Abstract
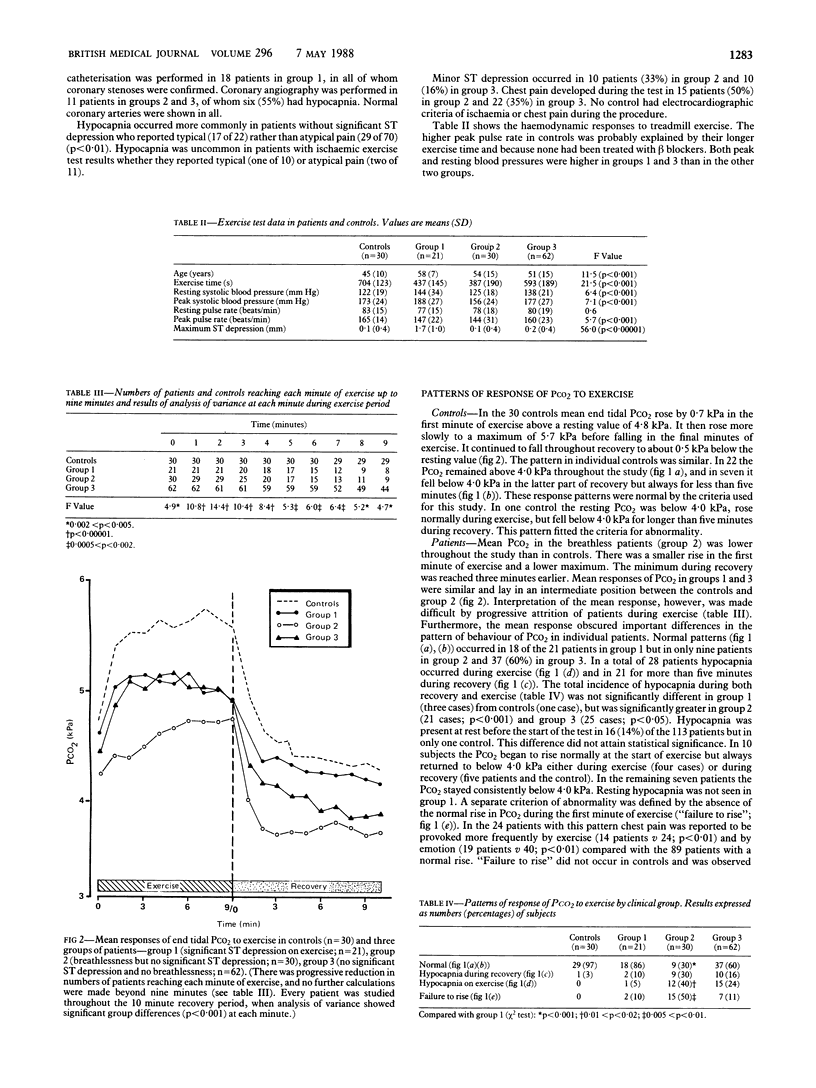
The end tidal partial pressure of carbon dioxide (Pco2) was measured during treadmill exercise in 30 normal controls and 113 patients referred for assessment of chest pain. Among the 92 patients without significant ST depression hypocapnia occurred more often in those reporting “typical” than “atypical” chest pain (17 of 22 patients compared with 29 of 70; p<0·01). Hypocapnia was uncommon in patients with significant ST depression whether reporting typical or atypical chest pain (one of 10 patients and two of 11, respectively).
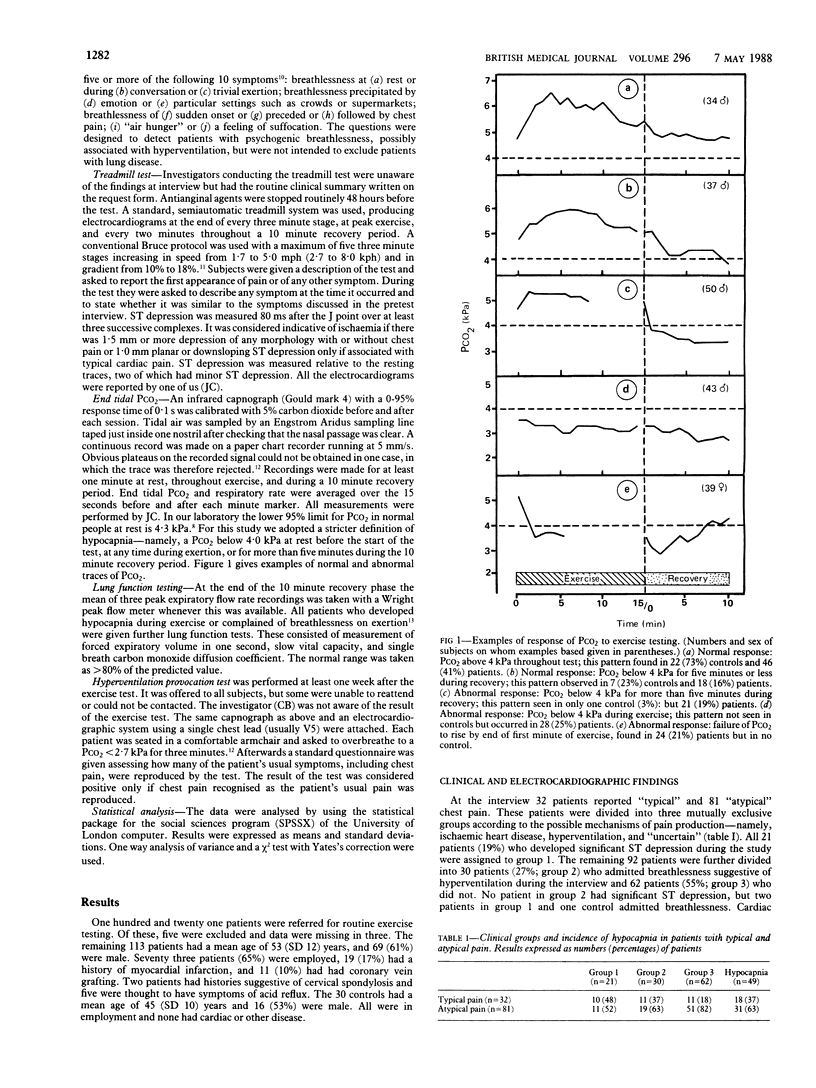
Hypocapnia at rest (Pco2 <4 kPa) occurred in 16 (14%) patients but in only one control. Hypocapnia occurred during or after exercise in only one control and three of the 21 patients with significant ST depression on exercise (group 1). The remaining 92 patients were divided into those with a history suggestive of hyperventilation (group 2; n=30) and those without (group 3; n=62). Hypocapnia developed significantly more often in both these groups (21 and 25 patients respectively) than in controls or patients with significant ST depression.
An abnormal response of the Pco2 to exercise provided objective data to support a clinical suspicion of chest pain induced by hyperventilation in 24 cases, suggested a cause for equivocal ST depression other than coronary stenosis in five patients, and led to the diagnosis of previously unsuspected respiratory disease in 14 patients.
Measurement of end tidal Pco2 gives additional valuable diagnostic information during the conventional treadmill exercise test in patients with both typical and atypical chest pain.
Full text
PDF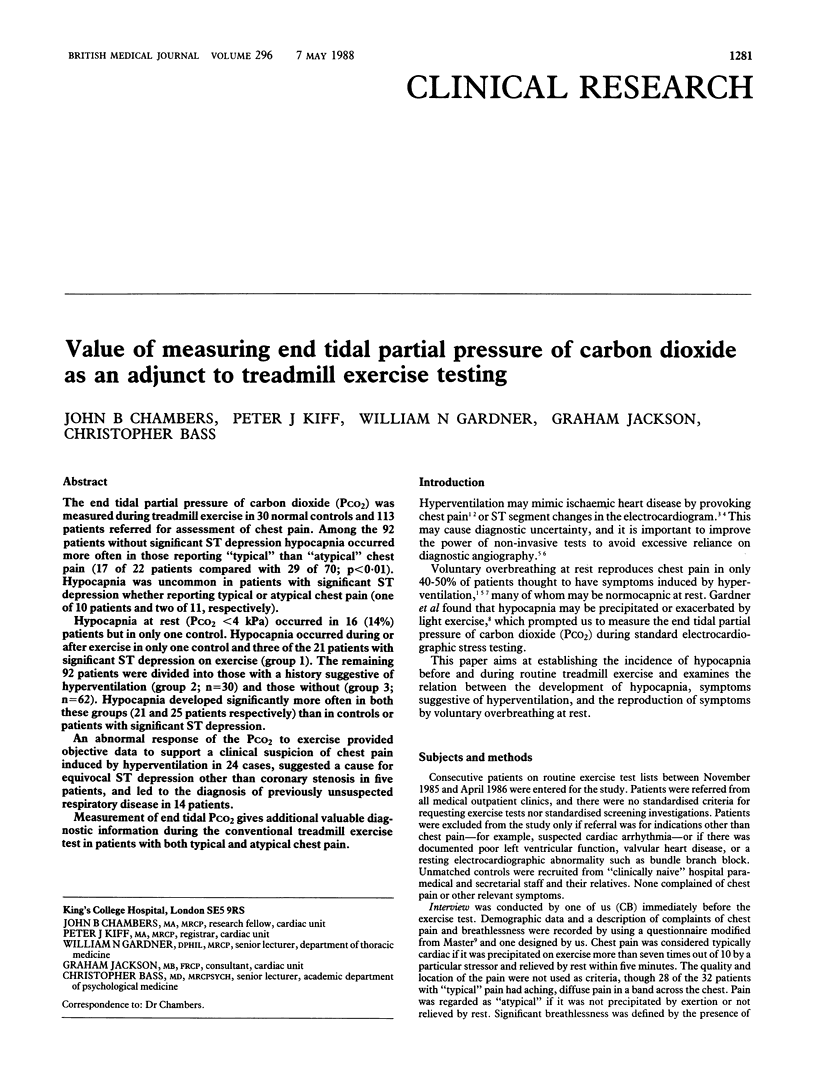


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bass C., Cawley R., Wade C., Ryan K. C., Gardner W. N., Hutchison D. C., Jackson G. Unexplained breathlessness and psychiatric morbidity in patients with normal and abnormal coronary arteries. Lancet. 1983 Mar 19;1(8325):605–609. doi: 10.1016/s0140-6736(83)91791-9. [DOI] [PubMed] [Google Scholar]
