Abstract
An isolate of Proteus mirabilis recovered from blood cultures of a diabetic patient was shown to be resistant to imipenem, meropenem, and ertapenem by disk diffusion susceptibility testing. Amplification of whole-cell and/or plasmid DNA recovered from the isolate with primers specific for the blaKPC carbapenemase gene produced an amplicon of the expected size which was confirmed to be blaKPC-2 by sequence analysis. Transformation of a susceptible Escherichia coli host with plasmid preparations from the isolate generated a transformant for which the MICs of all of the carbapenems tested were increased three- to fourfold. We believe this to be the first report of carbapenem resistance in P. mirabilis caused by the acquisition of blaKPC.
blaKPC-mediated carbapenem resistance among gram-negative bacteria is a relatively recent and emerging concern among health care practitioners in the United States. Chiefly limited to isolates of Klebsiella pneumoniae in initial surveillance reports (3-5), this carbapenem-hydrolyzing molecular class A β-lactamase has since been identified in a variety of Enterobacteriaceae including Escherichia coli (12), Enterobacter spp. (3, 7), Citrobacter spp.(7), Salmonella spp. (11), and Serratia marcescens (7), as well as Pseudomonas aeruginosa (16). The continued transfer of blaKPC between bacterial genera presents a serious challenge to infection prevention and control personnel because the enzyme mediates resistance not only to carbapenems but to all β-lactam antimicrobial agents, including cephalosporins, cephamycins, penicillins, and monobactams (13). Further, infection with blaKPC-producing bacteria is associated with higher patient mortality rates (4). Like many members of the family Enterobacteriaceae, Proteus spp. can harbor numerous plasmid- and integron-mediated antimicrobial resistance determinants (8, 9). Carbapenem resistance among Proteus spp. has previously been shown to be mediated by the OXA-23 molecular class D β-lactamase (2) or through porin mutation with or without decreased expression of penicillin binding proteins (15). Recently, Tsakris et al. (14) reported on the first isolate of P. mirabilis producing a VIM-1 molecular class B metallo-β-lactamase resulting in carbapenem resistance. Herein, we give what is believed to be the first report of a carbapenem-resistant isolate of P. mirabilis possessing a transmissible plasmid-mediated blaKPC-2 gene.
(This work was presented in part at the European Conference of Clinical Microbiology and Infectious Disease, Munich, Germany, 2007.)
The isolate of interest was presumptively identified as P. mirabilis on the basis of Gram staining, swarming motility on blood agar plates, inability to ferment lactose, and production of hydrogen sulfide, oxidase, and indole reactions, as well as phenotypic identification with the Vitek-2 identification system (bioMérieux, Marcy l'Etoile, France). Confirmation of the identification was accomplished by extended microbiological and biochemical techniques performed by the Missouri Department of Health Laboratory (Jefferson City). Antimicrobial susceptibility testing was performed by disk diffusion according to CLSI guidelines (6). In addition, MICs of ertapenem, meropenem, imipenem, and doripenem were determined with the Etest (AB Biodisk, Solna, Sweden). Inhibition of blaKPC activity was evaluated by disk approximation analysis as described previously (1).
Plasmid isolation, PCR, transformation, and restriction digestion. Total plasmid DNA was extracted from overnight cultures of the study isolate, the Top 10 E. coli host strain (TT), and selected transformants with the Qiagen plasmid mini extraction kit according to the manufacturer's procedures (Qiagen, Hilden, Germany). The presence of blaKPC was determined by conventional PCR with primers specific for blaKPC as described previously (5). Transformants were selected on nutrient agar plates containing 4 μg/ml imipenem. PCR-generated fragments were cloned into pCR-II and transformed into a chemically competent TT host according to the manufacturer's protocols (Qiagen). Transformants were selected on nutrient agar plates with 100 μg/ml ampicillin and screened by conventional PCR as described above.
DNA sequencing and analysis. Sequencing of the blaKPC PCR product cloned into pCR-II (TT/pPmir) was performed with primers F (5′-ATGTCACTGTATCGCCGTC-3′) and R (5′-CTCAGTGCTCTACAGAAAACC-3′) as described previously (16), with BigDye Terminator cycle sequencing kit v3.1 (Applied Biosystems, Inc., Foster City, CA) and an MJ Research PTC-200 DNA Engine thermal cycler (Bio-Rad Laboratories, Waltham, MA). Sequencing reaction mixtures were purified by ethanol precipitation, separated, and analyzed with an ABI PRISM 3100 genetic analyzer (ABI, Foster City, CA) by following the manufacturer's protocols. Forward and reverse strands of two independent PCR products were each sequenced. Sequences were aligned and compared to published sequences of the blaKPC-2 gene with Vector NTI v10.3.0 software (Invitrogen, Carlsbad, CA).
