
| Conscientiousness | Assiduous, well-organized | Easygoing, careless |
| Competence | Thorough, resourceful | Confused, inept |
| Order | Precise, methodical | Absentminded, careless |
| Dutifulness | Moral, scrupulous | Defensive, distractible |
| Achievement striving | Ambitious, industrious | Lackadaisical, aimless |
| Self-Discipline | Efficient, organized | Lazy, absent-minded |
| Deliberation | Cautious, patient | Hasty, slapdash |
These domains, and the facet traits that compose them, were shown to be heritable,38 biologically-based,39 and generalizable across languages, cultures, and countries.40,41 Investigators have shown that domain and facet traits can be validly and reliably assessed in psychiatric patients, even in the context of acute symptom change.42-44
Procedure and Treatment Protocols
Callers interested in either trial telephoned intake workers, who provided more information about the study. If continued interest was expressed, a screening interview for study eligibility was performed over the telephone and those meeting study criteria were invited for a face-to-face interview. Research assistants trained in diagnostic interviewing performed the assessment at CAMH. Those eligible were offered the opportunity to participate and if they agreed to randomization were asked to provide written informed consent and then assigned to one of the treatment conditions.
Those randomized to CBT received 16 to 20 sessions of treatment. The decision to extend therapy beyond 16 weeks was implemented if treatment remission was not achieved at 16 weeks. If remission was not achieved by 20 weeks, treatment was terminated. Greenberger and Padesky’s45 Mind Over Mood manual was used to guide treatment in Trial A, and the protocol developed by Beck et al46 was used in Trial B. Master’s and doctoral level psychologists trained in CBT served as the therapists. Those randomized to the PHT condition were treated for 16 to 20 weeks with one of several SSRIs using standardized protocols for initial dosing and adjustment in dose level, if necessary. The specific antidepressant chosen was left to the discretion of the treating psychiatrist. Those unable to continue with the prescribed medication owing to side effects and (or) lack of response were prescribed another medication only during the first 2 weeks of the protocol. The medications and the corresponding dosages were: bupropion, 150 to 300 mg; citalopram, 20 to 80 mg; fluoxetine, 20 to 60 mg; paroxetine, 20 to 40 mg; phenelizine, 60 to 90 mg; venlafaxine, 75 to 225 mg. Treatment was delivered by psychiatrists with experience treating MDD pharmacologically.
Results
Comparing Trial A and Trial B
We first compared the patients in Trial A and Trial B across numerous demographic and clinical variables. There were no significant differences across the 2 trials in the proportion of completers, compared with noncompleters, across the 2 trials, χ2 = 1.21, df 1, P = 0.48. Subjects in Trial A were older than those in Trial B, mean 41.8, SD 11.81, compared with mean 35.9, SD 11.96, t = 3.08, P = 0.002. As these ages are considered to be in the same age cohort according to the Canadian Census, they were judged as developmentally similar and we did not control for age. There were no significant differences across the 2 trials in the NEO PI-R personality domain traits, with, in all cases t < 1.58, P > 0.12, or facet traits, with, in all cases t < 1.58, P > 0.12.
Subjects in Trial A had significantly lower pretreatment HDRS scores, compared with those in Trial B, mean 17.8, SD 3.19, compared with mean 19.3, SD 3.94, t = 2.56, P < 0.01; however, there were no differences in posttreatment scores, mean 5.2, SD 5.05, compared with mean 6.5, SD 5.0, t = 1.64, P = 0.10; and the magnitude of change in HDRS scores from pretreatment to posttreatment did not differ between trials, Δmean 12.6, SD 5.84, compared with Δmean 12.74, SD 5.88, t = 0.18, P = 0.85. Remission rate, defined as a more than 50% decrease in HDRS scores from treatment entry to treatment completion and a final HDRS score of less than 8,47 was not significantly different between trials, χ2 = 2.66, df 1, P = 0.10. Based on these results, we combined the 2 trials for all analyses. For both trials the sample was predominantly Caucasian and Canadian-born. The combined sample was composed of 62 men and 111 women (mean age 38.10 years, SD 12.21). Pretreatment HDRS was mean 18.69, SD 3.72 and posttreatment HDRS was mean 6.02, SD 5.07, with a response rate of 69% overall.
Treatment Group Differences
There were no significant differences between the patients receiving CBT, compared with PHT, for age, t = 1.18, P = 0.12, or distribution of men and women, χ2 = 0.73, df 1, P = 0.39, nor were there any differences between the treatment groups for the personality domain traits, with, in all cases t < 1.90, mean value for P = 0.53, or personality facet traits, t < 1.68, mean value for P = 0.47.
