Abstract
Study Objectives:
To assess the impact of a daytime sleep medical procedure—the PAP-NAP—on adherence to positive airway pressure (PAP) therapy among insomnia patients with sleep disordered breathing (SDB)
Methods:
The PAP-NAP is based on Current Procedural Terminology (CPT) codes and combines psychological and physiological treatments into one procedure, which increases contact time between SDB patients and polysomnography technologists to enhance PAP therapy adherence. Using a Sleep Dynamic Therapy framework, explicating SDB as a mind-body disorder, the PAP-NAP includes mask and pressure desensitization, emotion-focused therapy to overcome aversive emotional reactions, mental imagery to divert patient attention from mask or pressure sensations, and physiological exposure to PAP therapy during a 100-minute nap period. Patients treated with the PAP-NAP test (n=39) were compared to an historical control group (n=60) of insomnia patients with SDB who did not receive the test.
Results:
All 99 insomnia patients were diagnosed with SDB (mean AHI 26.5 ± 26.3, mean RDI 49.0 ± 24.9), and all reported a history of psychiatric disorders or symptoms as well as resistance to PAP therapy. Among 39 patients completing the PAP-NAP, 90% completed overnight titrations, compared with 63% in the historical control group; 85% of the nap-tested group filled PAP therapy prescriptions for home use compared with 35% of controls; and 67% of the nap-tested group maintained regular use of PAP therapy compared with 23% of the control group. Using standards from the field of sleep medicine, the nap-tested group demonstrated objective adherence of 49% to 56% compared to 12% to 17% among controls. All studies were reimbursed using CPT 95807–52.
Conclusion:
In this pilot study, the PAP-NAP functioned as a brief, useful, reimbursable procedure to encourage adherence in insomnia patients with SDB in comparison to an historical control group that did not undergo the procedure.
Citation:
Krakow B; Ulibarri V; Melendrez D; Kikta S; Togami L; Haynes P. A daytime, abbreviated cardio-respiratory sleep study (CPT 95807–52) to acclimate insomnia patients with sleep disordered breathing to positive airway pressure (PAP-NAP). J Clin Sleep Med 2008;4(3):212-222.
Keywords: positive airway pressure therapy, adherence, CPT, sleep breathing
Research on adherence to positive airway pressure (PAP) therapy machines (e.g. CPAP, bilevel) for the treatment of sleep disordered breathing (SDB) consistently demonstrates “more is better.”1 More hands-on or group education,2–4 clinical follow-up,5 sleep technologist/technician coaching,6 telephone calls,7 objective data monitoring,8 and repeat polysomnography (PSG)1 all serve useful purposes in engaging sleep disordered breathing patients to maintain regular use of PAP therapy devices.
According to Haynes,6 these encounters are delivered with the greatest efficacy by behavioral sleep medicine (BSM) specialists, generally a group of physicians and psychologists with specialized training in cognitive-behavioral therapies directed at sleep problems. In addition, many sleep technologists (registered) and technicians (nonregistered) routinely provide services to patients during PSG tests or in “CPAP clinics.” These clinics are supervised usually by a physician or psychologist (nurses, nurse practitioners, and physician assistants may also participate),9 and sleep techs coach patients through a series of adjustments to find more comfortable masks to tolerate PAP, and to sort out complaints arising from this unusual form of physiological treatment.6
Unfortunately, BSM specialists are in short supply, and no Evaluation & Management CPT codes exist to reimburse sleep centers or sleep labs for the time spent by sleep techs to coach patients at CPAP clinics.10 In our discussions with other sleep medicine colleagues, we sense two important issues affect CPAP clinics: (1) many sleep centers or labs operate CPAP clinics without receiving any reimbursement; (2) resource use in these clinics varies based on the need to balance available time to enhance patient care with the lack of reimbursement.
In our patient population at Maimonides Sleep Arts & Sciences, Ltd. and in our collaboration with the Los Alamos Medical Center Sleep Laboratory, we specialize in the treatment of patients with the combination of mental health disorders, comorbid insomnia, and SDB.11 Although the literature on barriers to PAP therapy use among more complex SDB patients shows mixed findings,6,12–17 we note that these patients require extensive encounters to learn to tolerate PAP therapy devices. In particular, comorbid conditions such as insomnia, nightmares, anxiety, depression, posttraumatic stress disorder, panic attacks, and claustrophobia may interfere with the adaptation process and prevent long-term adherence to PAP therapy.6,14–18
In 2004, we expressed concerns about these complex patients to regional Medicare officials in order to develop more efficient treatment strategies. As these patients require repeated clinical encounters and extensive sleep tech coaching time, we raised questions about how such encounters might be more efficiently organized as a reimbursable procedure. The resulting discussions led us to develop a daytime procedure, combining hands-on coaching (delivered by sleep techs under the supervision of a physician) with the physiological experience of positive airway pressure therapy, which we call the PAP-NAP.
The current report describes the PAP-NAP, which utilizes existing CPT codes (CPT 95807–52; the modifier indicating a shorter study period) for reimbursement. The CPT 95807 procedure has previously been described as a tool to enhance PAP therapy compliance.19 The PAP-NAP was developed during a 6-month period and tested another 18 months in conjunction with discussions with Medicare staff and medical directors. This report describes the first 39 patients completing PAP-NAPs, all of whom suffered from insomnia, psychiatric disorders or symptoms, and SDB, who also manifested resistance to PAP therapy. We compared their results with a group of historical controls, who showed similar characteristics to our treated sample and who were drawn from our pool of patients from both centers prior to the inception of the PAP-NAP procedure.
We hypothesized the procedure would produce 5 outcomes:
The vast majority of those completing the PAP-NAP compared to the historical control group would gain sufficient confidence to complete a subsequent titration study.
Between the two groups, a larger proportion of PAP-NAP participants than controls would agree to fill their prescription for PAP therapy and attempt home use of the device.
The PAP-NAP group would demonstrate a much larger proportion of patients than controls regularly using PAP therapy.
Adherence (as defined per standards in the field1,20–22) to PAP therapy would equal or exceed 50% of those tested in the PAP-NAP group, compared with a much lower proportion of patients in the control group.
The PAP-NAP, utilizing CPT code 95807–52 as an abbreviated study, would be a reimbursable procedure.
METHODS
Consent
Per standard protocol at the two sleep facilities, all patients provide written and verbal consent for their medical information to be used anonymously for research purposes in the context of subsequent chart reviews. All patients from the two sleep centers completed their PAP-NAPs at the Maimonides sleep center in Albuquerque, NM. This study was a retrospective chart review of existing data. The study was reviewed and approved by the Los Alamos Medical Center IRB.