The study isolate was recovered from one of three cultures of blood drawn from a 53-year-old patient with uncontrolled diabetes mellitus. The patient was noncompliant with diabetes management and had recently undergone bilateral amputation of the lower extremities for gangrene. Prior antimicrobial therapy included vancomycin, cefepime, metronidazole, ciprofloxacin, and clindamycin. However, the patient had not been previously treated with a carbapenem. Disk diffusion testing indicated that the organism was resistant to imipenem, ampicillin, and cefazolin. Additional analysis with the Vitek2 automated system indicated that this organism was resistant to ampicillin, piperacillin, cefazolin, cefuroxime, and ceftriaxone; intermediately resistant to cefepime; and susceptible to piperacillin-tazobactam and ciprofloxacin. Because our laboratory was currently performing a prospective analysis of all carbapenem-resistant Enterobacteriaceae, the isolate was further tested for the presence of the blaKPC gene with conventional PCR assays. The patient was subsequently placed on piperacillin-tazobactam, followed by ciprofloxacin, and subsequent blood cultures were negative.
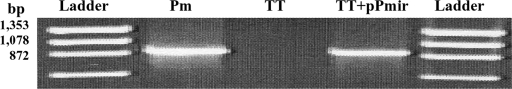
A single large plasmid (pPmir) was recovered from the study isolate (data not shown). Conventional and real-time (data not shown) PCR analyses of this plasmid, as well as total DNA, were positive for the presence of the blaKPC gene. Additional antimicrobial susceptibility testing with E-strips demonstrated that the MICs of doripenem, meropenem, imipenem, and ertapenem were >32 μg/ml (Table 1). Following transformation of the TT host strain, a single colony resistant to 4 μg/ml imipenem was selected and subcultured. As indicated in Fig. 1, a fragment of the size expected was generated from the transformant but not from the TT host strain. MIC testing of the transformant indicated that there was a three- to fourfold increase in the MICs of doripenem, meropenem, imipenem, and ertapenem compared to those for the susceptible host strain (Table 1). In addition, disk approximation analysis indicated an inhibition of blaKPC in the presence of clavulanate (data not shown).
TABLE 1.
MICs of the drugs tested in this study
| Drug | MIC (μg/ml)
|
Fold changed | ||
|---|---|---|---|---|
| P. mirabilisa | TT onlyb | TT/pPmirc | ||
| Meropenem | >32 | 0.047 | 0.125 | 3 |
| Ertapenem | >32 | 0.006 | 0.023 | 4 |
| Imipenem | >32 | 0.38 | 1.5 | 4 |
| Doripenem | >32 | 0.047 | 0.125 | 3 |
KPC (pPmir)-positive P. mirabilis.
Carbapenem-susceptible E. coli host strain.
E. coli host strain transformed with pPmir from P. mirabilis.
Fold difference between MICs for host strain and transformant.
FIG. 1.
KPC-specific PCR results generated from plasmid preparations of wild-type P. mirabilis (Pm), the TT host strain, and TT/pPmir. A fragment of the size expected (892 bp) was generated from wild-type P. mirabilis and the host strain transformed with the P. mirabilis KPC plasmid (pPmir) but not from the host strain.
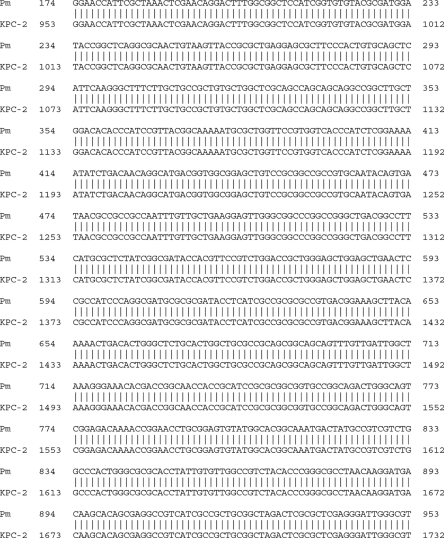
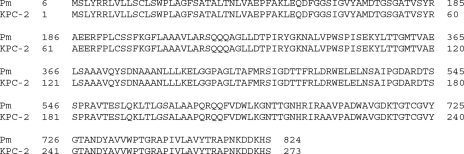
Isolated pPmir and TT/pPmir were submitted for sequence analysis with primers specific for blaKPC. A subsequent BLAST search showed that the amplified fragments were 100% homologous at the nucleic acid level (Fig. 2) and 100% identical at the amino acid level (Fig. 3) to the blaKPC-2 gene submitted to GenBank (accession no. AAK70220).
FIG. 2.