Subjects in both the CBT and PHT treatment cells exhibited significant reductions in depressive severity. For CBT, pre-treatment HDRS scores were mean 18.9, SD 3.53; posttreatment HDRS scores, mean 6.6, SD 4.98, t = 21.90, df = 104, P = 0.01, Cohen’s d = 2.85. For PHT, pretreatment HDRS scores were mean 18.4, SD 4.01; posttreatment HDRS scores mean 5.06, SD 5.10, t = 18.30, df = 67, P = 0.01, Cohen’s d = 2.91. The mean change in HDRS scores in the CBT condition was Δmean 12.22, SD 5.72; and in the PHT condition, Δmean 13.38, SD 6.03; the difference in mean change and HDRS change scores across treatment conditions was nonsignificant, t = 1.28, df = 171, P = 0.20. The remission rate was greater in the PHT (78%), compared with CBT (64%), χ2 = 3.88, df = 1, P = 0.05.
Personality and Treatment Outcome
Hierarchical linear regressions were conducted for each of the 5 NEO PI-R domain traits and 30 facet traits. The criterion variable was posttreatment HDRS score. In Step 1, pre-treatment HDRS scores were entered to control for pretreatment depression severity. In Step 2, treatment condition was entered as a main effect; as there were no differences in outcome between treatment conditions, this variable was not interpreted and was only used to create the treatment condition by personality interaction. In Step 3, one of the 5 domain traits or one of the 30 facet traits was entered as a main effect for personality. In Step 4, the treatment condition by personality interaction was entered. A significant main effect of personality indicates that personality predicts outcome regardless of treatment type; a significant interaction effect indicates that personality predicts differential response to treatment type. As the facets within a domain are correlated, a facet was considered a meaningful and unique moderator only if it remained significant after controlling for the common variance associated with the other remaining facets in that domain. To this end, the first unrotated factor of a common factor analysis of the remaining 5 facets, which represents the variance common to those facets, was entered into the regression as both a main effect and an interaction. Facets were considered unique predictors only if they contributed significantly following the inclusion of this measure of common facet variance.
Personality Domain Traits as Predictors of Treatment Outcome
Main Effects
There was only one significant main effect for openness, β = −0.26, t = 3.61, P < 001, R2 = 0.11. Higher scores on openness at the beginning of treatment were associated with lower depression severity at treatment completion.
Interaction Effects
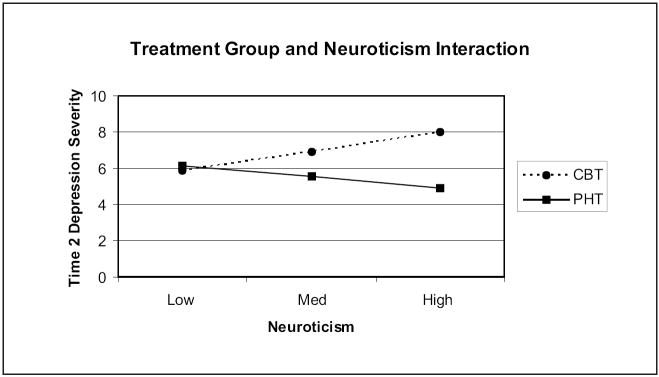
There was only one significant interaction effect for neuroticism, β = 0.90, t = 2.12, P < 0.04, R2 = 0.07. Higher scores at pretreatment were associated with lower posttreatment depression severity for those receiving PHT, compared with those receiving CBT (Figure 1).
Figure 1.
Personality and treatment group interaction—FFM domain traits
To evaluate the clinical significance of this interaction effect, we assessed the proportion of remission rates attendant on high or low status (SD 1) on this personality trait. Patients with high scores were more likely classified as remitters if treated with PHT, compared with CBT (75%, compared with 57%).
Personality Facet Traits as Predictors of Treatment Outcome
Main Effects
There were 6 significant main effects for the personality facet traits: 2 from the extraversion domain—excitement seeking (β = −0.17, t = 2.29, P < 0.02, R2 = 0.07) and positive emotions (β = −0.19, t = 2.59, P = 0.01, R2 = 0.08); and 4 from the openness-to-experience domain—fantasy (β = −0.18, t = 2.45, P = 0.02, R2 = 0.07), aesthetics (β = −0.18, t = 2.44, P = 0.02, R2 = 0.07), actions (β = −0.18, t = 2.40, P = 0.02, R2 = 0.07), and values (β = −0.22, t = 3.03, P = 0.003, R2 = 0.09). Excitement seeking and positive emotions did not remain significant after controlling for each of the remaining 5 extraversion facets.