- Bass C., Gardner W. N. Respiratory and psychiatric abnormalities in chronic symptomatic hyperventilation. Br Med J (Clin Res Ed) 1985 May 11;290(6479):1387–1390. doi: 10.1136/bmj.290.6479.1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass C., Wade C., Hand D., Jackson G. Patients with angina with normal and near normal coronary arteries: clinical and psychosocial state 12 months after angiography. Br Med J (Clin Res Ed) 1983 Nov 19;287(6404):1505–1508. doi: 10.1136/bmj.287.6404.1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce R. A. Exercise testing of patients with coronary heart disease. Principles and normal standards for evaluation. Ann Clin Res. 1971 Dec;3(6):323–332. [PubMed] [Google Scholar]
- Burns B. H., Howell J. B. Disproportionately severe breathlessness in chronic bronchitis. Q J Med. 1969 Jul;38(151):277–294. [PubMed] [Google Scholar]
- Evans D. W., Lum L. C. Hyperventilation: An important cause of pseudoangina. Lancet. 1977 Jan 22;1(8004):155–157. doi: 10.1016/s0140-6736(77)91760-3. [DOI] [PubMed] [Google Scholar]
- FLETCHER C. M. The clinical diagnosis of pulmonary emphysema; an experimental study. Proc R Soc Med. 1952 Sep;45(9):577–584. [PubMed] [Google Scholar]
- Ferguson A., Addington W. W., Gaensler E. A. Dyspnea and bronchospasm from inappropriate postexercise hyperventilation. Ann Intern Med. 1969 Dec;71(6):1063–1072. doi: 10.7326/0003-4819-71-6-1063. [DOI] [PubMed] [Google Scholar]
- Freeman L. J., Conway A., Nixon P. G. Physiological responses to psychological challenge under hypnosis in patients considered to have the hyperventilation syndrome: implications for diagnosis and therapy. J R Soc Med. 1986 Feb;79(2):76–83. doi: 10.1177/014107688607900206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner W. N., Meah M. S., Bass C. Controlled study of respiratory responses during prolonged measurement in patients with chronic hyperventilation. Lancet. 1986 Oct 11;2(8511):826–830. doi: 10.1016/s0140-6736(86)92867-9. [DOI] [PubMed] [Google Scholar]
