Abstract
The intracellular bacterium Francisella tularensis survives in mammals, arthropods, and freshwater amoeba. It was previously established that the conventional media used for in vitro propagation of this microbe do not yield bacteria that mimic those harvested from infected mammals; whether these in vitro-cultivated bacteria resemble arthropod- or amoeba-adapted Francisella is unknown. As a foundation for our goal of identifying F. tularensis outer membrane proteins which are expressed during mammalian infection, we first sought to identify in vitro cultivation conditions that induce the bacterium's infection-derived phenotype. We compared Francisella LVS grown in brain heart infusion broth (BHI; a standard microbiological medium rarely used in Francisella research) to that grown in Mueller-Hinton broth (MHB; the most widely used F. tularensis medium, used here as a negative control) and macrophages (a natural host cell, used here as a positive control). BHI- and macrophage-grown F. tularensis cells showed similar expression of MglA-dependent and MglA-independent proteins; expression of the MglA-dependent proteins was repressed by the supraphysiological levels of free amino acids present in MHB. We observed that during macrophage infection, protein expression by intracellular bacteria differed from that by extracellular bacteria; BHI-grown bacteria mirrored the latter, while MHB-grown bacteria resembled neither. Naïve macrophages responding to BHI- and macrophage-grown bacteria produced markedly lower levels of proinflammatory mediators than those in cells exposed to MHB-grown bacteria. In contrast to MHB-grown bacteria, BHI-grown bacteria showed minimal delay during intracellular replication. Cumulatively, our findings provide compelling evidence that growth in BHI yields bacteria which recapitulate the phenotype of Francisella organisms that have emerged from macrophages.
Francisella tularensis is an extremely infectious gram-negative bacterium which is readily aerosolized. Inhalation of this category A select agent can lead to pulmonary tularemia, which in the absence of treatment has a mortality rate of 35%. Reportedly, antibiotic-resistant strains of this bacterium were developed by at least one nation's biological weapons program (30). The specter of such an agent being maliciously employed, in concert with the current lack of a licensed tularemia vaccine, has evoked a groundswell of interest in F. tularensis.
In addition to being a potentially fearsome biological weapon, F. tularensis is also a naturally occurring zoonotic bacterium found in strikingly diverse environments, such as mammals, arthropods, and possibly freshwater amoeba (30), and could reasonably be expected to display distinct phenotypes in these environments. The ability of F. tularensis to replicate within mammalian macrophages and amoebae is dependent upon the transcriptional regulator MglA (24). This DNA-binding protein, along with the related protein SspA (8) and the response regulator PmrA (29), coordinates the differential expression of F. tularensis genes known to be important for infection. The environmental cues that govern this regulation are unknown. The media most commonly used for cultivation of F. tularensis, Chamberlain's defined medium (CDM) (7) and Mueller-Hinton broth (MHB), have been shown to yield bacteria with phenotypes distinct from those displayed during mammalian infection (17, 44). Whether MHB- or CDM-grown bacteria mimic those found in arthropods, amoebae, or other environmental niches is currently unknown. Accordingly, one of the challenges faced by researchers using conventionally cultivated bacteria for in vitro assays is determining the extent to which their results relate to the progression of tularemia. Our long-term interests include the identification of bacterial surface proteins which are both (i) accessible to host antibodies and/or cellular receptors and, importantly, (ii) expressed during mammalian infection. In this quest, we favor various biochemical/biophysical approaches to directly label and/or enrich for outer membrane proteins (OMPs). While this approach is powerful, it is dependent upon starting with sufficiently large numbers of bacteria that are phenotypically identical to those causing a mammalian infection. Prior to starting our search for antibody-accessible OMPs of F. tularensis, we first sought to replicate the infection-derived phenotype of F. tularensis during in vitro growth. To this end, we characterized F. tularensis grown in brain heart infusion (BHI; a standard bacteriological medium infrequently used for Francisella). As positive and negative controls, we employed Francisella from infected macrophages (Mφ) and that grown in MHB, respectively.
Cumulatively, our results from a battery of technical approaches support the notion that BHI-grown Francisella cells closely mimic their host-adapted counterparts which have emerged from macrophages. Host adaptation of Francisella has both MglA-dependent and MglA-independent components and is inhibited by multiple components in MHB. Host-adapted bacteria show a minimal lag time during intramacrophage growth and trigger very low levels of proinflammatory cytokines. These findings have significant implications for the Francisella research community beyond our focused goal of identifying OMPs.
MATERIALS AND METHODS
Bacteria and media.
F. tularensis LVS (ATCC 29684; American Type Culture Collection) was provided by K. Elkins (U.S. Food and Drug Administration, Bethesda, MD). F. tularensis SchuS4, originally isolated from a human case of tularemia (15, 38), was obtained from the U.S. Army Medical Research Institute for Infectious Diseases (Frederick, MD). All experiments using SchuS4 were conducted within a Centers for Disease Control-certified animal biosafety level 3 facility at Albany Medical College. SchuS4 lysates for protein analysis to be performed outside this facility were generated by boiling harvested bacteria in 50 mM Tris, pH 8.0, containing protease inhibitors and 1% sodium dodecyl sulfate (SDS), followed by sterility testing. An in-frame mglA deletion mutant strain of LVS (46) was provided by Anders Sjostedt (Umea, Sweden). An Escherichia coli-F. tularensis shuttle vector (hereafter denoted pGFP-Kan) encoding kanamycin resistance and the green fluorescent protein driven by the F. tularensis groEL promoter was kindly provided by Tom Kawula (UNC).