Treatment Group
Our initial efforts focused on mental health patients with insomnia and SDB who manifested obvious resistance to using PAP therapy. These patients had been referred by psychiatrists or primary care physicians for unspecified insomnia conditions, insomnia due to a mental disorder, or hypnotic dependence. In our experience, most of these patients show signs and symptoms suggestive of SDB.23–26 After intake, patients receive sleep hygiene and cognitive-behavioral instructions in book format27 to initiate insomnia treatment. Nearly all express strong skepticism about the possibility of a sleep breathing condition influencing their sleep, or they express anxiety or fear about PAP therapy. Some never agree to complete diagnostic polysomnography. Among those who completed PSG and were subsequently diagnosed with UARS or OSA, the concept of the titration procedure was discussed to determine receptivity and motivation to proceed. Among those expressing resistance towards the SDB diagnosis in general or PAP therapy in particular, the PAP-NAP procedure is offered as an alternate option to be conducted prior to (not in place of) a full night PAP therapy titration.
All patients completed an intake set of questionnaires, including an extensive sleep medicine history as well as the validated scale Insomnia Severity Index (ISI).28 Responses on the intake and ISI were reviewed initially by the sleep specialist to determine patient appropriateness for diagnostic polysomnography. After diagnostic testing and establishing an SDB diagnosis (based on AASM criteria29), the patient was contacted by telephone or in person to discuss the potential value of a titration. On a case-by-case basis, the physician or his supervised assistant discussed the risks and benefits of the titration; among those who showed some degree of resistance to moving forward, the PAP-NAP was offered instead. Indeed, in every case, patients who chose the PAP-NAP could not be persuaded to complete a full-night titration or split-night protocol.
Historical Control Group
To develop a comparable historical group of control patients with insomnia, mental health conditions, and SDB, who also showed resistance or skepticism to PAP therapy, we started by reviewing charts on all patients who were seen at either sleep center between June of 2003 and June 2004 (n = 291), that is, before the inception of the PAP-NAP procedure. These patients had completed the same questionnaires described above, and their data had already been stored in our patient database. This data resource permitted us to review their information blindly without looking at actual patient charts. By doing so, the reviewer (second author) was blinded from any knowledge of type or number of studies performed on each patient and whether these patients were ever prescribed or currently using PAP therapy. The reviewer used the following sequence of five steps to develop the control group:
(Step 1) Insomnia Problems. The patients had to score higher than 11 on the Insomnia Severity Index,28 the original validation cut-off for clinically meaningful insomnia. Of 291 patients seen in the year prior to the PAP-NAP procedure, 179 patients scored 12 or greater.
(Step 2) Psychiatric Disorders/Symptoms. To be included, patients indicated the presence of current or past history of mental health disorders and/or psychotropic medication usage, or a history of other psychiatric symptoms (e.g., claustrophobia, nightmares, history of trauma) or specific anxiety about PAP therapy. Forty-nine patients were excluded, leaving 130 patients as potential controls.
(Step 3) SDB Awareness. Responses on the intake were then reviewed to assess awareness of potential sleep breathing problems, because we have observed greater awareness in those who are motivated to seek treatment and lesser awareness in those with more skepticism about SDB. Patients who acknowledged a sleep breathing problem or saw SDB as the main cause of their sleep problems were eliminated. Forty-five additional patients were excluded, leaving 85 potential controls.
(Step 4) PAP Therapy Perspectives. Finally, patient responses to a question about PAP therapy were reviewed, and those who expressed favorable views of breathing mask treatments were excluded, which removed another 20 patients, leaving a potential control group of 65 patients.
(Step 5) Then, for the first time, we looked at medical records and when available diagnostic polysomnography data, interpretations, and recommendations in these 65 patients. Four patients were eliminated who had refused diagnostic testing, and one patient was excluded whose diagnostic PSG did not show SDB. The final sample involved these 60 patients.
Procedure
Diagnostic studies were performed on all 99 (treated n = 39; control n = 60) patients using standard polysomnography, performed in the Los Alamos Medical Center Sleep Lab or at Maimonides Sleep Arts & Sciences. Technicians prepared the patients using the International 10–20 System of Electrode Placement. The recording had a 14-channel montage: left outer canthus-A2; right outer canthus-A1; C3-A2; C4-A1; O1-A2; O2-A1; chin; ECG; left leg-right leg; snore; nasal pressure transducer via nasal cannula; chest effort; abdominal effort; pulse oximetry; and position. Sleep was scored manually according to Rechtschaffen and Kales.30 Three types of breathing events were scored. An apnea was a greater than 70% decrease in airflow for ≥ 10 sec. Hypopnea was 30% to 70% decrease in airflow coupled with either a 4% oxygen desaturation or an arousal. Flow limitation was a decrease in airflow of ≤ 30% in the form of classic flattening or notching of the airflow limb for at least 2 consecutive breaths, ending in an arousal. Minimum oxygen saturation (minSaO2) was recorded by pulse oximetry.
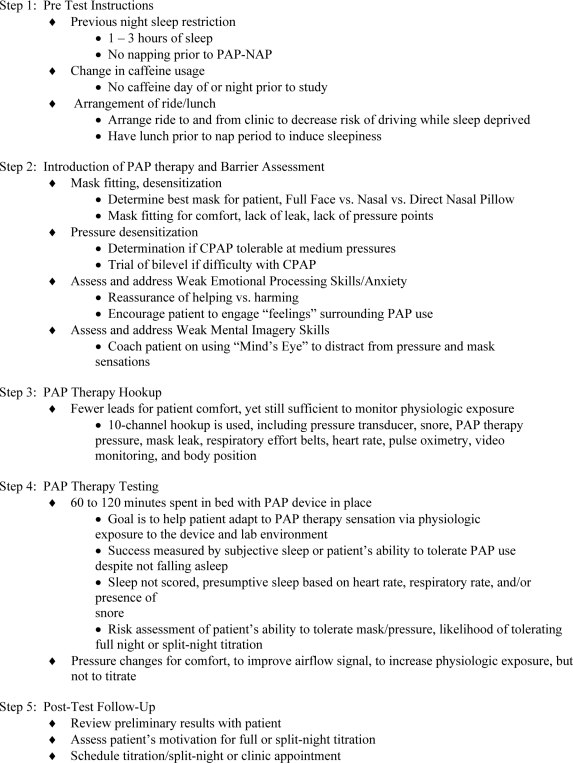
The PAP-NAP involves 5 components, which are summarized in Figure 1; key elements are discussed below:
Figure 1.
PAP-Nap Procedure
Pretest instructions on how to prepare for the study to maximize chances for napping during the day in the sleep lab. Steps include previous night sleep restriction, change in caffeine use, finding a ride to the sleep center to avoid driving, and eating (if soporific) prior to the test.