For the facets from the openness domain, fantasy (ΔR2= 0.06, F1,169 = 11.77, P = 0.001); aesthetics (ΔR2 = 0.07, F1,169 = 13.09, P < 0.001); actions (ΔR2 = 0.06, F1,169 = 11.23, P < 0.001) and values (ΔR2 = 0.05, F1,169 = 10.04, P = 0.002) all remained significant after controlling for each of the remaining 5 openness facets. Patients with higher scores on these facets were associated with lower levels of depression severity at treatment completion.
Interaction Effects
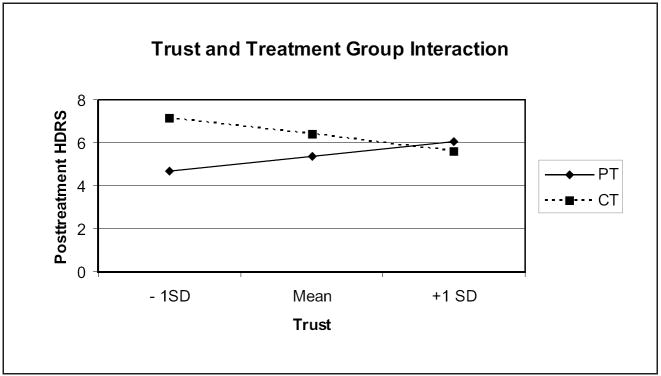
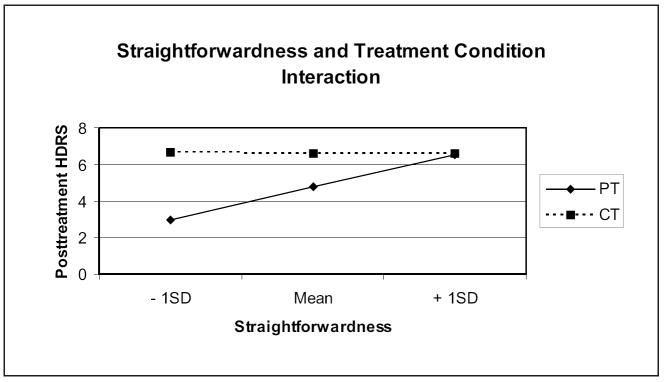
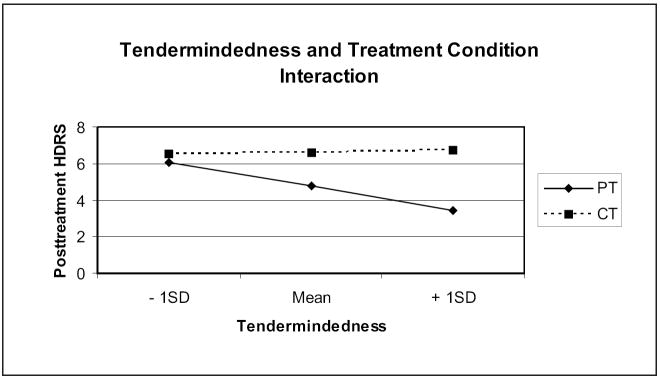
There were 5 significant personality by treatment interaction effects: 2 from the neuroticism domain—angry hostility (β = 0.62, t = 2.32, P = 0.02, R2 = 0.07) and self-consciousness (β = 0.64, t = 2.06, P = 0.04, R2 = 0.07), and 3 from the agreeableness domain—trust (β = −0.53, t = 2.05, P = 0.04, R2 = 0.07), straightforwardness (β = −.84, t = 2.32, P = 0.02, R2 = 0.09), and tendermindedness (β = 0.80, t = 2.02, P = 0.04, R2 = 0.08). Angry hostility and self-consciousness did not remain significant after controlling for the remaining 5 neuroticism facets, indicating that it is the variance common to all of the neuroticism facets that is associated with this moderation effect.
For the facets from the agreeableness domain, trust (ΔR2 = 0.04, F1,167 = 6.46, P = 0.01), straightforwardness (ΔR2 = 0.02, F1,167 = 4.18, P = 0.04), and tendermindedness (ΔR2 = 0.04, F1,167 = 7.20, P < 0.01), all remained significant after controlling for the remaining 5 agreeableness facets. Lower trust and straightforwardness scores were associated with lower depression severity following treatment with PHT, compared with those treated with CBT. Higher tendermindedness scores were associated with lower depression severity in the PHT condition, compared with those treated with CBT. Patients categorized as low scorers on trust were more likely to respond if treated with PHT, compared with CBT (86%, compared with 56%). Similarly, patients categorized as low scorers on straightforwardness were more likely to respond if treated with PHT, compared with CBT (100%, compared with 62%). Finally, patients categorized as high scorers on tendermindedness were more likely to respond if treated with PHT, compared with CBT (80%, compared with 54%).