Routine culturing of F. tularensis involved streaking aliquots of frozen bacterial glycerol stocks onto Mueller-Hinton chocolate agar plates (Becton Dickinson [BD], Sparks, MD), followed by 2 to 3 days of growth in a humidified chamber maintained at 37°C. Starter cultures were generated by resuspending several isolated colonies in ∼100 μl of BHI, from which ∼50 μl was immediately used to inoculate 3 to 5 ml of BHI and MHB for ∼18 h of growth on an orbital shaker operating at 200 rpm and 37°C. Mature starter cultures were used at a 1:100 dilution to inoculate larger volumes (10 to 50 ml within 125- to 250-ml Erlenmeyer flasks) of fresh media appropriate for each experiment. MHB was prepared with 21 g/liter Mueller-Hinton II broth powder, 1.2 mM CaCl2, 2.2 mM MgCl2, 0.1% glucose, 0.335 mM anaerobic ferric pyrophosphate (FePPi), and 2% Isovitalex (BD). BHI was prepared with 37 g/liter BHI powder, adjusted to pH 6.8, and sterile filtered. Initial attempts to propagate Francisella in BHI without pH adjustment were unsuccessful. A 10× stock of Casamino Acids (CAA) was prepared by dissolving CAA powder in BHI broth to a final concentration of 175 g/liter and was sterile filtrated (MHB contains 17.5 g/liter CAA). Individual amino acids (Sigma Chemical Company, St. Louis, MO) were dissolved to 200 to 400 mM in 18 MΩ/cm H2O (acidified where required for solubility) and sterile filtered.
Tissue culture.
Unless stated otherwise, tissue culture was performed using high-glucose Dulbecco's modified Eagle's medium (DMEM; contains 120 mM NaCl, 1.6 μM iron, and 7.3 mM free amino acids) (HyClone, Logan, UT) containing 10% fetal bovine serum (Pel-Freez, Rogers, AK), 100 U/ml penicillin-100 μg/ml streptomycin (Gibco/Invitrogen, Grand Island, NY), 2 mM GlutaMAX (Gibco), 10 mM HEPES (Mediatech, Inc., Herndon VA), 0.075% sodium bicarbonate (Mediatech), and 50 μM β-mercaptoethanol (Sigma). Bone marrow-derived macrophages (BMDM) were harvested from BALB/c, C57/BL6, and C3H/HeN mice (all from Taconic Farms, NY); the murine macrophage-like cell line RAW 264.7 was cultured as described previously (27). Murine hybridomas producing monoclonal antibodies (MAbs) directed against IglB and IglC were graciously provided by Francis Nano (University of Victoria).
Generation of Mφ-grown bacteria for SDS-polyacrylamide gel electrophoresis (SDS-PAGE) analysis.
To generate Mφ-grown F. tularensis LVS, adherent RAW cells at ∼75% confluence within four to six T-75 flasks were rinsed and replenished with antibiotic-free DMEM (13 ml/flask). MHB-grown bacteria were (i) used to inoculate fresh MHB and BHI at a dilution of 1:500 and (ii) harvested by centrifugation (4,000 × g, 10 min) and resuspended in either 1 ml of antibiotic-free DMEM (for Mφ infections) or 50 mM Tris, pH 8.0, containing protease inhibitors (TrisPI) for subsequent protein analysis. Mφ infections were initiated at a multiplicity of infection (MOI) of ∼500 and allowed to proceed for 8 h within a tissue culture incubator, after which the medium (with remaining extracellular bacteria) was recovered. Monolayers were rinsed as described above, incubated for 1 h with medium containing 50 μg/ml gentamicin, rinsed five times, and replenished with ∼13 ml of fresh antibiotic-free DMEM prior to further incubation. The bacteria remaining extracellular after 8 h of infection were subjected to two to four low-speed (500 × g, 10 min) spins to remove any Mφ; supernatants from each spin were examined by dark-field microscopy for contaminating eukaryotic cells. The Mφ-free supernatants were subjected to three high-speed spins (12,500 × g, 15 min) with intervening washes with DMEM (containing only buffers) to reduce the amount of eukaryotic proteins; washed bacteria were resuspended in TrisPI for subsequent protein analysis. At 24 h postinfection, the extracellular bacteria from half of the monolayers, along with the subcultures in MHB and BHI, were harvested and resuspended in TrisPI as described above (the 48-h flasks were merely supplemented with 7 ml fresh medium). The 24-h monolayers were rinsed three times with DMEM, harvested with a cell scraper into 10 ml phosphate-buffered saline (PBS) containing protease inhibitors, 0.2 μl/ml Benzonase (Sigma), and 1% Tween 20, and lysed by repeated rapid passage through a 21-gauge needle (lysis was monitored by microscopy). Eukaryotic debris was removed by multiple low-speed spins (monitored by microscopy); bacteria were washed and harvested as described above. At 48 h, the remaining flasks were processed similarly, except that because many Mφ were detached, the eukaryotic cells recovered from the first monolayer supernatant were added (after extensive washes, monitored by dark-field microscopy) to the recovered monolayer cells prior to lysis. While the above protocol routinely yielded rather clean preparations of bacteria, we did not presume that these preparations were devoid of mammalian proteins. However, the presence or absence of host protein contamination would have no influence on Western blots for bacterial proteins.