PCR and sequencing of pPmir and a subsequent BLAST search determined that the PCR fragment generated showed 100% homology with the KPC-2 gene sequence submitted to GenBank.
FIG. 3.
PCR and sequencing of pPmir and a subsequent BLAST search determined that the PCR fragment generated shared 100% identity with the KPC-2 protein sequence submitted to GenBank.
In this report, we describe what we believe to be the first reported case of infection caused by a strain of carbapenem-resistant Proteus mirabilis positive for the blaKPC-2 gene. While this finding is not totally unexpected, given the recent documented spread of blaKPC carbapenemase to a number of genera within the family Enterobacteriaceae (3-5, 11, 12), it is a disturbing trend, given the relatively recent discovery of this family of β-lactamases. While extended-spectrum β-lactamase and carbapenemase activities have previously been documented in Proteus species (2, 10, 14, 15, 17), the addition of blaKPC to the spectrum of resistance factors carried by an organism that traditionally has been placed in the low-level endogenous resistance category (similar to Klebsiella spp.) is equally troubling. It is possible that, as part of the normal gut flora, Proteus species may be unrecognized vectors for the dissemination of blaKPC until, as in our case, they are identified as a clinically significant cause of infection. As a case in point, until recently, KPC-positive K. pneumoniae recovered from urine might have gone unrecognized in our laboratory as carbapenems were not routinely tested versus urinary tract isolates. However, a prospective study initiated at our institution following the identification of our first KPC-positive K. pneumoniae isolate showed that nearly 12% of the K. pneumoniae strains recovered in our laboratory from all sources were positive for blaKPC. Most of these (64%) were urinary tract isolates with evidence of both clonal expansion and the introduction of unique, unrelated strains (data not shown). Currently, all of the carbapenem-resistant Enterobacteriaceae recovered in our laboratory are tested for the presence of blaKPC and of these, 99.0% contain blaKPC.
Our surveillance data indicate that blaKPC disseminates rapidly within a health care environment—primarily among strains of K. pneumoniae. However, we have also identified KPC-positive isolates of Enterobacter cloacae, Citrobacter freundii, Klebsiella oxytoca, and most recently, P. mirabilis. In an effort to curb this trend, we have begun routine screening of all gram-negative, carbapenem-resistant organisms for blaKPC with a real-time PCR assay. If positive, results are conveyed to infection prevention personnel for appropriate precautions.
Although the carbapenem MICs for transformed E. coli were considerably lower than those for the donor strain of P. mirabilis, all were three- to fourfold higher than those for the TT host recipient strain. While this finding was somewhat perplexing, it was not extraordinary since similar results have been reported by others (12, 18). Several possibilities exist to explain this observation: (i) the promoter associated with pPmir has low affinity for E. coli RNA polymerase, (ii) pPmir has a much lower copy number in the E. coli host, and/or (iii) the P. mirabilis donor strain has multiple mechanisms of carbapenem resistance, i.e., porin mutation or genetic determinants that the E. coli host does not have. In terms of the latter, we were unable to demonstrate the presence of a metallo-β-lactamase with an EDTA disk approximation test (data not shown).
In conclusion, we give here what we believe to be the first description of a KPC-positive strain of P. mirabilis. Based on this finding, it would be prudent to routinely screen all clinically relevant isolates of Enterobacteriaceae for carbapenem resistance—even under circumstances where the use of this class of drug for the treatment of infection would be less likely, i.e., uncomplicated urinary tract infection.
Acknowledgments
We thank Jennifer Bauer-Turpin for technical assistance with DNA sequencing.
The mention of trade names or commercial products in this report is solely for the purpose of providing specific information and does not imply recommendation or endorsement by the U.S. Department of Agriculture.
Footnotes
Published ahead of print on 16 July 2008.