- Jones N. L., Robertson D. G., Kane J. W. Difference between end-tidal and arterial PCO2 in exercise. J Appl Physiol Respir Environ Exerc Physiol. 1979 Nov;47(5):954–960. doi: 10.1152/jappl.1979.47.5.954. [DOI] [PubMed] [Google Scholar]
- Joy M., Trump D. W. Significance of minor ST segment and T wave changes in the resting electrocardiogram of asymptomatic subjects. Br Heart J. 1981 Jan;45(1):48–55. doi: 10.1136/hrt.45.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lary D., Goldschlager N. Electrocardiographic changes during hyperventilation resembling myocardial ischemia in patients with normal coronary arteriograms. Am Heart J. 1974 Mar;87(3):383–390. doi: 10.1016/0002-8703(74)90081-7. [DOI] [PubMed] [Google Scholar]
- Magarian G. J. Hyperventilation syndromes: infrequently recognized common expressions of anxiety and stress. Medicine (Baltimore) 1982 Jul;61(4):219–236. [PubMed] [Google Scholar]
- Rasmussen K., Ravnsbaek J., Funch-Jensen P., Bagger J. P. Oesophageal spasm in patients with coronary artery spasm. Lancet. 1986 Jan 25;1(8474):174–176. doi: 10.1016/s0140-6736(86)90651-3. [DOI] [PubMed] [Google Scholar]
- Wasserman K., Van Kessel A. L., Burton G. G. Interaction of physiological mechanisms during exercise. J Appl Physiol. 1967 Jan;22(1):71–85. doi: 10.1152/jappl.1967.22.1.71. [DOI] [PubMed] [Google Scholar]
- Wood P. Da Costa's Syndrome (or Effort Syndrome). Lecture I. Br Med J. 1941 May 24;1(4194):767–772. doi: 10.1136/bmj.1.4194.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Caestecker J. S., Blackwell J. N., Brown J., Heading R. C. The oesophagus as a cause of recurrent chest pain: which patients should be investigated and which tests should be used? Lancet. 1985 Nov 23;2(8465):1143–1146. doi: 10.1016/s0140-6736(85)92676-5. [DOI] [PubMed] [Google Scholar]


