Abstract
Patients with obstructive sleep apnea syndrome (OSAS) sometimes have atrioventricular (AV) block during sleep. However, significant resolution of such AV block with treatment for OSAS has been reported. On the other hand, during rapid eye movement (REM) sleep, conduction disturbances not associated with the apnea event can be observed, particularly in young healthy subjects. We report the case of a 67-year-old man with severe OSAS and 2:1 AV block that occurred only during the phasic events of REM sleep; continuous positive airway pressure (CPAP) treatment did not result in resolution of the AV block. No specific abnormalities were found on cardiac evaluation. Based on the analysis of overnight heart rate variability, CPAP treatment resulted in a markedly reduced ratio of low-frequency to high-frequency power and an increased high-frequency power, though high-frequency power was not increased during REM sleep on CPAP.
Citation:
Kawana F; Kasai T; Maeno KI; Momomura SI; Narui K. Atrioventricular block during the phasic events of REM sleep in a patient with severe obstructive sleep apnea syndrome. J Clin Sleep Med 2008;4(3):257-259.
Keywords: obstructive sleep apnea syndrome, heart rate variability, ratio of low frequency to high frequency, continuous positive airway pressure
Conduction disturbance has been reported during rapid eye movement (REM) sleep in normal subjects, in particular young healthy subjects, and it has been suggested that this is associated with enhanced parasympathetic activity.1 In cases with severe obstructive sleep apnea syndrome (OSAS), atrioventricular (AV) block has sometimes been observed during both REM and non-REM sleep.2 There are several reports of AV block during the phasic events of REM sleep in patients with no or mild OSAS. 3,4 It has been proposed that such AV block should specifically be called REM-sleep–related AV block. 3 However, the mechanisms for such AV block remain unclear.
We report a case with severe OSAS who presented with 2:1 AV block only during the phasic events of REM sleep.
CASE REPORT
A 67-year-old man was admitted to our hospital for evaluation of habitual snoring and excessive daytime sleepiness. There was no history of any cardiovascular diseases, and no abnormalities were detected on a previous electrocardiogram. The patient had never been athletic, either in his youth or more recently. The physical examination was normal except for obesity (body mass index, 26.1 kg/m2) and slightly elevated blood pressure (143/92 mm Hg). The admission electrocardiogram showed regular sinus rhythm with a heart rate of 62 per minute. Laboratory tests revealed no electrolyte disorder.
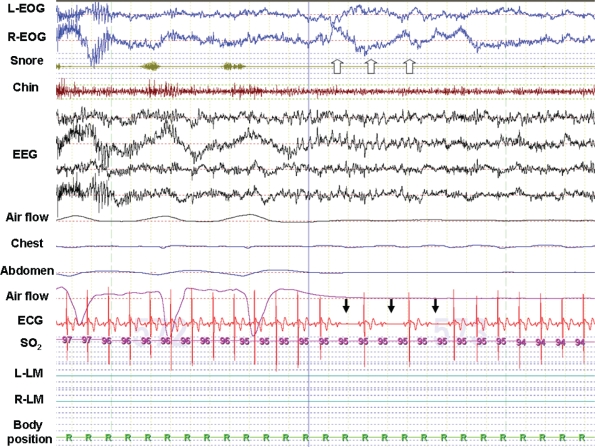
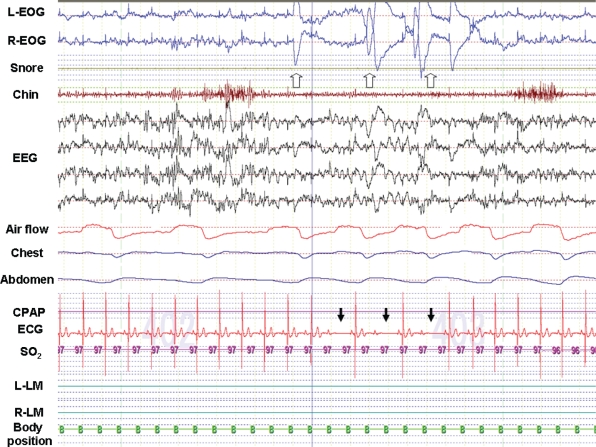
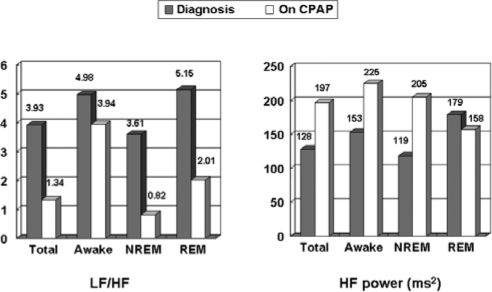
The initial polysomnogram showed an apnea-hypopnea index of 37.3 events per hour (consisting of 100% obstructive events) and an arousal index of 40.3 events per hour. Based on these results, the patient was diagnosed as having severe OSAS. Furthermore, apnea and hypopnea were present both in non-REM and REM sleep. Of note, the 2:1 AV block was documented only during phasic events of REM sleep (Figure 1a). Subsequently, to titrate the continuous positive airway pressure (CPAP), a second polysomnogram was performed with the patient on CPAP. Both the apnea-hypopnea index and the arousal index were reduced to 1.1 and 9.7 events per hour, respectively, on CPAP. Nevertheless, the 2:1 AV block persisted (Figure 1b). No significant abnormalities were observed on echocardiographic or electrophysiologic study. Heart rate variability (HRV) during polysomnogram was analyzed using commercially available software for frequency domain analysis of heart rate variability (R-R Interval Analysis, NoruPro Light Systems., Japan), which estimates the spectra using the MemCalc method; the low-frequency (LF; 0.04 Hz-0.150 Hz), high-frequency (HF; 0.150 Hz-0.400 Hz), and LF to HF power (LF/HF) ratio were calculated. In general, HF reflects parasympathetic activity, LF reflects both parasympathetic and sympathetic activity, and the LF/HF ratio reflects sympathetic activity. In this case, each 2 minute of recording were used as a window for HRV analysis, and HRV showed a markedly reduced LF/HF ratio and an increased HF power on CPAP during awakening, total sleep, and non-REM sleep, whereas the HF power was not increased during REM sleep on CPAP (Figure 1c). The Holter electrocardiogram showed no episodes of AV block during the day, and the patient did not complain of any symptoms. Therefore, the patient was not given specific treatment for 2:1 AV block.