-
Introduction of PAP therapy and barrier assessment to provide patient with physical exposure to masks and pressurized airflow, including mask fittings and testing the feel of pressure with mask in place. These exposures are designed as a hierarchical desensitization. Throughout the procedure, the patient receives coaching in areas perceived by the sleep tech as likely to interfere with adaptation to the breathing mask. Beyond the physical barriers, 2 additional areas are addressed, involving deficits in emotional processing skills or mental imagery skills, previously described in our work with insomnia patients under the rubric “Sleep Dynamic Therapy.”31
Weak emotional processing skills generally manifest in the form of an inability to articulate the precise nature of complaints about the breathing mask. SDB patients may state they don't like the idea of PAP therapy or it feels odd, but often 6 common emotional processes underlie these impressions, including: anxiety, fear, discomfort, pain, embarrassment, or shame.26 The patient learns that “talking” about PAP therapy complaints may be one step removed from the actual “feeling” of an emotion that might be the real barrier. Instead, if the patient articulates or experiences some emotion about the process, it may release stressful feelings. Usually, the patient recognizes whether the emotion is a major barrier needing ongoing efforts to resolve (e.g., embarrassment about spouse's reaction to the mask; fear that sex life will be ruined, or shame about needing a machine to sleep) or whether simple recognition of the emotion starts defusing it.26 The discussion is straightforward, easily conducted by the sleep tech, and only rarely leads to increased anxiety. Moreover, because the PAP-NAP is conducted during regular work hours, the sleep specialist at our center is immediately available to address unexpected reactions or more intense issues that may arise.
Suppressed mental imagery skills are nearly omnipresent among our insomnia patients with racing thoughts or ruminations, because they tend to use “thinking” as a defense against “feeling” or “picturing” things in the mind's eye.26 This overly analytic or intellectualizing style not only interferes with sleep onset, but eventually, ruminations often turn toward the mask or pressure sensations. The patient is coached on the human capacity to engage the mind's eye to picture pleasant scenes from past, present, or anticipated events. Mental imagery is something within their control and which proves to be a superior way to decrease racing thoughts or ruminations.26 Once mental imagery skills are strengthened, the SDB patient uses them as a diversion to turn attention away from the mask and pressure sensations. Most patients are coached by the sleep tech to perform imagery exercises during a 15-min period, and then the technique is applied in the next phase of the PAP-NAP. For more severe cases such as trauma survivors with nightmares, the sleep specialist is available to meet the patient to determine whether they are capable of proceeding with imagery exercises.
PAP Therapy Hookup is designed specifically for patients who reported prior difficulties in the lab environment during a diagnostic study or who anticipate such difficulties based on preconceived notions of the process. As EEG leads on the scalp and eyes are common sources of complaints in our experience, the PAP-NAP avoids these contact points. Instead, as implied in the 1997 guidelines of the American Academy of Sleep Medicine,19 leads are less intrusive and are designed to help the patient feel more comfortable while at the same time providing the sleep tech with sufficient monitoring tools to enhance the physiological exposure of PAP therapy during the nap period. A 10-channel hookup is used, including airflow pressure transducer, snore, PAP therapy pressure, mask leak, respiratory effort belts, heart rate, pulse oximetry, video monitoring, and body position.
-
PAP Therapy Testing is conducted during a 60- to 120-min interval in bed. The primary goal is to help the patient use PAP therapy for more than one hour, during which he or she has the potential to fall asleep with the mask in place or to at least report that the experience was not uncomfortable. Success is measured by either those patients who reported they slept with the mask or who reported the ability to tolerate the mask or pressure regardless of whether they slept, and thus perceived themselves capable of attempting the full-night titration test. Although monitoring of sleep might be ideal, the PAP-NAP is not a titration but instead provides the patient with physiologic exposure to PAP therapy as well as to the lab environment. It does not provide definitive sleep or breathing evaluations. The sensors for the PAP-NAP are utilized as follows:
Airflow pressure transducer identifies presumptive breathing events observed on the airflow channel including hypopneas, apneas, flow limitation as well as pressure intolerance, warranting pressure adjustment to normalize breathing and facilitate pressure adaptation;
Snore microphone assists in identifying presumptive sleep and breathing types;
PAP pressure adjustments promote desensitization, enhance patient comfort, and respond to presumptive breathing events;
Pressure leak assesses proper mask fit and possible mouth leak, requiring mask adjustment, application of chinstrap, or mask replacement;
Respiratory effort belts identify presumptive breathing events in conjunction with the pressure transducer;
Pulse oximeter measures oxyhemoglobin saturation and heart rate to identify presumptive sleep, breathing events, and response to PAP therapy, as adjustments are made to stabilize the oxygen baseline;
Video monitoring provides visual assessment of position and comfort by monitoring patient movement, which may indicate need for adjustments to mask or pressure;
Body position monitoring allows for the identification of position-dependent breathing events;
Presumptive sleep is assumed but not validated by the emergence of snoring or other presumptive breathing events or through the steady reductions in heart rate or in oxygen baseline.32 Although monitoring of sleep might prove useful, the purpose of the PAP-NAP is to expose and acclimate not titrate the patient to PAP therapy.
Post-Test Follow-up discussion with patient to review preliminary study impressions and determine patient motivation to pursue next treatment steps, after which patients were either scheduled for their titration test or scheduled in clinic to review issues that prevented scheduling for a titration test. No predetermined methods for measuring adherence were developed for this protocol. In the results section, we report methods published in the literature, and we used these metrics to measure adherence in our sample.1,20–22
Billing Codes
The procedure meets criteria for sleep study CPT code 95807 in that it includes 4 or more sensors, including “simultaneous recording of ventilation, respiratory effort, ECG or heart rate, and oxygen saturation, attended by a technologist.”10 The average procedure length ranges between 2 to 5 h, with time usually dependent upon the degree of desensitization and coaching needed for masks and pressure sensations, efforts to overcome emotional or imagery barriers, and actual recording time. Rare procedures are as short as 1.5 h or as long as 6 h. The average for this sample was slightly under 3.5 h. Nonetheless, following our discussions with Medicare officials, we agreed that Modifier 52 for abbreviated studies should be used, so that final billing was entered as CPT 95807–52.10 We labeled the procedure: Abbreviated Cardio-Respiratory Nap Study for billing purposes so that the terms matched the CPT code.10 In the sleep center environment, we refer to the procedure as the PAP-NAP.
RESULTS
Data Analysis
ANOVA and Chi-Square analyses were performed for continuous and dichotomous variables. Cohen's d effect sizes, the standardized mean difference, were calculated from the difference in 2 means, divided by the pooled standard deviation. Statistical significance was 0.05.