SDS-PAGE and Western blot analysis.
Samples of Francisella (10 μg [∼1 × 108 cells]) were mixed with Laemmli sample buffer and boiled for 10 min prior to resolution through 4 to 12% gradient SDS-PAGE precast gels (Invitrogen). The running buffer was NuPAGE morpholineethanesulfonic acid-SDS buffer from Invitrogen; gels were variously run at 90 to 160 V. Resolved gels were stained with Coomassie blue (Bio-Rad) or transferred to nitrocellulose membranes. Coomassie-stained gels were scanned into Adobe Photoshop by use of an HP 2820 scanner. Membranes to be probed with MAb were blocked for 15 min with PBS, 0.05% Tween 20, and 1% casein; blots to be probed with polyclonal sera were blocked for 1 h with PBS, 0.05% Tween 20, 2.5% horse serum, and 1% casein. Polyclonal sera were applied for 1 to 2 h at dilutions ranging from 1:1,000 to 1:60,000. Supernatants from MAb-producing hybridomas were applied for overnight incubations. The MAb specific for F. tularensis O antigen (Abcam) was used overnight at a dilution of 1:1,000. Blots to be probed multiple times were first probed with MAb prior to being stripped and reprobed with polyclonal sera. Horseradish peroxidase-conjugated secondary antibodies were used at dilutions ranging from 1:1,000 to 1:20,000. Development of the chemiluminescent substrate (SuperSignal West Pico; Pierce, Rockford, IL) was visualized using an Alpha Innotech imaging system in movie mode. Densitometric analysis of developed blots was performed on the same system. Primary antibodies were generously provided by Francis E. Nano (University of Victoria) and Terry Otto (Immuno-Precise Antibodies, Ltd.) (anti-MglB, anti-IglC, and anti-IglB), Daniel L. Clemens (UCLA) (anti-GroEL, anti-KatG, anti-SodB, and anti-Bfr), Micheal V. Norgard and Jason F. Huntley (University of Texas Southwestern Medical Center) (anti-Tul4A, anti-Mip, anti-Pal, and anti-FopA), and Eric R. LaFontaine (University of Georgia) (anti-FspA).
Macrophage infections for cytokine analysis and mitogen-activated protein (MAP) kinase assays.
BMDM seeded in 24- or 48-well plates were coincubated with various MOIs of F. tularensis that had been grown in MHB or BHI or harvested from previously infected BMDM. Lipopolysaccharide (LPS) from E. coli O111:B4 (Sigma) was similarly employed as a positive control. After 18 h, the media were analyzed by enzyme-linked immunosorbent assay or cytometric bead array to detect interleukin-12 p40 (IL-12p40) or tumor necrosis factor alpha (TNF-α), IL-6, and IL-10, respectively; the Greiss reaction was used to measure nitrite levels as an indicator of nitric oxide production. For nitrite determinations, Mφs were pretreated for 12 h with 100 u/ml of gamma interferon prior to bacterial infection (26). Phosphorylated forms of extracellular signal-regulated kinase, p38, and Jun N-terminal protein kinase present after 30 min and 1 and 2 h of bacterial infection were detected by cytometric bead array (BD).
PCA.
Principal component analysis (PCA) was performed on a 3-by-10 data matrix, where the rows of the matrix were bacterial growth conditions (MHB, BHI, and Mφ) and the columns were measurements of differentially expressed bacterial proteins (IgIC, IgIB, KatG, MgIB, and FsaP) and host responses (TNF-α, IL-12, nitrite, IL-6, and IL-10). Due to differences in the spread of data between proteins and host responses, the data were normalized so that the relationships in the data became more apparent without impacting the final analysis. Using a PCA algorithm, two principal components captured 100% of the information in the original data matrix, reducing the 10-dimensional data matrix to 2 dimensions with no loss of information. The dimensions were defined based on the eigenvectors of the original data matrix, where only the eigenvectors corresponding to the largest eigen values needed to be included. By doing this dimensionality reduction, the trends and intercorrelations in the data become visually apparent. The score values captured the relationships among the bacteria, while the loading values compared the proteins and host responses based on their contributions to classifying the bacteria. For convenience in interpreting the relationships between the bacteria, the proteins, and the host responses, a biplot was created with axes of PC1 and PC2.
Determination of intramacrophage replication.
BMDM from C3H/HeN mice which had been seeded into 24-well plates were infected for 2 h with MHB- or BHI-grown F. tularensis LVS at an MOI of 100. Following two gentle washes with PBS, the monolayers were treated for 1 h with DMEM containing 50 μg/ml gentamicin and washed twice prior to replenishment with fresh antibiotic-free medium. At the indicated times, bacteria within the culture supernatant were combined with those liberated from the macrophages by treatment with 0.1% sodium deoxycholate. Dilutions of the recovered bacteria were plated on Mueller-Hinton chocolate agar plates to determine CFU, which were read 48 h after the designated harvest time. Infections were performed in duplicate, and CFU determinations were performed in triplicate.
Mouse survival studies.
