Abstract
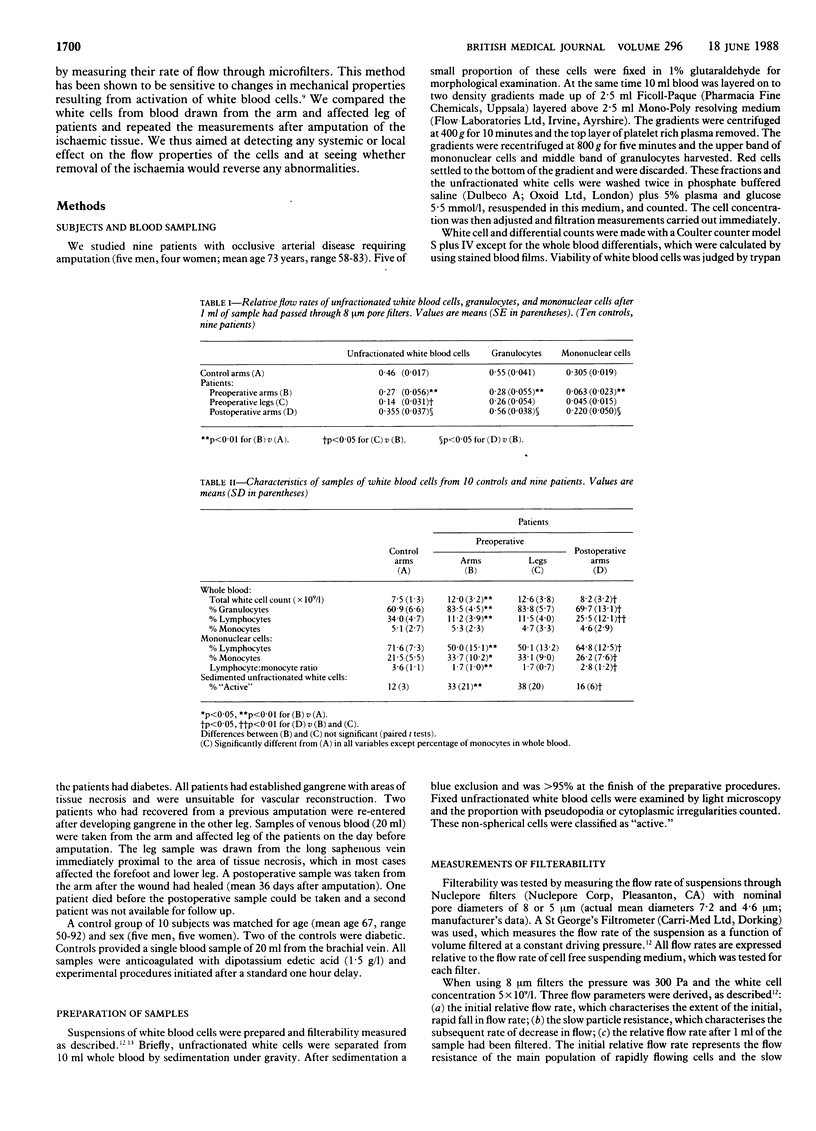
The possible role of white blood cells in tissue ischaemia has attracted recent interest. White blood cells can block narrow vessels, particularly if perfusion pressure is reduced or if the cells become activated. To investigate the role of white blood cells in ischaemia microfiltration techniques were used to measure the flow properties of these cells in patients with severe leg ischaemia before and after amputation. Compared with controls white blood cells from patients showed impaired ability to flow through 8 μm and 5 μm pore filters. This applied to fractionated granulocytes and mononuclear cells as well as to unfractionated mixed white blood cells. White blood cells from blood draining the ischaemic leg had worse filterability than those from arm blood of the same patients. After amputation of the ischaemic leg there was definite improvement, the flow properties of the cells being no longer significantly different from controls.
These abnormalities detected in white blood cells probably reflect activation of the cells by factors released in the ischaemic tissue. As activation alters the mechanical and adhesive properties of white blood cells, a vicious cycle of microcirculatory trapping at low perfusion pressure, activation, tissue damage, and further activation and trapping might contribute to the progressive worsening of tissue ischaemia.