Discussion
In the current study, depressed patients with higher scores on neuroticism are more likely to respond to PHT, compared with CBT. As neuroticism reflects the heritable predisposition to experience high levels of negative affect, one explanation for this result is that those with higher scores on this trait may be too emotionally dysregulated to recruit the psychological resources needed to enable cognitive strategies required for CBT. PHT may directly target neural systems involved in dysregulated emotions, circumventing the cognitive requirements for response to CBT. This interpretation is bolstered by outcomes from earlier studies indicating antidepressants,43 especially SSRIs,48 decrease levels of negative affect. One possible treatment implication of this finding is the potential benefit of treatment sequencing,49 such that patients with high levels of neuroticism might prove to be best treated initially with pharmacotherapy, and then receive a trial of CBT, when they are able to fully use CBT strategies. As CBT has been demonstrated to confer a slight advantage over antidepressant medication in the prevention of depression recurrence,50 this sequencing strategy maximizes the benefits of the superior effects of SSRIs in the treatment of the acute episode, and the protective effects of CBT for recurrence.
Patients scoring lower on the trust facet, a lower-order trait of the agreeableness domain, which assesses interpersonal aspects of personality, were more likely to respond to PHT, compared with CBT. Low scorers on the trust personality trait facet are described as cynical or skeptical and tend to see others as dishonest; these characteristics may impede the formation of a therapeutic alliance, which is the cornerstone of psychotherapy,51 including CBT.52 Although the capacity and disposition to trust is important in any physician–patient relationship, the results from the current study suggest it plays a less critical role in medication management. The straightforwardness facet, also of the agreeableness domain, reflects tendency toward sincerity, with high scorers on this trait described as frank and ingenuous. Low scorers may have a higher response rate to PHT as they benefit most from treatments that do not require disclosure of feelings. Curiously, high scorers on the tendermindedness facet trait had better outcome when treated with PHT, compared with CBT. High scorers on this trait are described as sympathetic and soft-hearted, whereas low scorers are described as obstinate and logical. Of the 4 significant interaction effects, this outcome is not readily understandable and may simply reflect a spurious effect.
Although the primary goal of the current investigation was to examine personality and treatment-specific moderating effects, several personality traits emerged as moderators of general treatment outcome. Facets from both the extraversion and openness-to-experience domain demonstrated significant predictive capacity; however, openness-to-experience was the only significantly predicting domain trait and 4 of 6 facets from this domain predicted treatment outcome after removing unique variance associated with the other facets, suggesting both general and unique predictive components associated with this personality trait. This result is particularly interesting as this personality domain is unique to the FFM in relation to the dimensional models of personality psychopathology and has been dismissed by most as unrelated to psychopathology.53-55 Openness reflects “the recurrent need to enlarge and examine experience”—curiosity and imagination and flexibility in considering novel ideas, behaviours, and feelings.56, p 167 This set of traits would seem to describe a characteristic predictive of response to psychotherapy; however, it may also reflect a general receptivity to treatment in general. To our knowledge, this is the first study to examine the effects of openness in the prediction of treatment outcome to both psychotherapy and PHT and the finding here certainly requires replication and further exploration.
Conclusion
The results from the current investigation suggest that treatment response for those with MDD may be optimized if patient personality traits are taken into consideration. One limitation of the current investigation is that our data analytic approach was designed to minimize type II error. We believe the significant results obtained are not attributable to chance, as they are logical and consistent with the broader literature on treatment outcome in MDD. We used stringent statistical tests and criteria to examine the unique and specific components of the significantly predicting personality traits, which minimize spurious and redundant effects.