Pertinent Clinical Background
Tables 1 and 2 describe pertinent sociodemographic and clinical backgrounds about the 2 patient groups, tested (n = 39) and historical controls (n = 60). Both groups were middle-aged with the nap-tested group slightly older (51.13 [14.97] vs. 43.65 [13.57]; p = 0.01) and slightly more overweight per body mass index (29.84 [7.54] vs. 26.63 [5.37]; p = 0.02). Both groups were predominantly Caucasian with the nap-tested group having a slightly higher percentage of Caucasians than the control group (82% vs. 72%, p = 0.03). All patients demonstrated a clinically meaningful degree of insomnia on the Insomnia Severity Index with no difference between groups (17.5 [5.2] for nap-tested; 16.7 [4.1] for controls). Further indications of greater complexity to their sleep disorders were the presence of hypnotic dependence among 36% of the nap-tested group and 25% of control group. Regular use of OTC sleep aids was seen by another 8% in the nap-tested group and 20% in the control group. The majority of both groups had some history of psychiatric disorders (54% nap-tested vs. 73% control, p = 0.04). Claustrophobia was seen in 46% of the nap-tested group, but only in 20% of the control group (p = 0.01). Overall, these patients fit into the model previously described as “complex insomnia,” which involves both insomnia and sleep breathing problems of moderate to severe intensity, frequently associated with mental health symptoms likely to exacerbate sleep complaints.33
Table 1.
Sociodemographics Data§
| Characteristic | NAP Tested (n = 39) | Control (n = 60) | Total (n = 99) | p value‡ |
|---|---|---|---|---|
| Age, y | 51.13 ± 14.97 | 43.65 ± 13.57 | 46.6 ± 14.53 | 0.01 |
| Sex | ||||
| Male | 20 (51) | 25 (42) | 45 (45) | |
| Female | 19 (49) | 35 (58) | 54 (55) | 0.23 |
| Body Mass Index, kg/m2 | 29.84 ± 7.54 | 26.63 ± 5.37 | 27.89 ± 6.48 | 0.02 |
| Marital Status | ||||
| Married, Living w/partner | 23 (59) | 31 (52) | 54 (55) | |
| Single, Divorced, or other | 16 (41) | 29 (48) | 45 (45) | 0.31 |
| Education | ||||
| Some college or lower | 20 (51) | 27 (45) | 47 (47) | |
| Bachelors degree or higher | 19 (49) | 33 (55) | 52 (53) | 0.34 |
| Ethnicity∞ | ||||
| Hispanic | 5 (13) | 9 (15) | 14 (14) | |
| Caucasian | 32 (82) | 43 (72) | 75 (76) | |
| Other | 2 (5) | 8 (13) | 10 (10) | 0.03 |
Dichotomous variables expressed as n (% of total) and continuous variables expressed as mean ± SD.
p value determined using χ2 analysis for dichotomous variables and One-Way ANOVA for continuous variables.
p value determined using χ2 analysis of men/women by Anglo/Hispanic. Ten patients excluded.
Table 2.
Insomnia Severity and Related Sleep Medical and Psychiatric History§
| Characteristic | NAP Tested (n = 39) | Control (n = 60) | Total (n = 99) | p value‡ |
|---|---|---|---|---|
| Insomnia Severity Index | 17.51 ± 5.17 | 16.68 ± 4.14 | 17.01 ± 4.57 | 0.38 |
| Psychiatric Disorders | ||||
| Yes | 21 (54) | 44 (73) | 65 (66) | |
| No | 18 (46) | 16 (27) | 34 (34) | 0.04 |
| Claustrophobia History | ||||
| Yes | 18 (46) | 12 (20) | 30 (30) | |
| No | 21 (54) | 48 (80) | 69 (70) | 0.01 |
| Trauma History | ||||
| Yes | 12 (31) | 22 (37) | 34 (34) | |
| No | 27 (69) | 38 (63) | 65 (66) | 0.35 |
| Nightmare History | ||||
| Yes | 15 (38) | 30 (50) | 45 (45) | |
| No | 24 (62) | 30 (50) | 54 (55) | 0.18 |
| Avg. Number of Traumas | 4.67 ± 18.16 | 1.46 ± 2.89 | 3.40 ± 14.29 | 0.28 |
| Snore | ||||
| Yes | 31 (79) | 39 (65) | 70 (71) | |
| No | 8 (21) | 21 (35) | 29 (29) | 0.09 |
| Stop Breathing | ||||
| Yes | 15 (38) | 11 (18) | 26 (26) | |
| No | 24 (62) | 49 (82) | 73 (74) | 0.02 |
| Sleepy VAS | 6.08 ± 2.36 | 6.23 ± 2.21 | 6.17 ± 2.25 | 0.74 |
| Tired VAS | 7.03 ± 2.40 | 6.93 ± 2.09 | 6.97 ± 2.21 | 0.84 |
| Hypnotic Dependent | ||||
| Yes | 14 (36) | 15 (25) | 29 (29) | |
| No | 25 (64) | 45 (75) | 70 (71) | 0.17 |
| OTC Sleep Aid Dependent | ||||
| Yes | 3 (8) | 12 (20) | 15 (15) | |
| No | 36 (92) | 48 (80) | 84 (85) | 0.08 |
| Napping Habits | ||||
| Every other day or more | 11 (28) | 15 (25) | 26 (26) | |
| Less than every other day | 28 (72) | 45 (75) | 73 (74) | 0.45 |
| Caffeine Use | ||||
| Once a day or more | 13 (33) | 23 (38) | 36 (36) | |
| Less than once a day | 26 (67) | 37 (62) | 63 (64) | 0.39 |
Dichotomous variables expressed as n (% of total) and continuous variables expressed as mean ± SD.
p value determined using χ2 analysis for dichotomous variables and One-Way ANOVA for continuous variables.
Prescription and OTC sleep aid dependence based on subjective report of regular, multiple night use per week.
Objective Diagnostic PSG Data
Table 3 confirmed objectively the insomnia problems in these patients as their PSG indices demonstrated moderate to severe sleep maintenance insomnia (∼1 h), decreased total sleep time (∼6 h) and poor sleep efficiency (∼80%). The apnea-hypopnea index in these 2 groups was essentially identical with an average of 25.5 (29.8) events/h in the nap-tested group vs. 27.1 (25.0) in the controls; average RDI was comparable in both groups (49.3 [27.34] vs. 49.2 [23.5]). When comparing percentage of total sleep time spent below SpO2 of 90%, there was a trend towards greater severity in the nap-tested group vs. the control group (24.1% [28.6] vs. 14.3% [26.8]; p = 0.09).
Table 3.