Full text
PDF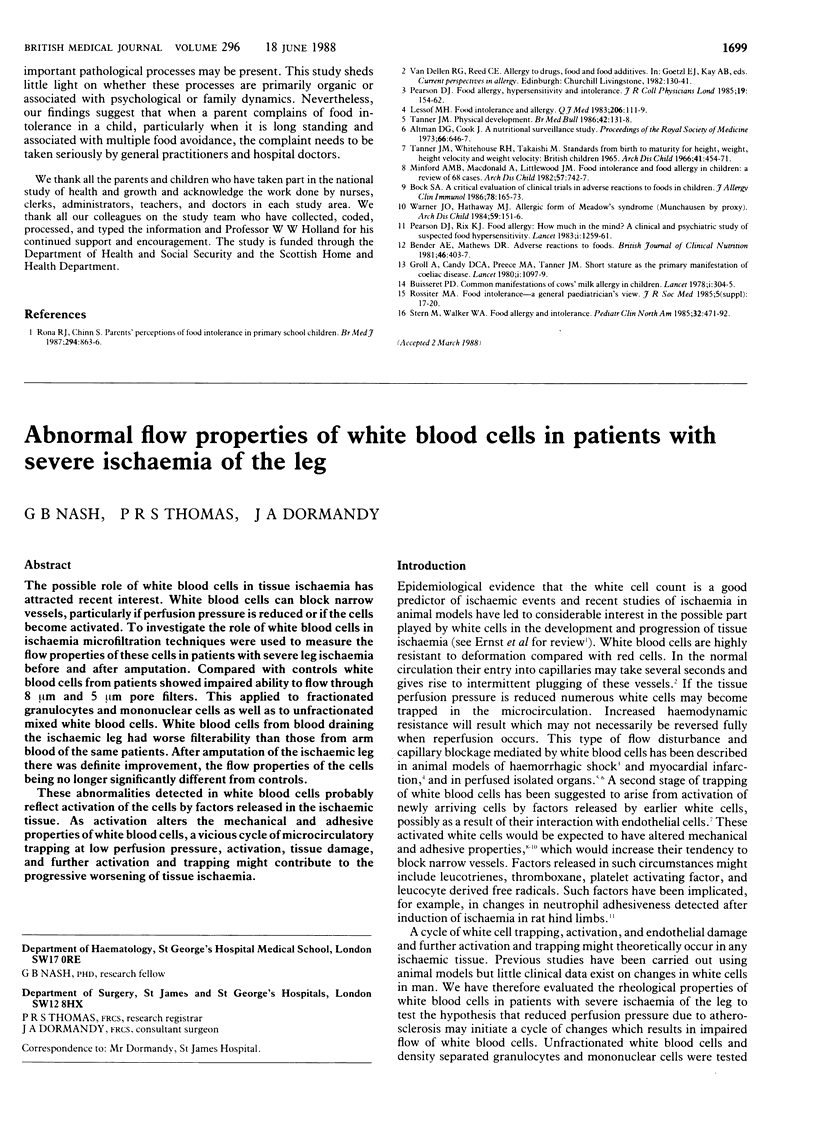

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anner H., Kaufman R. P., Jr, Kobzik L., Valeri C. R., Shepro D., Hechtman H. B. Pulmonary leukosequestration induced by hind limb ischemia. Ann Surg. 1987 Aug;206(2):162–167. doi: 10.1097/00000658-198708000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bengtson A., Holmberg P., Heideman M. The ischaemic leg as a source of complement activation. Br J Surg. 1987 Aug;74(8):697–700. doi: 10.1002/bjs.1800740816. [DOI] [PubMed] [Google Scholar]
- Braide M., Amundson B., Chien S., Bagge U. Quantitative studies on the influence of leukocytes on the vascular resistance in a skeletal muscle preparation. Microvasc Res. 1984 May;27(3):331–352. doi: 10.1016/0026-2862(84)90064-5. [DOI] [PubMed] [Google Scholar]
- Braide M., Blixt A., Bagge U. Leukocyte effects on the vascular resistance and glomerular filtration of the isolated rat kidney at normal and low flow states. Circ Shock. 1986;20(1):71–80. [PubMed] [Google Scholar]
- Engler R. L., Dahlgren M. D., Peterson M. A., Dobbs A., Schmid-Schönbein G. W. Accumulation of polymorphonuclear leukocytes during 3-h experimental myocardial ischemia. Am J Physiol. 1986 Jul;251(1 Pt 2):H93–100. doi: 10.1152/ajpheart.1986.251.1.H93. [DOI] [PubMed] [Google Scholar]
- Engler R. L., Schmid-Schönbein G. W., Pavelec R. S. Leukocyte capillary plugging in myocardial ischemia and reperfusion in the dog. Am J Pathol. 1983 Apr;111(1):98–111. [PMC free article] [PubMed] [Google Scholar]
- Ernst E., Hammerschmidt D. E., Bagge U., Matrai A., Dormandy J. A. Leukocytes and the risk of ischemic diseases. JAMA. 1987 May 1;257(17):2318–2324. [PubMed] [Google Scholar]
- Harlan J. M. Leukocyte-endothelial interactions. Blood. 1985 Mar;65(3):513–525. [PubMed] [Google Scholar]
- Lucchesi B. R., Mullane K. M. Leukocytes and ischemia-induced myocardial injury. Annu Rev Pharmacol Toxicol. 1986;26:201–224. doi: 10.1146/annurev.pa.26.040186.001221. [DOI] [PubMed] [Google Scholar]
- Williams T. J., Jose P. J., Forrest M. J., Wedmore C. V., Clough G. F. Interactions between neutrophils and microvascular endothelial cells leading to cell emigration and plasma protein leakage. Kroc Found Ser. 1984;16:195–208. [PubMed] [Google Scholar]