One potential limitation of this investigation is that we relied on a single dimensional model—the FFM—using a self-report method of assessment. As the FFM readily captures the most important aspects of other dimensional models of personality57 and even DSM-IV Axis II personality disorders,58 we believe the results were highly generalizable. Recent studies have also demonstrated that the self-report measure of the FFM used in this study (NEO PI-R, Form S) is highly correlated with third-person informant ratings59 and with structured interviews of the FFM,60,61 even for depressed patients in the acute phase of their depressive illness.62
The results of the current investigation are only generalizable to one type of psychotherapy (CBT) and the antidepressant medications used in this study. As CBT and IPT have produced their own personality by treatment-specific moderating effect in comparison with one another,30,32 the outcome may be different with IPT in comparison with PHT. The lack of statistical power prohibited us from examining that effect in this study. Similarly, one can only extrapolate findings from the current study to the antidepressant medications used, predominantly SSRIs. For example, as the short variant of the serotonin transporter polymorphism, which is thought to decrease transporter expression and serotonin reuptake,63 and has been linked to neuroticism,64 the effect of PHT on high neuroticism in the current study may not hold for other classes of antidepressant medication that have no direct action on the serotonin transporter, such as the noradrenergic and dopaminergic reuptake blockers and reversible monoamine oxidase inhibitors. Investigators conducting research in this area in the future might use other forms of empirically-supported psychotherapies and other classes of antidepressant medication. Finally, another potential limitation is that our exclusion criteria may limit the degree to which our results can be generalized to more pathological patients, especially those with high rates of comorbidity with other mental disorders.
Figure 2.
Personality and treatment group interaction—FFM facet traits
Figure 3.
Personality and treatment group interaction—FFM facet traits
Figure 4.
Personality and treatment group interaction—FFM facet traits
Acknowledgments
Funding and Support This study was supported by operating grants from the Ontario Mental Health Foundation (Dr Bagby as principle investigator), the Canadian Institute of Health Research (Dr Segal as principle investigator) and, in part, the National Institute on Aging/National Institute of Health (US) Intramural Research Program (Dr Costa). Dr Bagby and Dr Segal also received Senior Research Fellowship Awards from the Ontario Mental Health Foundation, which funded, in part, this work. Dr Quilty received a Postdoctoral Fellowship Award from the Canadian Institute of Health Research, which also, in part, funded this work.
Abbreviations used in this article
- CAMH
Centre for Addiction and Mental Health
- CBT
cognitive-behaviour therapy
- DAS
Dysfunctional Attitudes Scale
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- FFM
Five-Factor Model of Personality
- HDRS
Hamilton Depression Rating Scale
- IPT
interpersonal therapy
- MDD
major depressive disorder
- NEO PI-R
NEO Personality Inventory-Revised
- PHT
pharmacotherapy
- RCT
randomized controlled trials
- SCID-II
structured clinical interview for DSM-IV Axis II personality disorders
- SSRI
selective serotonin reuptake inhibitor
- TCI
temperament and character inventory
- TDCRP
National Institute of Mental Health Treatment of Depression Collaborative Research Program
References
- 1.American Psychiatric Association. Practice guidelines for the treatment of patients with major depressive disorder (revision) Am J Psychiatry. 2000;157 [PubMed] [Google Scholar]
- 2.Canadian Psychiatric Association, Canadian Network for Mood and Anxiety Treatments. Clinical guidelines for the treatment of depressive disorders. Can J Psychiatry. 2001;46:1S–92S. [PubMed] [Google Scholar]
- 3.Hollon SD, Thase ME, Markowitz JC. Treatment and prevention of depression. Psychological Science in the Public Interest. 2002;3:39–77. doi: 10.1111/1529-1006.00008. [DOI] [PubMed] [Google Scholar]