Diagnostic PSG Data§
| Variable | NAP Tested (n = 39) | Control (n = 60) | Total (n = 99) | p value‡ |
|---|---|---|---|---|
| Total Sleep Time, min | 338.59 ± 126.99 | 365.02 ± 119.52 | 354.60 ± 122.57 | 0.30 |
| Wake after Sleep Onset, min* | 69.33 ± 52.05 | 55.78 ± 46.97 | 60.95 ± 49.15 | 0.19 |
| Sleep Efficiency, % | 77.68 ± 16.65 | 82.48 ± 12.91 | 80.59 ± 14.61 | 0.11 |
| AHI, events/h | 25.50 ± 29.80 | 27.16 ± 24.95 | 26.50 ± 26.33 | 0.77 |
| RDI, events/h | 49.28 ± 27.34 | 48.85 ± 23.44 | 49.01 ± 24.88 | 0.93 |
| % Study Time SpO2 < 90%* | 24.12 ± 28.58 | 14.31 ± 26.78 | 18.05 ± 27.78 | 0.09 |
Continuous variables expressed as mean ± SD.
p value determined using One-Way ANOVA.
Based on n of 38 (diagnostic PSG done at other sleep lab with no report of WASO)
TST (Total Sleep Time), duration of rapid eye movement (REM) sleep plus non-REM sleep epochs from lights off to lights on; WASO (Wake After Sleep Onset), number of wake epochs from lights off to lights-on; Sleep Efficiency, total time from persistent sleep onset to the end of the polysomnogram divided by time in bed multiplied by 100; AHI (Apnea-Hypopnea Index), number of apneas and hypopneas per hour of sleep time; RDI (Respiratory Disturbance Index), AHI plus flow limitation events per hour of sleep time.
PAP-NAP Testing Results
Table 4 summarizes the experiences of the patients who completed the PAP-NAP test. Over the nose or nasal pillow interfaces were the preferred masks for most patients. Recording time averaged just under 100 min during the actual nap portion of the procedure. Based on sleep tech impressions, three-quarters of patients fell asleep during the PAP-NAP, but only one-third of patients actually believed they slept. The pressure range used during the studies was fairly low and narrow, averaging 6 to 9 cm H2O (CPAP or IPAP on bilevel). Men greatly preferred bilevel over CPAP (85% vs. 15%), whereas a small majority of women preferred bilevel over CPAP (53% vs. 47%), which was statistically significant (p = 0.03). The most commonly stated reason for bilevel preference was greater ease of breathing on exhalation. Both mask discomfort and PAP discomfort were commonly reported, but not a single patient prematurely terminated the PAP-NAP procedure.
Table 4.
PAP-NAP Data§
| Variable | Men (n = 20) | Women (n = 19) | Total (n = 39) | p value‡ |
|---|---|---|---|---|
| Mask Used‡‡ | ||||
| Nasal (over the nose) | 11 (55) | 12 (63) | 23 (59) | |
| Nasal (pillow) | 5 (25) | 5 (26) | 10 (26) | |
| Full Face | 4 (20) | 2 (11) | 6 (15) | 0.71 |
| PAP Exposure Time, min | 90.4 ± 30.84 | 106.03 ± 35.38 | 98.04 ± 32.93 | 0.14 |
| Sleep Achieved§§ | ||||
| Self Reported | 7 (35) | 6 (32) | 13 (33) | |
| Tech Reported | 15 (75) | 14 (74) | 29 (74) | |
| Indeterminate | 2 (10) | 3 (16) | 5 (13) | 0.62 |
| Maximum CPAP or bilevel IPAP Pressure Achieved | ||||
| PAP-NAP Starting Pressure, cm H2O | 6.50 ± 2.54 | 5.76 ± 1.62 | 6.14 ± 2.15 | 0.29 |
| Highest Pressure, cm H2O | 9.48 ± 2.94 | 8.42 ± 2.85 | 8.96 ± 2.91 | 0.26 |
| PAP Therapy Mode Preferred | ||||
| CPAP | 3 (15) | 9 (47) | 12 (31) | |
| Bilevel | 17 (85) | 10 (53) | 27 (69) | 0.03 |
| Patient Discomfort*Φ | ||||
| Mask | 2 (10) | 7 (37) | 9 (23) | |
| Pressure | 9 (45) | 5 (26) | 14 (36) | |
| Other (anxiety, claustrophobia, etc.), n (%) | 5 (25) | 6 (32) | 11 (28) | |
| No Discomfort | 8 (40) | 8 (42) | 16 (41) | 0.53 |
Dichotomous variables expressed as n (% of total) and continuous variables expressed as mean ± SD.
p value determined using χ2 analysis for dichotomous variables and One-Way ANOVA for continuous variables.
p value determined using χ2analysis of men/women by nasal interface mask/full face mask.
p value determined using χ2 analysis of men/women by self reported sleep/tech reported sleep with the exclusion of 5 indeterminate patients
Note: Some patients experienced more than one form of discomfort during PAP-NAP.
p value determined using χ2 analysis of men/women by presence of any discomfort/no discomfort.
Post PAP-NAP Follow-up
Titration Data
Table 5 compares the post PAP-NAP titration data for the 90% (n = 35) of the 39 nap-tested patients and 63% (n = 38) of the control patients who subsequently scheduled and completed an overnight titration or split-night with full sensor hookups (p = 0.003). Among those completing titrations, the apnea hypopnea index and the RDI were reduced in both groups, and no differences were noted between groups. In the nap-tested group, diagnostic AHI decreased from 25.9 (31.1) events/h to 2.0 (3.1); whereas, in controls, diagnostic AHI decreased from 33.5 (26.8) events/h to 15.3 (17.0) events/h (p = 0.35). For RDI, the nap-tested group decreased from 48.5 (27.7) events/hour to 25.6 (20.3) compared to the control group, which decreased from 54.5 (24.6) events/h to 31.8 (16.1) (p = 0.78).
Table 5.
| Variable | NAP Tested (n = 35) | Control (n = 38) | Total (n = 73) | p value‡ |
|---|---|---|---|---|
| Total Sleep Time, min | 326.05 ± 108.44 | 338.04 ± 108.22 | 332.29 ± 107.74 | 0.64 |
| Sleep Efficiency | 76.46 ± 18.12 | 74.91 ± 14.94 | 75.65 ± 16.44 | 0.69 |
| Wake after Sleep Onset, min | 84.00 ± 62.81 | 90.10 ± 57.15 | 87.18 ± 59.59 | 0.67 |
| AHI, events/h | 2.00 ± 3.18 | 15.26 ± 16.96 | 9.00 ± 14.11 | 0.00 |
| RDI, events/h | 25.62 ± 20.25 | 31.77 ± 16.05 | 28.87 ± 18.29 | 0.16 |
Continuous variables expressed as mean ± SD.
Based on n of 35 for nap-tested group and n of 38 for control group who completed a full night titration.
p value determined using One-Way ANOVA for continuous variables.