Mice were obtained from Taconic and maintained in the Albany Medical College animal facility. Infection and survival studies were performed as described previously (23). Anesthetized mice were inoculated intranasally with the desired CFU of F. tularensis LVS within 50 μl PBS; bacterial doses that were actually delivered were confirmed by plating of dilutions on Mueller-Hinton chocolate agar. Mouse viability was monitored once or twice daily. All animal procedures were approved by the Albany Medical College Institutional Animal Care and Use Committee.
RESULTS
Growth of F. tularensis in BHI and macrophages induces a similar set of MglA-dependent and MglA-independent changes.
As previously reported (25), we observed that Trypticase soy broth (TSB) and BHI broth supported growth of F. tularensis which was grossly similar to that in the conventional media CDM and MHB. SDS-PAGE analysis revealed that CDM- and MHB-cultivated bacteria displayed similar protein profiles, which differed from those of TSB- and BHI-grown cells, which were similar to each other (data not shown). Since two abundant proteins present in TSB- and BHI-grown cells were similar in size (∼23 and ∼57 kDa) to those induced by growth in Mφ (17), we proceeded to more extensively characterize F. tularensis LVS grown in BHI with respect to proteins known to be up- or downregulated during infection of either cultured Mφ or mice. As controls, we used MHB-grown bacteria as well as those that had replicated in and emerged from cultured macrophages.
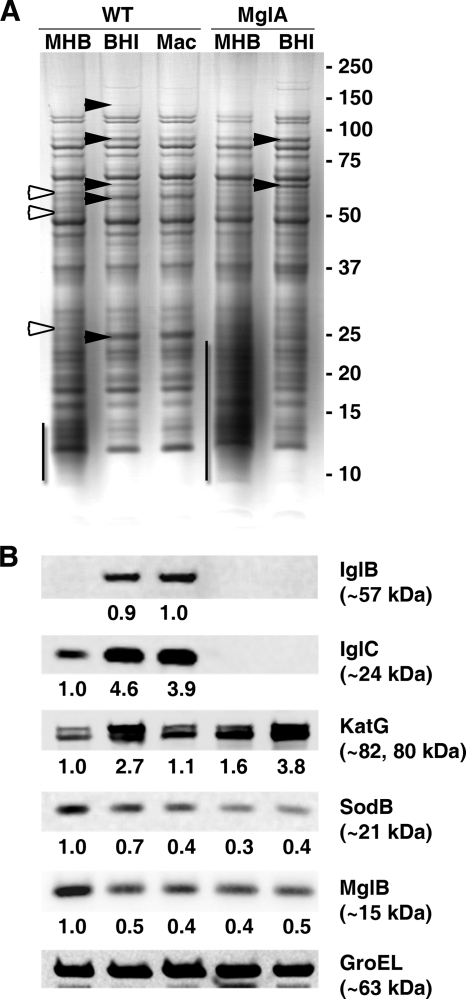
As shown in Fig. 1A, growth of F. tularensis in BHI and Mφ induces highly similar protein profiles which differ markedly from that of MHB-grown bacteria. Most notable are proteins of ∼128, ∼82, ∼61, ∼57, and ∼24 kDa (present in BHI- and Mφ-grown cells) and a low-molecular-weight (LMW) diffuse material that is present specifically in MHB-cultivated bacteria. Western blot analysis revealed increased levels of IglB (FTL0112), IglC (FTL0111), and catalase (KatG; FTL1504) among BHI- and Mφ-grown bacteria (Fig. 1B). These proteins are known to be upregulated during host infection compared to growth in either CDM or MHB (17, 44). Interestingly, the degree of KatG induction in Mφ-grown bacteria was less than that previously reported for bacteria recovered from infected mouse spleens (44) and less than that observed for BHI-grown bacteria (Fig. 1B). Superoxide dismutase (SodB; FTL1791), whose expression is decreased during animal infection (44), was downregulated by growth in BHI and Mφ. MglB (FTL1184), whose expression in vivo has not been characterized, was reduced in both BHI- and Mφ-grown cells. Western blots performed with a MAb specific for the O antigen of F. tularensis did not suggest any changes in the glycosylation of LPS among these bacteria (data not shown).
FIG. 1.
Growth of F. tularensis in BHI and Mφ induces similar sets of MglA-dependent and MglA-independent changes. Lysates (10 μg/lane) of F. tularensis LVS grown to late log phase in MHB and BHI or harvested from the tissue culture medium of infected RAW 264.7 cells were resolved by SDS-PAGE and stained with Coomassie blue or transferred to nitrocellulose for Western blotting. (A) Filled arrowheads indicate Coomassie-visible bands more abundant in lysates of BHI- and Mφ-grown cells; empty arrowheads indicate bands more abundant in MHB-grown Francisella. The LMW diffuse material is indicated by vertical lines. WT, wild type. (B) Western blots were performed on two identical membranes, which were probed, developed, and stripped for subsequent reprobing. The first membrane was probed sequentially with Abs against IglC, KatG, and GroEL, and the second membrane was similarly probed for IglB, SodB, and GroEL; observed molecular masses are indicated in parentheses. Numerical values below each blot indicate inductions (x-fold) over levels in wild-type LVS grown in MHB; the levels of induction were subsequently normalized to GroEL content. For IglB, the signal for Mφ-grown bacteria was compared to that for BHI-grown cells.