- 4.Judd LL, Paulus MP, Zeller P. The role of residual subthreshold depressive symptoms in early episode relapse in unipolar major depressive disorder. Arch Gen Psychiatry. 1999;56:764–765. doi: 10.1001/archpsyc.56.8.764. [DOI] [PubMed] [Google Scholar]
- 5.Thase ME, Haight BR, Richard N, et al. Remission rates following antidepressant therapy with bupropion or selective serotonin reuptake inhibitors: a meta-analysis of original data from 7 randomized controlled trials. J Clin Psychiatry. 2005;66:974–981. doi: 10.4088/jcp.v66n0803. [DOI] [PubMed] [Google Scholar]
- 6.Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40. doi: 10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- 7.Thase ME. How should efficacy be evaluated in randomized clinical trials of treatments for depression? J Clin Psychiatry. 1999;60:23–31. [PubMed] [Google Scholar]
- 8.Mattocks KM, Horwitz RI. Placebos, active control groups, and the unpredictability paradox. Biol Psychiatry. 2000;47:693–698. doi: 10.1016/s0006-3223(00)00839-8. [DOI] [PubMed] [Google Scholar]
- 9.Kennedy SH, Farvolden P, Cohen NL, et al. The impact of personality on the pharmacological treatment of depression. In: Rosenbluth M, Kennedy SH, Bagby RM, editors. Depression and personality: conceptual and clinical challenges. Washington (DC): American Psychiatric Publishing; 2005. pp. 97–119. [Google Scholar]
- 10.Mulder RT. Personality pathology and treatment outcome in major depression: a review. Am J Psychiatry. 2002;159:359–371. doi: 10.1176/appi.ajp.159.3.359. [DOI] [PubMed] [Google Scholar]
- 11.Costa PT, McCrae RR. Revised NEO personality inventory (NEO-PI-R) and NEO five-factor inventory (NEO-FFI) professional manual. Odessa (FL): Psychological Assessment Resources; 1992. [Google Scholar]
- 12.Kool S, Schoevers R, de Maat S, et al. Efficacy of pharmacotherapy in depressed patients with and without personality disorders: a systematic review and meta-analysis. J Affect Disord. 2005;88:269–278. doi: 10.1016/j.jad.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 13.Newton-Howes G, Tyrer P, Johnson T. Personality disorder and the outcome of depression: meta-analysis of published studies. Br J Psychiatry. 2006;88:13–20. doi: 10.1192/bjp.188.1.13. [DOI] [PubMed] [Google Scholar]
- 14.Eysenck HJ, Eysenck SB. Manual of the Eysenck personality inventory. London (GB): University of London; 1964. [Google Scholar]
- 15.Eysenck HJ. Manual of the Maudsley personality inventory. London (GB): University of London Press; 1959. [Google Scholar]
- 16.Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Arch Gen Psychiatry. 1993;50:975–989. doi: 10.1001/archpsyc.1993.01820240059008. [DOI] [PubMed] [Google Scholar]
- 17.Cloninger CR. A systematic method for clinical description and classification of personality variants. A proposal. Arch Gen Psychiatry. 1987;44:573–588. doi: 10.1001/archpsyc.1987.01800180093014. [DOI] [PubMed] [Google Scholar]
- 18.Costa PT, McCrae RR. The NEO personality inventory manual. Odessa (FL): Psychological Assessment Resources; 1985. [Google Scholar]
- 19.Harkness AR, McNulty JL. The personality psychopathology five (PSY-5): issues from the pages of a diagnostic manual instead of a dictionary. In: Strack S, Lorr M, editors. Differentiating normal and abnormal personality. New York (NY): Springer Publishing Co; 1994. pp. 291–315. [Google Scholar]
- 20.Bagby RM, Joffe RT, Parker JDA, et al. Major depression and the five-factor model of personality. J Personal Disord. 1995;9:224–234. [Google Scholar]
- 21.Du L, Bakish D, Ravindran AV, et al. Does fluoxetine influence major depression by modifying five-factor personality traits? J Affect Disord. 2002;71:235–241. doi: 10.1016/s0165-0327(01)00370-6. [DOI] [PubMed] [Google Scholar]
- 22.Petersen T, Papakostas GI, Bottonari K, et al. NEO-FFI factor scores as predictors of clinical response to fluoxetine in depressed outpatients. Psychiatry Res. 2002;109:9–16. doi: 10.1016/s0165-1781(01)00359-6. [DOI] [PubMed] [Google Scholar]
- 23.Elkin I, Shea MT, Watkins JT, et al. National institute of mental health treatment of depression collaborative research program: general effectiveness of treatments. Arch Gen Psychiatry. 1989;46:971–982. doi: 10.1001/archpsyc.1989.01810110013002. [DOI] [PubMed] [Google Scholar]
- 24.Sotsky SM, Glass DR, Shea MT, et al. Patient predictors of response to psychotherapy and pharmacotherapy: findings in the NIMH treatment of depression collaborative research program. Am J Psychiatry. 1991;148:997–1008. doi: 10.1176/ajp.148.8.997. [DOI] [PubMed] [Google Scholar]