Figure 1a.
Representative raw waveform on initial polysomnogram. The 2:1 atrioventricular (AV) block (black arrow) was documented during the phasic events of rapid eye movement (REM) sleep in the initial phase of the apnea or hypopnea episodes without hypoxia.
The white arrow indicates eye movement. The AV block occurred at the time of eye movement. The duration of this waveform is 30 seconds. L-EOG and R-EOG refer to left and right electrooculogram, respectively; EEG, electroencephalogram; ECG, electrocardiogram; SO2, oxyhemoglobin saturation; R-LM and L-LM, right and left leg movements, respectively.
Figure 1b.
Representative raw waveform on polysomnogram during continuous positive airway pressure (CPAP) titration. The 2:1 AV block (black arrow) during the phasic events of REM sleep persisted with the patient on CPAP. The white arrow indicates eye movement. The AV block occurred at the time of eye movement, as had occurred during the diagnostic polysomnogram. The duration of this waveform is 30 seconds.
Figure 1c.
Heart rate variability during diagnostic polysomnography and during polysomnography with the patient on CPAP. CPAP increased the high-frequency (HF) power during awake, non-REM, and the total night but not during REM sleep. However, CPAP reduced the low-frequency (LF)/HF ratio during REM sleep.
DISCUSSION
Although patients with OSAS sometimes have AV block during sleep in association with an apnea event, significant resolution of such AV block with treatment of the OSAS has been reported.5, 6 On the other hand, during REM sleep, AV block can be observed, particularly in young healthy subjects.1 It was initially thought that the AV block seen in the present patient was primarily associated with OSAS, since the patient had severe OSAS and was not a young athlete. Therefore, as has been previously reported, one would have supposed that CPAP would have been an effective treatment for AV block.5, 6 However, the patient's 2:1 AV block during phasic events of REM sleep continued even on CPAP. The laboratory data and echocardiographic and electrophysiologic studies ruled out an electrolyte disorder and an abnormality of the cardiac conduction system. Therefore, this patient appeared to have REM-sleep–related AV block, quite similar to that reported by Osuna et al.3 They reported one case with mild OSAS who had complete AV block only during phasic events of REM sleep, and, as in the present case, the complete AV block did not improve with CPAP treatment. On the other hand, Janssens et al4 have reported non-OSAS cases of REM-sleep–related bradyarrhythmia with decreased sympathetic tone and increased parasympathetic tone during REM sleep. In the present patient, both the LF/HF ratio and the HF power were greater during REM sleep than during non-REM sleep. In addition, the LF/HF ratio was reduced and the HF power was increased with the patient on CPAP during awakening, total sleep, and non-REM sleep. This may indicate that sympathetic tone was reduced and parasympathetic tone was increased during these periods with the patient on CPAP. However, the HF power was not increased during REM sleep on CPAP; this may indicate that parasympathetic tone was not increased during REM sleep with the patient on CPAP. These findings may indicate that AV block during REM sleep, which was observed even when the patient was on CPAP, was not provoked by enhanced parasympathetic tone. Although, the specific mechanisms for such AV block remain unclear, the present report highlights the existence of REM-related AV block that is not resolved by CPAP in nonathletic older patients with severe OSAS.
Footnotes
Disclosure Statement
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Adlakha A, Shepard JW., Jr Cardiac arrhythmias during normal sleep and in obstructive sleep apnea syndrome. Sleep Med Rev. 1998;2:45–60. doi: 10.1016/s1087-0792(98)90053-3. [DOI] [PubMed] [Google Scholar]
- 2.Koehler U, Fus E, Grimm W, et al. Heart block in patients with obstructive sleep apnoea: pathogenetic factors and effects of treatment. Eur Respir J. 1998;11:434–439. doi: 10.1183/09031936.98.11020434. [DOI] [PubMed] [Google Scholar]
- 3.Osuna E, Patiño G. REM sleep-related complete heart block. Is it a specific sleep-related disorder? Sleep Med. 2006;7:387–388. doi: 10.1016/j.sleep.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 4.Janssens W, Willems R, Pevernagie, et al. REM sleep-related brady-arrhythmia syndrome. Sleep Breath. 2007;11:195–199. doi: 10.1007/s11325-007-0105-2. [DOI] [PubMed] [Google Scholar]
- 5.Becker HF, Koehler U, Stammnitz A, Peter JH. Heart block in patients with sleep apnoea. Thorax. 1998;53(Suppl 3):S29–32. doi: 10.1136/thx.53.2008.s29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gula LJ, Krahn AD, Skanes AC, et al. Clinical relevance of arrhythmias during sleep: guidance for clinicians. Heart. 2004;90:347–352. doi: 10.1136/hrt.2003.019323. [DOI] [PMC free article] [PubMed] [Google Scholar]