TST (Total Sleep Time), duration of rapid eye movement (REM) sleep plus non-REM sleep epochs from lights off to lights on; WASO (Wake After Sleep Onset), number of wake epochs from lights off to lights-on; Sleep Efficiency, total time from persistent sleep onset to the end of the polysomnogram divided by time in bed multiplied by 100; AHI (Apnea-Hypopnea Index), number of apneas and hypopneas per hour of sleep time; RDI (Respiratory Disturbance Index), AHI plus flow limitation events per hour of sleep time.
PAP Therapy Usage
Table 6 summarizes current use and adherence data for the 2 groups. Of the 39 patients in the nap-tested group, 85% (n = 33) filled their prescription for PAP therapy, obtained a device, and attempted home use. Of these 39 patients, 26 or 67% maintained regular use of the device. Women appeared to maintain use of PAP therapy more so than men (74% vs. 57%), but this finding was not significant (p = 0.22). In the control group of 60 patients, only 35% (n = 21) ever filled a prescription for a machine, and only 14 (23%) were regular users of PAP therapy.
Table 6.
Current Use And Adherence Data§
| Variable | NAP Tested (n = 39) | Control (n = 60) | Total (n = 99) | p value‡ |
|---|---|---|---|---|
| Current Regular PAP Therapy Useϕ | ||||
| Yes | 26 (67) | 14 (23) | 40 (40) | |
| No | 13 (33) | 46 (77) | 59 (60) | 0.00 |
| Monthly PAP Therapy Use, %∞‡‡ | 84.66 ± 12.78 | 76.67 ± 23.13 | 82.13 ± 16.84 | 0.18 |
| Hours/Night PAP Use Based Only on Nights Used in the Month∞ | 6.22 ± 1.37 | 5.78 ± 1.82 | 6.08 ± 1.51 | 0.42 |
| Hours/Night PAP Use Based on All Nights in the Month∞ | 5.24 ± 1.74 | 4.46 ± 2.71 | 5.00 ± 2.09 | 0.29 |
| Adherence based on CPAP use of ≥5d/wk and ≥ 4h/d avg. on days used∞** | ||||
| Yes | 22 (56) | 10 (17) | 32 (32) | |
| No | 17 (44) | 50 (83) | 67 (68) | 0.00 |
| Adherence based on CPAP use of ≥ 5d/wk and ≥ 4h/d avg. for all days including days not used∞⧣ | ||||
| Yes | 19 (49) | 7 (12) | 26 (26) | |
| No | 20 (51) | 53 (88) | 73 (74) | 0.00 |
Dichotomous variables expressed as n (% of total) and continuous variables expressed as mean ± SD.
p value determined using χ2 analysis for dichotomous variables and One-Way ANOVA for continuous variables.
Obtained from individual PAP machine data downloads (n = 26 for NAP tested group and n = 14 for control group).
% based on number of nights of actual use in potential 30 day period.
Based on study by Kribbs et al.(20)
Based on study by Pepin et al.(22)
Objective Data and Adherence
To measure time spent using treatment among regular users, we obtained objective data downloads from patients' PAP devices (nap-tested, n = 26; controls, n = 14). Data downloads among the nap-tested group showed that PAP therapy was used an average of 84.7% of nights/month compared to the control group, which averaged 76.7% of nights/month. On nights actually used, the nap-tested group averaged 6.2 (1.4) h compared to 5.7 (1.8) h in controls (p = 0.42). Overall usage for the month averaged 5.2 (1.7) h/night in the nap-tested group in contrast to the control group, which averaged 4.5 (2.7) h/night (p = 0.29).
To assess overall adherence, we started with gold standard adherence, defined by Weaver1 as “every night, all night,” which revealed adherence of only 10% (4 of 39) in our nap-tested vs. 3% (2 of 60) in controls (p = 0.16). A more liberal metric by McArdle et al.21 defines adherence as a mean PAP therapy use of >2 h/night, yielding 67% adherence in our nap-tested sample and 23% in our control group (p = 0.00). In the middle of this spectrum, Kribbs et al.20 define adherence as PAP therapy for ≥5 days/week and an average of ≥4 h/day, restricted to only those days used, yielding 56% adherence in our sample compared to 17% in controls (p = 0.00). Finally, Pepin et al.22 use the identical model of Kribbs et al. (5 nights, 4 h), but average hourly use is calculated more stringently with a denominator consisting of all days for the time interval studied, whether PAP therapy was used or not on any given day. Our nap-tested group showed adherence equaled 49% on this last model compared to 12% in controls (p = 0.00).
Hypothesis Testing Summary
In terms of our hypotheses, the nap-tested group fared better than the controls in those completing titrations (90% vs. 63%, p = 0.003), those filling scripts (85% vs. 35%; p = 0.00), and those meeting criteria for averaged adherence between Kribbs' and Pepin's guidelines (53% vs. 15%) based on objective data. Based on subjective data, the nap-tested group fared better than controls in those regularly using PAP therapy (67% vs. 23%, p = 0.00). Even when comparing only those patients who completed a titration (35 nap-tested patients and 38 controls), the nap-tested group filled prescriptions in greater numbers (86% vs. 55%, p = 0.004), were more regular users (67% vs. 37%, p = 0.001), and once again based on averaged adherence rates using Kribbs and Pepin guidelines, were more adherent (59% vs. 20%, p = 0.001).
Additional analyses revealed a few distinguishing findings between users and non-users of PAP therapy across groups. There was a higher mean post-titration AHI value (12.0 ± 15.0) among non-users compared to users (4.9 ± 11.7), which was statistically significant (p = 0.03, d = 0.48). Sleep efficiency decreased in both groups during titrations; however, there was a trend (p = 0.07, d = 0.34) toward greater decrease in sleep efficiency in the non-user group (8.6% decrease) compared to the user group (1.6% decrease). When comparing current users to individuals who are nonadherent, a history of psychiatric disorders was associated with a decreased likelihood of PAP adherence (25% adherent with positive psychiatric history vs. 75% adherent without psychiatric history, p = 0.02). Likewise, individuals with a history of trauma were less PAP adherent (15% adherent with positive trauma history vs. 85% adherent with negative trauma history, p = 0.04). Finally, in current users vs. non-users there was a trend towards higher BMI (29.39 [7.16] vs 26.87 [5.81], p = 0.06) and older age (49.90 [17.39] vs. 44.36 [11.87], p = 0.06). A series of follow-up logistic regression analyses revealed no changes in any of the statistically significant PAP therapy adherence outcomes when group differences at baseline were separately entered as a covariate into each of the regression models.
To test our last hypothesis, all procedures were reimbursed using CPT 95807–52.