- 25.Weissman AN, Beck AT. Developmental validation of the dysfunctional attitude scale. Paper presented at the Annual Meeting of the Association of Advancement of Behavioral Therapy; Chicago (IL). 1978. [Google Scholar]
- 26.Blatt SJ, Quinlan DM, Pilkonis PA, et al. Impact of perfectionism and need for approval on the brief treatment of depression: the national institute of mental health treatment of depression collaborative research program revisited. J Consult Clin Psychol. 1995;63:125–132. doi: 10.1037//0022-006x.63.1.125. [DOI] [PubMed] [Google Scholar]
- 27.Blatt SJ, Zuroff DC, Bondi CM, et al. When and how perfectionism impedes the brief treatment of depression: further analyses of the national institute of mental health treatment of depression collaborative research program. J Consult Clin Psychol. 1998;66:423–428. doi: 10.1037//0022-006x.66.2.423. [DOI] [PubMed] [Google Scholar]
- 28.Rector NA, Bagby RM, Segal ZV, et al. Self-criticism and dependency in depressed patients treated with cognitive therapy or pharmacotherapy. Cognit Ther Res. 2000;24:571–584. [Google Scholar]
- 29.Blatt SJ, D’Affitti JP, Quinlan DM. Experiences of depression in normal young adults. J Abnorm Psychol. 1976;85:383–389. doi: 10.1037//0021-843x.85.4.383. [DOI] [PubMed] [Google Scholar]
- 30.McBride C, Atkinson L, Quilty LC, et al. Attachment as moderator of treatment outcome in major depression: a randomized control trial of interpersonal psychotherapy versus cognitive behavior therapy. J Consult Clin Psychol. 2006;74:1041–1054. doi: 10.1037/0022-006X.74.6.1041. [DOI] [PubMed] [Google Scholar]
- 31.Griffin DW, Bartholomew K. The metaphysics of measurement: the case of adult attachment. In: Bartholomew K, Perlman D, editors. Advances in personal relationships: attachment processes in adulthood. London (GB): Jessica Kingsley; 1994. pp. 17–52. [Google Scholar]
- 32.Joyce PR, McKenzie JM, Carter JD, et al. Temperament, character and personality disorders as predictors of response to interpersonal psychotherapy and cognitive-behavioural therapy for depression. Br J Psychiatry. 2007;190:503–508. doi: 10.1192/bjp.bp.106.024737. [DOI] [PubMed] [Google Scholar]
- 33.First MB, Gibbon M, Spitzer RL, et al. User’s guide for the structured clinical interview for DSM–IV Axis II personality disorders. Washington (DC): American Psychiatric Press; 1997. [Google Scholar]
- 34.Cohen J. A power primer. Psych Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 35.First MB, Spitzer RL, Gibbon M, et al. Structured clinical interview for DSM–IV Axis I disorders—patient edition (version 2) New York (NY): Biometric Research Institute; 1995. [Google Scholar]
- 36.Hamilton M. Development of a rating scale for primary depressive illness. J Clin Psychol. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 37.Bagby RM, Ryder AG, Schuller DR, et al. The Hamilton depressive rating scale: have the gold standard become a lead weight? Am J Psychiatry. 2004;161:2163–2177. doi: 10.1176/appi.ajp.161.12.2163. [DOI] [PubMed] [Google Scholar]
- 38.Ebstein RP. The molecular genetic architecture of human personality: beyond self-report questionnaires. Mol Psychiatry. 2006;11:427–445. doi: 10.1038/sj.mp.4001814. [DOI] [PubMed] [Google Scholar]
- 39.Levinson DF. The genetics of depression: a review. Bio Psychiatry. 2006;60:84–92. doi: 10.1016/j.biopsych.2005.08.024. [DOI] [PubMed] [Google Scholar]
- 40.McCrae RR, Allik J. The five-factor model across cultures. New York (NY): Kluwer-Plenum; 2002. [Google Scholar]
- 41.McCrae RR, Terracciano A. Universal features of personality traits from the observer’s perspective: data from 50 cultures. J Pers Soc Psychol. 2005;88:547–561. doi: 10.1037/0022-3514.88.3.547. [DOI] [PubMed] [Google Scholar]
- 42.Bagby RM, Bindseil KD, Schuller DR, et al. Relationship between the five-factor model of personality and unipolar, bipolar, and schizophrenic patients. Psychiatry Res. 1997;70:83–94. doi: 10.1016/s0165-1781(97)03096-5. [DOI] [PubMed] [Google Scholar]
- 43.Bagby RM, Levitan RD, Kennedy SH, et al. Selective alteration of personality in response to noradrenergic and serotonergic antidepressant medication in depressed sample: evidence of non-specificity. Psychiatry Res. 1999;86:211–216. doi: 10.1016/s0165-1781(99)00041-4. [DOI] [PubMed] [Google Scholar]