MglA (FTL1185) is a transcriptional regulator which activates many pathogenicity island genes, such as IglC, IglB, and PdpB (FTL0125; 128 kDa), and represses others, such as KatG (2, 5, 8, 18, 24). To determine if growth in BHI was stimulating any MglA-independent changes, we also examined the phenotype(s) of an mglA mutant in this medium. This strain of F. tularensis LVS, harboring an in-frame deletion of mglA, was able to effect some of the BHI- and Mφ-induced changes (induction of KatG and loss of the LMW diffuse material), whereas others (upregulation of IglB and IglC) were predictably ablated (Fig. 1B). While transposon insertion of MglA has been reported to ablate MglB expression, an inactivating point mutation of mglA causes only a reduction in MglB expression (2), similar to what we observed with the mglA deletion mutant.
The Mφ/BHI phenotype is reversible, begins in vitro during log-phase growth, and is inhibited by components of MHB.
Next, we monitored the phenotype of bacteria over the course of a full growth cycle in vitro. To determine whether we were observing medium-dependent changes in gene expression (as opposed to the accumulation of mutant/variant organisms [6]), MHB- or BHI-grown cultures were used to inoculate the opposite medium and then incubated for 36 h. During this time, we monitored growth (by optical densities and CFU counts) and periodically harvested samples for subsequent protein analysis.
After 4 h of growth in the new media, the protein profiles of the two cultures were indistinguishable, with both lacking visible expression of the 128-, 82-, 57-, and 23-kDa proteins yet containing the LMW diffuse material (see Fig. S1A in the supplemental material). At this early point (lag phase), the cultures had similar optical densities and equivalent CFU per ml (see Fig. S1B in the supplemental material). At 12 h of growth, which corresponds to mid-log phase, the bacteria growing in BHI began to display elements of the Mφ phenotype (i.e., the loss of the LMW diffuse material, decreased MglB expression, and increased expression of IglB and IglC) (Fig. 2A). This phenotype developed to a stable maximum at 20 h, which corresponds to entry into stationary phase, at which time KatG expression became evident. In contrast, the Francisella cells growing in MHB maintained the LMW material and failed to express elevated levels of IglB, IglC, or KatG at any time. Despite the increasing optical densities of these MHB cultures, the growth rate (as determined by CFU counts) began to diminish at the same time that the Mφ phenotype was developing in the BHI cultures. Beginning at ∼16 h, the discrepancy between optical densities and CFU counts became visually apparent by both dark-field and scanning electron microscopy. At this time, the MHB-grown Francisella cultures contained both larger pleomorphic cells with variegated surfaces and cellular aggregates (see Fig. S1C in the supplemental material). Prior to this time, the BHI- and MHB-grown bacteria were morphologically indistinguishable by dark-field microscopy.
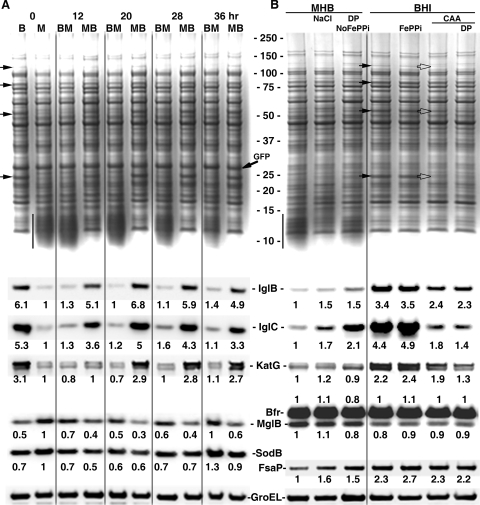
FIG. 2.
The Mφ/BHI phenotype is reversible, begins in vitro during log-phase growth, and is repressed by components of MHB. (A) Cultures of F. tularensis LVS (pGFP-Kan) grown in BHI (B) and MHB (M) were used to inoculate the opposite medium and incubated for 36 h. BM, BHI-grown cells placed into MHB medium; MB, MHB-grown cells placed into BHI medium. Aliquots were harvested periodically for analysis by SDS-PAGE and Western blotting; growth was monitored by absorbance and CFU formation. Arrows are as described in the legend to Fig. 1. Western blots were performed on two identical membranes as described in the legend to Fig. 1. The first membrane was probed with a cocktail of MAbs against IglB and IglC and then sequentially with sera against KatG and GroEL, and the second membrane was similarly probed with a mixture of sera against MglB and SodB, followed by serum against GroEL. GroEL-normalized levels of induction were determined as described in the legend to Fig. 1. (B) F. tularensis LVS was grown to late log phase in unaltered MHB and BHI or in medium that had been modified as follows: MHB plus NaCl to 150 mM, iron pyrophosphate-free MHB (NoFePPi) containing 100 μM dipyridyl (DP), BHI containing 335 μM FePPi, or BHI containing 17.5 g/liter CAA, with or without 100 μM dipyridyl. Arrows on the Coomassie blue-stained gel indicate bands which visibly increased (filled arrowheads) or decreased (empty arrowheads) compared to those in the preceding lane. Western blots were performed as described above. The first membrane was probed sequentially with Abs against a mixture of IglB and IglC and Abs against KatG and GroEL, and the second membrane was similarly probed with a mixture of Bfr and MglB sera and then with FspA and GroEL sera. GroEL-normalized levels of induction were determined as described in the legend to Fig. 1; levels of induction for Bfr are shown above the Bfr/MglB blot.