REFERENCES
- 1.Anderson, K. F., D. R. Lonsway, J. K. Rasheed, J. Biddle, B. Jensen, L. K. Mcdougal, R. B. Carey, A. Thompson, S. Stocker, B. Limbago, and J. B. Patel. 2007. Evaluation of methods to identify the Klebsiella pneumoniae carbapenemase in Enterobacteriaceae. J. Clin. Microbiol. 452723-2725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bonnet, R., H. Marchandin, C. Chanal, D. Sirot, R. Labia, C. De Champs, E. Jumas-Bilak, and J. Sirot. 2002. Chromosome-encoded class D β-lactamase OXA-23 in Proteus mirabilis. Antimicrob. Agents Chemother. 462004-2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bratu, S., D. Landman, M. Alam, E. Tolentino, and J. Quale. 2005. Detection of KPC carbapenem-hydrolyzing enzymes in Enterobacter spp. from Brooklyn, New York. Antimicrob. Agents Chemother. 49776-778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bratu, S., M. Mooty, S. Nichani, D. Landman, C. Gullans, B. Pettinato, U. Karumudi, P. Tolaney, and J. Quale. 2005. Emergence of KPC-possessing Klebsiella pneumoniae in Brooklyn, New York: epidemiology and recommendations for detection. Antimicrob. Agents Chemother. 493018-3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bratu, S., P. Tolaney, U. Karumudi, J. Quale, M. Mooty, S. Nichani, and D. Landman. 2005. Carbapenemase-producing Klebsiella pneumoniae in Brooklyn, N.Y.: molecular epidemiology and in vitro activity of polymyxin B and other agents. J. Antimicrob. Chemother. 56128-132. [DOI] [PubMed] [Google Scholar]
- 6.Clinical and Laboratory Standards Institute. 2006. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard. CLSI document M7-A7. Clinical and Laboratory Standards Institute, Wayne, PA
- 7.Deshpande, L. M., P. R. Rhomberg, H. S. Sader, and R. N. Jones. 2006. Emergence of serine carbapenemases (KPC and SME) among clinical strains of Enterobacteriaceae isolated in the United States medical centers: report from the MYSTIC program (1999-2005). Diagn. Microbiol. Infect. Dis. 56367-372. [DOI] [PubMed] [Google Scholar]
- 8.Giske, C. G., D. L. Monnet, O. Cars, and Y. Carmeli on Behalf of ReAct—Action on Antibiotic Resistance. 2008. Clinical and economic impact of common multidrug-resistant gram-negative bacilli. Antimicrob. Agents Chemother. 52813-821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hall, R. M., and C. M. Collis. 1998. Antibiotic resistance in gram-negative bacteria: the role of gene cassettes and integrons. Drug Resist. Updates 1109-119. [DOI] [PubMed] [Google Scholar]
- 10.Luzzaro, F., M. Perilli, G. Amicosante, G. Lombardi, R. Belloni, A. Zollo, C. Bianchi, and A. Toniolo. 2001. Properties of multidrug-resistant, ESBL-producing Proteus mirabilis isolates and possible role of β-lactam/β-lactamase inhibitor combinations. Int. J. Antimicrob. Agents 17131-135. [DOI] [PubMed] [Google Scholar]
- 11.Miriagou, V., L. S. Tzouvelekis, S. Rossiter, E. Tzelepi, F. J. Angulo, and J. M. Whichard. 2003. Imipenem resistance in a Salmonella clinical strain due to plasmid-mediated class A carbapenemase KPC-2. Antimicrob. Agents Chemother. 471297-1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Navon-Venezia, S., I. Chmelnitsky, A. Leavitt, M. J. Schwaber, D. Schwartz, and Y. Carmeli. 2006. Plasmid-mediated imipenem-hydrolyzing enzyme KPC-2 among multiple carbapenem-resistant Escherichia coli clones in Israel. Antimicrob. Agents Chemother. 503098-3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Queenan, A. M., and K. Bush. 2007. Carbapenemases: the versatile β-lactamases. Clin. Microbiol. Rev. 20440-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsakris, A., A. Ikonomidis, A. Poulou, N. Spanakis, S. Pournaras, and F. Markou. 2007. Transmission in the community of clonal Proteus mirabilis carrying VIM-1 metallo-β-lactamase. J. Antimicrob. Chemother. 60136-139. [DOI] [PubMed] [Google Scholar]
- 15.Villar, H., F. Danel, and D. Livermore. 1997. Permeability to carbapenems of Proteus mirabilis mutants selected for resistance to imipenem or other beta-lactams. J. Antimicrob. Chemother. 40365-370. [DOI] [PubMed] [Google Scholar]
- 16.Villegas, M. V., K. Lolans, A. Correa, J. N. Kattan, J. A. Lopez, J. P. Quinn, and the Colombian Nosocomial Resistance Study Group. 2007. First identification of Pseudomonas aeruginosa isolates producing a KPC-type carbapenem-hydrolyzing β-lactamase. Antimicrob. Agents Chemother. 511553-1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vourli, S., H. Tsorlini, H. Katsifa, M. Polemis, L. S. Tzouvelekis, A. Kontodimou, and A. C. Vatopoulos. 2006. Emergence of Proteus mirabilis carrying the blaVIM-1 metallo-β-lactamase gene. Clin. Microbiol. Infect. 12691-694. [DOI] [PubMed] [Google Scholar]
- 18.Zhang, R., H. W. Zhou, J. C. Cai, and G.-X. Chen. 2007. Plasmid-mediated carbapenem-hydrolysing β-lactamase KPC-2 in carbapenem-resistant Serratia marcescens isolates from Hangzhou, China. J. Antimicrob. Chemother. 59574-576. [DOI] [PubMed] [Google Scholar]