DISCUSSION
The PAP-NAP appeared to be a useful procedure to facilitate interest in PAP therapy in complex insomnia patients likely to fear or dismiss this unusual physiological form of treatment. In the first 39 patients tested with the PAP-NAP procedure, the majority expressed positive experiences, and 90% completed either a full-night titration or a split-night diagnostic/titration after the PAP-NAP. In this population of patients who would be expected to be resistant to PAP therapy and suffer low compliance rates, 67% of those undergoing a PAP-NAP are currently using the breathing mask treatment with some regularity, compared with 23% of the historical control group. Adherence rates were also higher for the nap-tested group (49%22 to 56%20) versus the control group (12%22 to 17%20) based on commonly used standards. Given the clinical complexity of our patients, the rates in the nap-tested group fared well in comparison to results reported in the extant literature on PAP therapy adherence in typical sleep clinic settings.
In this small sample, a few associations were observed across groups for insomnia and mental health variables in relationship to PAP therapy use. Lower post-titration sleep efficiency, history of psychiatric disorders, and traumatic exposure were more common among non-users. Also, BMI was somewhat lower and post-titration AHI was higher in non-users. Taken together, these findings point to important clinical relationships among factors that might predict greater difficulty adjusting to pressurized airflow as early as the first titration test.34,35 However, more rigorous designs are needed test these hypotheses.
Six main benefits were observed with the PAP-NAP in this sample of complex sleep patients:
Brief, daytime, less threatening exposure to pressurized airflow
Meaningful desensitization trial of masks and PAP therapy during in vivo exposure in sleep or recumbent position
Consistent opportunities to identify and manage behavioral factors (notably emotional conflicts or imagery deficits) likely to interfere with PAP therapy adherence
The sleep specialist in our environment was readily available to assist in any aspect of the procedure, including personal contact time with the patient as indicated.
The procedure was reimbursable under existing CPT codes.10
The procedure appears to be a useful means to introduce behavioral sleep medicine concepts into daytime CPAP clinics.
The main limitations to the procedure identified through these pilot data are that sleep is not monitored during the PAP-NAP, and the PAP-NAP is inadequate for titration purposes, although these elements may not be required for successful outcomes. Other general limitations include the lack of outcomes data, assessment of other influences on adherence not measured in this study, the lack of generalizability to other populations and the use of historical controls instead of a randomized control group. Only pretest PAP-NAP questionnaire data were collected, preventing comparison of self-reported treatment outcomes. Many other factors may have influenced whether or not these patients continued use of PAP therapy, not the least of which would be the additional time spent with these patients36 regardless of any putative PAP-NAP effects. Another mediator may be that the vast majority responded better to bilevel than fixed CPAP during the titration phase, suggesting adherence may improve with simple expiratory relief.37 Also, this select sample was complex and vocally dismissive of PAP therapy. While they likely reflect similar types of patients in sleep medical clinical settings, they may not generalize to the larger group of patients who do not adhere to PAP therapy. Although an historical control suggests that the PAP-NAP procedure was influential in the adherence process, without a randomized control comparison, caution is advised in the interpretation of these findings.
In this retrospective review of the PAP-NAP, we conclude that this innovative, reimbursable procedure may prove to be a beneficial approach for exposing PAP therapy to complex insomnia patients who are likely to dismiss PAP therapy early in the course of treatment. Whether the PAP-NAP can be used in other types of patients is unknown, but it may be worth considering in those with sufficient skepticism or fears about sleeping with a breathing mask. Claims about the PAP-NAP as a tool to enhance adherence, however, remain speculative. Future studies in this area should focus on randomized control trials among problematic patients at-risk for nonadherence to PAP therapy, although case-by-case evaluation in the clinical setting may indicate a value for this daytime procedure among select patients.
ACKNOWLEDGMENTS
We wish to thank Dr. Lynn Hickman, our New Mexico Medicare Carrier Medical Director, for his advice on this project and manuscript. A special thank you to the following DME companies for their contribution of objective data downloads: A & R Medical Supply, Walgreens Home Care, Pneumexico Respiratory, Integrity Home Medical and Apria Healthcare.
Footnotes
Disclosure Statement
This was not an industry supported study. Dr. Krakow owns and operates Maimonides Sleep Arts and Sciences, Ltd., a for-profit sleep medical center and has published the following intellectual properties: Books – Insomnia Cures, Turning Nightmares Into Dreams, and Sound Sleep, Sound Mind; Websites – www.sleaptreatment.com, www.nightmaretreatment.com, and www.sleepdynamictherapy.com. Mr. Melendrez owns Quality Sleep Solutions, Inc., a for-profit sleep medical consulting company. The other authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Weaver TE. Adherence to positive airway pressure therapy. Curr Opin Pulm Med. 2006;12:409–13. doi: 10.1097/01.mcp.0000245715.97256.32. [DOI] [PubMed] [Google Scholar]
- 2.Golay A, Girard A, Grandin S, et al. A new educational program for patients suffering from sleep apnea syndrome. Patient Educ Couns. 2006;60:220–7. doi: 10.1016/j.pec.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Aloia MS, Di Dio L, Ilniczky N, Perlis ML, Greenblatt DW, Giles DE. Improving compliance with nasal CPAP and vigilance in older adults with OAHS. Sleep Breath. 2001;5:13–21. doi: 10.1007/s11325-001-0013-9. [DOI] [PubMed] [Google Scholar]
- 4.Likar LL, Panciera TM, Erickson AD, Rounds S. Group education sessions and compliance with nasal CPAP therapy. Chest. 1997;111:1273–7. doi: 10.1378/chest.111.5.1273. [DOI] [PubMed] [Google Scholar]