The above data suggested that components of MHB were repressing the BHI/Mφ phenotype. In contrast to both BHI and the mammalian intracellular and extracelluar environments, MHB is a low-salt medium that contains supraphysiological levels of iron (335 μM) and free amino acids (120 mM). Salt supplementation and iron depletion of MHB each resulted in modest changes in the expression of FsaP and IglC but did not induce the pronounced changes induced by growth in BHI; moreover, iron supplementation of BHI to the level found in MHB failed to blunt expression of the BHI/Mφ phenotype (Fig. 2B). Supplementation of BHI (which contains enzymatic digests of proteins) with free amino acids (CAA) to the level found in MHB quenched expression of IglB, IglC, and to a lesser extent, KatG; the iron chelator dipyridyl failed to reverse these effects (Fig. 2B). Since CAA supplementation did not alter the levels of MglB, Bfr (FTL0617), or FsaP and did not promote the formation of the LMW diffuse material, it appears that only a subset of the changes that occur during growth in BHI are inhibited by high concentrations of amino acids. The levels of free amino acids in vivo vary between ∼2 mM in plasma and ∼35 mM intracellularly (4).
Cumulatively, these observations suggest that expression of the genes previously associated with growth in vivo is also a normal part of log-phase growth in vitro and that inhibition of this expression (either by growth in MHB, as shown here, or by mutation of MglA [18]) has detrimental effects on bacterial growth/physiology.
BHI-grown F. tularensis cells most closely resemble extracellular Mφ-grown bacteria.
During the infectious cycle, F. tularensis replicates intracellularly for ∼24 to ∼48 h and then egresses into the extracellular milieu prior to infecting new cells (36). This extracellular phase was recently shown to be a significant component of mammalian tularemia (16, 48). To determine whether BHI-grown bacteria more closely resemble intracellular or extracellular bacteria, we compared them to those harvested at various times and from various cellular locations from infected macrophage cultures. For these experiments, Mφ-grown cultures were coincubated with MHB-grown Francisella for 8 h, after which the remaining extracellular bacteria were harvested. The Mφ monolayers were treated with gentamicin, washed, and provided with fresh antibiotic-free medium. At 24 and 48 h postinfection, both extracellular and intracellular bacteria were collected and washed. Consistent with our intention of monitoring a complete infection cycle, the majority of bacteria were intracellular at 24 h, whereas the majority of bacteria were extracellular at 48 h.
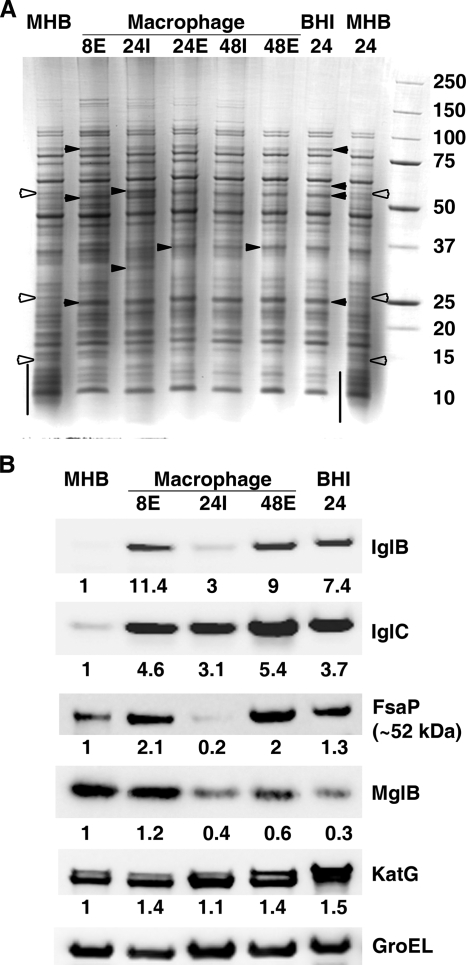
After 8 h of coincubation with macrophages, bacteria present in the extracellular compartment displayed increased levels of IglB, IglC, and KatG and decreased levels of the LMW diffuse material relative to those in the MHB-grown inoculum (Fig. 3A and B, lanes 8E). Given the concentrations of free amino acids in the Mφ culture medium (7.3 mM) and in serum (∼2 mM) compared to that in MHB (120 mM), these results are predictable in light of our results in Fig. 2B. FsaP (FTL1658), which is upregulated in mouse spleens versus MHB (44), was also increased in these extracellular bacteria. The levels of IglB, IglC, FsaP, and KatG were all modestly to profoundly reduced among the intracellular bacteria harvested at 24 h. Expression of these proteins was restored in the extracellular bacteria harvested at 48 h. The scant recovery of bacteria from the 24-h extracellular and 48-h intracellular groups precluded Western blot analysis of these two groups. MglB appeared to be downregulated in all bacteria that entered and replicated within macrophages (Fig. 3B). Considering the protein pattern visible on Coomassie-stained SDS-PAGE gels and the expression levels of IglC, IglB, KatG, SodB, FsaP, and MglB (Fig. 1B and 3B), it appears that BHI-grown bacteria most resemble Francisella cells that have replicated in and emerged from Mφ. Since MHB-grown bacteria show many discrepancies (IglC, FsaP, and MglB levels) with intracellular bacteria, the former do not appear to mimic the latter. Visual inspection of green fluorescent protein-expressing Francisella grown in MHB, BHI, and Mφ confirmed that the pleomorphic swelling and/or aggregation noted previously (see Fig. S1C in the supplemental material) for MHB-grown bacteria was not observed in either BHI- or Mφ-grown Francisella (see Fig. S2 in the supplemental material).