- 44.Costa PT, Bagby RM, Herbst JH, et al. Personality self-reports are concurrently reliable and valid during acute depressive episodes. J Affect Disord. 2005;89:45–55. doi: 10.1016/j.jad.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 45.Greenberger D, Padesky CA. Mind over mood: a cognitive therapy treatment manual for clients. New York (NY): Guilford Press; 1995. [Google Scholar]
- 46.Beck AT, Rush AJ, Shaw BF, et al. Cognitive therapy of depression. New York (NY): Guilford Press; 1979. [Google Scholar]
- 47.Frank E, Prien RF, Jarrett RB, et al. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Arch Gen Psychiatry. 1991;48:851–855. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- 48.Knutson B, Wolkowitz OM, Cole SW, et al. Selective alteration of personality and social behavior by serotonergic intervention. Am J Psychiatry. 1998;115:373–379. doi: 10.1176/ajp.155.3.373. [DOI] [PubMed] [Google Scholar]
- 49.Gaynes BN, Davis L, Rush AJ, et al. The aims and design of the sequenced treatment alternative to relieve depression (STAR*D) study. Prim Psychiatry. 2005;12:36–41. [Google Scholar]
- 50.Vittengl JR, Clark LA, Dunn TW, et al. Reducing relapse and recurrence in unipolar depression: a comparative meta-analysis of cognitive-behavioral therapy’s effects. J Consult Clin Psychol. 2007;75:475–488. doi: 10.1037/0022-006X.75.3.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Horvath AO, Bedi RP. In: The alliance in psychotherapy relationships that work: therapist contributions and responsiveness to patients. Norcross JC, editor. New York (NY): Oxford University Press; 2002. [Google Scholar]
- 52.Waddington L. The therapy relationship in cognitive therapy: a review. Behav Cogn Psychother. 2002;30:179–192. [Google Scholar]
- 53.Trull TJ, Durrett CA. Categorical and dimensional models of personality disorder. Annu Rev Clin Psychol. 2005;1:355–380. doi: 10.1146/annurev.clinpsy.1.102803.144009. [DOI] [PubMed] [Google Scholar]
- 54.Livesley WJ, Jang KL, Vernon PA. Phenotypic and genetic structure of traits delineating personality disorder. Arch Gen Psychiatry. 1998;55:941–948. doi: 10.1001/archpsyc.55.10.941. [DOI] [PubMed] [Google Scholar]
- 55.Widiger TA. Four out of five ain’t bad. Arch Gen Psychiatry. 1998;55:865–866. doi: 10.1001/archpsyc.55.10.865. [DOI] [PubMed] [Google Scholar]
- 56.McCrae RR, Costa RT. Conceptions and correlates of openness to experience. In: Hogan R, Johnson JA, Briggs SR, editors. Handbook of personality psychology. San Diego (CA): Academic Press; 1997. pp. 825–847. [Google Scholar]
- 57.O’Connor BP. A search for consensus on the dimensional structure of personality disorders. J Clin Psychol. 2005;61:323–345. doi: 10.1002/jclp.20017. [DOI] [PubMed] [Google Scholar]
- 58.Lynam DR, Widiger TA. Using the five-factor model to represent the DSM-IV personality disorders: an expert consensus approach. J Abnorm Psychol. 2001;110:401–412. doi: 10.1037//0021-843x.110.3.401. [DOI] [PubMed] [Google Scholar]
- 59.Miller JD, Pilkonis PA, Morse JO. Five-factor model prototypes for personality disorders: the utility of self-reports and observer ratings. Assessment. 2004;11:127–138. doi: 10.1177/1073191104264962. [DOI] [PubMed] [Google Scholar]
- 60.Trull TJ, Widiger TA, Useda JD, et al. A structured interview for the assessment of the five-factor model of personality. Psychol Assess. 1998;10:229–240. [Google Scholar]
- 61.Bagby RM, Costa PT, Widiger TA, et al. DSM-IV personality disorders and the five-factor model of personality: a multi-method examination of domain—and facet-level predictions. Eur J Pers. 2005;19:307–324. [Google Scholar]
- 62.Bagby RM, Rector NA, Bindsel K, et al. Self-report ratings and informants’ ratings of personalities of depressed outpatients. Am J Psychiatry. 1998;155:437–438. doi: 10.1176/ajp.155.3.437. [DOI] [PubMed] [Google Scholar]
- 63.Heinz A, Jones DW, Mazzanti C, et al. A relationship between serotonin ransporter genotype and in vivo protein expression and alcohol neurotoxicity. Bio Psychiatry. 2000;47:643–649. doi: 10.1016/s0006-3223(99)00171-7. [DOI] [PubMed] [Google Scholar]
- 64.Lesch K, Bengel D, Heils A, et al. Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science. 1996;274:1527–1531. doi: 10.1126/science.274.5292.1527. [DOI] [PubMed] [Google Scholar]