- 5.Lewis KE, Bartle IE, Watkins AJ, Seale L, Ebden P. Simple interventions improve re-attendance when treating the sleep apnoea syndrome. Sleep Med. 2006;7:241–7. doi: 10.1016/j.sleep.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Haynes PL. The role of behavioral sleep medicine in the assessment and treatment of sleep disordered breathing. Clin Psychol Rev. 2005;25:673–705. doi: 10.1016/j.cpr.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 7.Smith CE, Dauz ER, Clements F, et al. Telehealth services to improve nonadherence: A placebo-controlled study. Telemed J E Health. 2006;12:289–96. doi: 10.1089/tmj.2006.12.289. [DOI] [PubMed] [Google Scholar]
- 8.Kushida CA, Littner MR, Hirshkowitz M, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006;29:375–80. doi: 10.1093/sleep/29.3.375. [DOI] [PubMed] [Google Scholar]
- 9.Lee KA, Landis C, Chasens ER, et al. Sleep and chronobiology: recommendations for nursing education. Nurs Outlook. 2004;52:126–33. doi: 10.1016/j.outlook.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 10.American Medical Association. Current Procedural Terminology, CPT 2003. AMA: Chicago; 2002. [Google Scholar]
- 11.Krakow B. An emerging interdisciplinary sleep medicine perspective on the high prevalence of co-morbid sleep-disordered breathing and insomnia. Sleep Med. 2004;5:431–3. doi: 10.1016/j.sleep.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Stepnowsky CJ, Jr, Marler MR, Ancoli-Israel S. Determinants of nasal CPAP compliance. Sleep Med. 2002;3:239–47. doi: 10.1016/s1389-9457(01)00162-9. [DOI] [PubMed] [Google Scholar]
- 13.Stepnowsky CJ, Jr, Bardwell WA, Moore PJ, Ancoli-Israel S, Dimsdale JE. Psychologic correlates of compliance with continuous positive airway pressure. Sleep. 2002;25:758–62. doi: 10.1093/sleep/25.7.758. [DOI] [PubMed] [Google Scholar]
- 14.Wild MR, Engleman HM, Douglas NJ, Espie CA. Can psychological factors help us to determine adherence to CPAP? A prospective study. Eur Respir J. 2004;24:461–5. doi: 10.1183/09031936.04.00114603. [DOI] [PubMed] [Google Scholar]
- 15.Weaver TE, Maislin G, Dinges DF, et al. Self-efficacy in sleep apnea: instrument development and patient perceptions of obstructive sleep apnea risk, treatment benefit, and volition to use continuous positive airway pressure. Sleep. 2003;26:727–32. doi: 10.1093/sleep/26.6.727. [DOI] [PubMed] [Google Scholar]
- 16.Means MK, Edinger JD. Graded exposure therapy for addressing claustrophobic reactions to continuous positive airway pressure: a case series report. Behav Sleep Med. 2007;5:105–16. doi: 10.1080/15402000701190572. [DOI] [PubMed] [Google Scholar]
- 17.Chasens ER, Pack AI, Maislin G, Dinges DF, Weaver TE. Claustrophobia and adherence to CPAP treatment. West J Nurs Res. 2005;27:307–21. doi: 10.1177/0193945904273283. [DOI] [PubMed] [Google Scholar]
- 18.Krakow B, Melendrez D, Haynes P. Integrating psychosocial and biomedical CPAP adherence models. A commentary on: “Improving CPAP use by patients with the sleep apnea/hypopnea syndrome (SAHS)” (HM Engleman & MR Wild) Sleep Med Rev. 2003;7:441–4. doi: 10.1053/smrv.2002.0288. [DOI] [PubMed] [Google Scholar]
- 19.Indications for Polysomnography Task Force, American Sleep Disorders Association Standards of Practice Committee. Practice parameters for the indications for polysomnography and related procedures. Sleep. 1997;20:406–22. [PubMed] [Google Scholar]
- 20.Kribbs NB, Pack AI, Kline LR, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147:887–95. doi: 10.1164/ajrccm/147.4.887. [DOI] [PubMed] [Google Scholar]
- 21.McArdle N, Devereux G, Heidarnejad H, Engleman HM, Mackay TW, Douglas NJ. Long-term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med. 1999;159(4 Pt 1):1108–14. doi: 10.1164/ajrccm.159.4.9807111. [DOI] [PubMed] [Google Scholar]
- 22.Pepin JL, Krieger J, Rodenstein D, et al. Effective compliance during the first 3 months of continuous positive airway pressure. A European prospective study of 121 patients. Am J Respir Crit Care Med. 1999;160:1124–9. doi: 10.1164/ajrccm.160.4.9802027. [DOI] [PubMed] [Google Scholar]
- 23.Krakow B, Melendrez D, Ferreira E, et al. Prevalence of insomnia symptoms in patients with sleep-disordered breathing. Chest. 2001;120:1923–9. doi: 10.1378/chest.120.6.1923. [DOI] [PubMed] [Google Scholar]
- 24.Krakow B, Melendrez D, Lee SA, Warner TD, Clark JO, Sklar D. Refractory insomnia and sleep-disordered breathing: a pilot study. Sleep Breath. 2004;8:15–29. doi: 10.1007/s11325-004-0015-5. [DOI] [PubMed] [Google Scholar]
- 25.Krakow B, Melendrez D, Warner TD, et al. Signs and symptoms of sleep-disordered breathing in trauma survivors: a matched comparison with classic sleep apnea patients. J Nerv Ment Dis. 2006;194:433–9. doi: 10.1097/01.nmd.0000221286.65021.e0. [DOI] [PubMed] [Google Scholar]
- 26.Krakow B. Sound Sleep, Sound Mind. New York: John Wiley & Sons; 2007. Oct, [Google Scholar]
- 27.Krakow B. Insomnia Cures. The New Sleepy Times; 2002. [Google Scholar]
- 28.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 29.American Academy of Sleep Medicine. International classification of sleep disorders, 2nd ed.; diagnostic and coding manual. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 30.Rechtschaffen A, Kales A. A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Subjects. UCLA, Los Angeles: Brain Information Service/Brain Research Institute; 1968. [Google Scholar]
- 31.Krakow BJ, Melendrez DC, Johnston LG, et al. Sleep dynamic therapy for Cerro Grande fire evacuees with posttraumatic stress symptoms: a preliminary report. J Clin Psychiatry. 2002;63:673–84. doi: 10.4088/jcp.v63n0804. [DOI] [PubMed] [Google Scholar]
- 32.Spriggs W. Principles of polysomnography. Salt Lake City: Sleep Ed, LLC; 2002. [Google Scholar]
- 33.Krakow B, Melendrez D, Pedersen B, et al. Complex insomnia: insomnia and sleep-disordered breathing in a consecutive series of crime victims with nightmares and PTSD. Biol Psychiatry. 2001;9:948–53. doi: 10.1016/s0006-3223(00)01087-8. [DOI] [PubMed] [Google Scholar]
- 34.Rapoport DM. Methods to stabilize the upper airway using positive pressure. Sleep. 1996;19(9) Suppl:S123–30. doi: 10.1093/sleep/19.suppl_9.s123. [DOI] [PubMed] [Google Scholar]
- 35.Meurice JC, Paquereau J, Denjean A, Patte F, Series F. Influence of correction of flow limitation on continuous positive airway pressure efficiency in sleep apnoea/hypopnoea syndrome. Eur Respir J. 1998;11:1121–7. doi: 10.1183/09031936.98.11051121. [DOI] [PubMed] [Google Scholar]
- 36.Jensen PS, Weersing R, Hoagwood KE, Goldman E. What is the evidence for evidence-based treatments? A hard look at our soft underbelly. Ment Health Serv Res. 2005;7:53–74. doi: 10.1007/s11020-005-1965-3. [DOI] [PubMed] [Google Scholar]
- 37.Aloia MS, Stanchina M, Arnedt JT, Malhotra A, Millman RP. Treatment adherence and outcomes in flexible vs standard continuous positive airway pressure therapy. Chest. 2005;127:2085–93. doi: 10.1378/chest.127.6.2085. [DOI] [PMC free article] [PubMed] [Google Scholar]