FIG. 3.
BHI-grown Francisella organisms most closely resemble extracellular, Mφ-grown bacteria. (A) MHB-grown F. tularensis LVS (lane MHB) was used to inoculate fresh MHB and BHI broths and to infect a murine Mφ cell line. At the indicated times (h), bacteria were harvested from the culture media and the extracellular (E) or intracellular (I) compartment of the Mφ cultures. Lysates (10 μg/lane) of each were resolved by SDS-PAGE, followed by staining with Coomassie blue or transfer to nitrocellulose for Western blot analysis. (A) Arrowheads and lines are as described in the legend to Fig. 1. (B) A single membrane was probed (as in Fig. 1) with a cocktail of MAbs against IglB and IglC, followed sequentially by sera against FsaP, MglB, KatG, and GroEL. Numerical values below each blot are GroEL-normalized levels of induction over those observed with MHB-grown cells.
Macrophages make little distinction between BHI- and Mφ-grown Francisella.
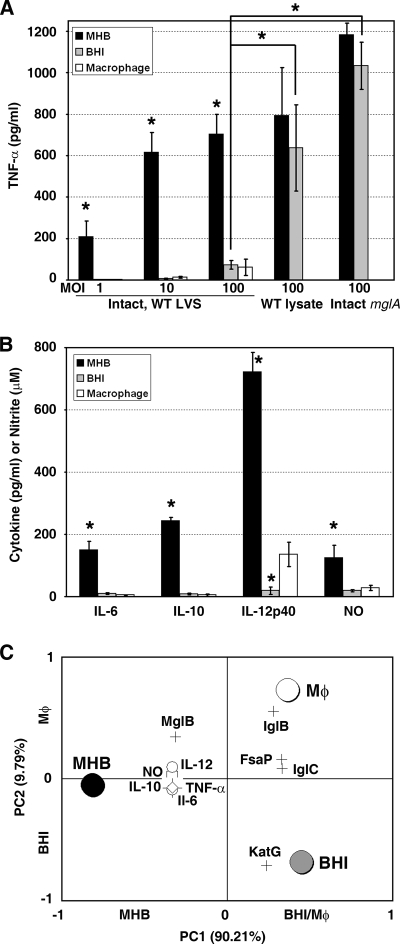
To further vet the notion that BHI-grown Francisella cells mimic their infection-derived extracellular counterparts, we next employed a biological assay to gauge the responses of naïve macrophages to differentially cultivated bacteria. F. tularensis LVS grown in MHB or on Thayer-Martin plates induces (9, 10, 21) or, as described in one report, initially induces and then represses (42) the production of proinflammatory cytokines (TNF-α, IL-12p40, IL-6, etc.) by responding naïve Mφ. In contrast, Mφ-grown Francisella elicits markedly lower levels of these cytokines (27). As shown in Fig. 4A and consistent with previous reports (9, 10, 21), MHB-grown bacteria were potent inducers of TNF-α at all MOIs up to 100 bacteria per host cell; cell-free, spent medium evoked no TNF-α production (data not shown). In contrast, both BHI- and Mφ-grown bacteria triggered markedly lowers levels of TNF-α secretion by naïve Mφ, even at the highest MOI. The only BHI-grown bacteria that elicited high levels of TNF-α were those incapable of complete host adaptation (mglA mutant) or those that had been disrupted by sonication (wild-type lysate) (Fig. 4A). Production of IL-6, IL-10, IL-12p40, and nitric oxide followed a similar pattern of modest induction by BHI- and Mφ-grown Francisella (Fig. 4B) (MOI = 100). Consistent with our cytokine results and with a previous report (42), infection of Mφ with MHB-grown bacteria induced a marked, transient increase in the phosphorylation of extracellular signal-regulated kinase, p38, and Jun N-terminal protein kinase. This spike in MAP kinase activity did not occur in response to BHI-grown bacteria (data not shown). Since production of several of the above cytokines in response to intact Francisella is primarily dependent on Toll-like receptor 2 (TLR2) (9, 10, 21, 28), host adaptation may involve downregulation of surface TLR2 agonists.
FIG. 4.
Naïve macrophages make little distinction between BHI- and Mφ-grown Francisella. (A and B) BMDM from BALB/c mice were incubated with F. tularensis LVS (prepared as indicated; MOI = 100 unless indicated otherwise) for 18 h, after which the culture supernatants were analyzed for cytokines and/or nitrite. Bars indicate the means and standard errors of the means for three or four independent experiments. Unless otherwise indicated, asterisks indicate values that differ significantly (P < 0.05) from those in the same category obtained with Mφ-grown bacteria. BMDM from C57BL/6 and C3H/HeN mice also produced more TNF-α and IL-6 in response to MHB-grown F. tularensis than in response to BHI-grown bacteria (data not shown). WT, wild type. (C) MHB-, BHI-, and Mφ-grown bacteria were classified based on the differences in their respective bacterial protein levels (shown as crosses) and induced host responses (shown as small symbols). PC1 captures the values which differentiate MHB- from BHI- and Mφ-grown bacteria, whereas PC2 captures the values which differentiate BHI- from Mφ-grown bacteria.
Having obtained multiple measurements of several differentially expressed bacterial proteins (IglB, IglC, etc.) and host responses (TNF-α, IL-6, etc.) to differentially grown bacteria, we sought to aggregate these data into a cumulative metric of similarity among MHB-, BHI-, and Mφ-grown bacteria. We turned to PCA, a mainstay of systems biology which is used to uncover complex patterns within large data sets (12, 19, 32, 39). For this analysis, we only considered data for which we had sufficient matched replicates (IglB, IglC, KatG, MglB, FsaP, TNF-α, IL-6, IL-10, IL-12, and nitrite levels in wild-type F. tularensis LVS grown in MHB and BHI and in Mφ-grown, extracellular bacteria). We first used these 10 values for each bacterium to describe a dimensionally reduced, numerical space (large circles in Fig. 4C). We then assessed variance among these 10 parameters (small symbols in Fig. 4C) as a function of the three growth conditions. Among these 30 values, ∼90% of the difference (principal component 1 [PC1]) was found between MHB-grown bacteria and those grown in BHI or Mφ; <10% of the total variance (PC2) was between BHI- and Mφ-grown Francisella (Fig. 4C). Based on this, we can say that the differences between MHB-grown and host-adapted (BHI- and Mφ-grown) bacteria are approximately nine times more significant than the differences between BHI- and Mφ-grown bacteria.
In models of infection, MHB-grown Francisella lags behind its BHI-grown counterpart.
As a final evaluation of the degree of host adaptation of BHI-grown F. tularensis, we compared this bacterium to that cultured in MHB, using two infection models, i.e., Mφ and mice. Since the Mφ/BHI phenotype begins to become evident in vitro at the protein level by ∼12 h and is complete by ∼20 h postinoculation, we reasoned that if BHI-grown bacteria are truly host adapted, they should “outpace” nonadapted bacteria during infection by roughly this period. After this time, the bacterial replication/infection would be predicted to proceed at the same rate.
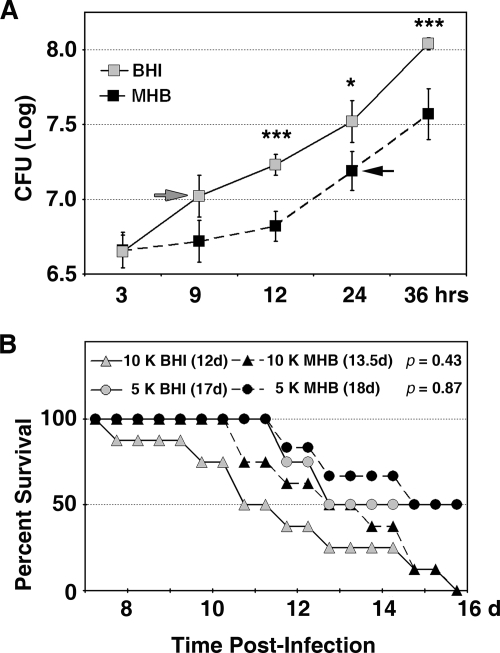
In the Mφ model, while bacterial entry was equivalent, intracellular replication of the BHI-grown Francisella proceeded immediately, resulting in a fourfold increase in bacteria within 12 h. In this same period, intracellular replication by MHB-grown bacteria was insignificant (Fig. 5A). After 12 h, MHB-grown bacteria replicated at the same rate as BHI-grown bacteria. Indeed, the data points for the BHI-grown Francisella fit a nearly linear pattern (R2 = 0.98), whereas replication of MHB-grown bacteria within Mφ was biphasic. We anticipated that this apparent 12-h “head start” might reduce the mean survival time of infected mice by approximately half a day. Surprisingly, in two independent experiments encompassing five groups of animals, mice infected with BHI-grown Francisella reproducibly had a 1- to 1.5-day shorter median survival time than mice infected with MHB-grown bacteria (Fig. 5B shows BALB/c mouse data; see Fig. S3 in the supplemental material for C57B/6 mouse data). The single exception to this trend was observed with C57B/6 mice infected with 5,000 CFU of MHB-grown bacteria, where a median survival time could not be calculated because <50% of these mice succumbed to infection. While, as expected, statistical significance was not achieved within any single group of infected mice, this reproducible trend lends support to the notion that BHI-grown F. tularensis is preadapted to the host environment, whereas MHB-cultivated bacteria must first adapt and then proceed with the infectious process.
FIG. 5.
In models of infection, MHB-grown Francisella cells lag behind their BHI-grown counterparts. (A) BMDM from C3H/HeN mice were incubated at an MOI of 100 for 2 h with F. tularensis LVS previously grown in MHB or BHI. After infection, the monolayers were washed, treated with gentamicin for 1 h, and replenished with antibiotic-free media. Total (intracellular plus extracellular) CFU were determined at the indicated times. Similar results were observed with BMDM from BALB/c mice (data not shown). Values are the means and standard deviations for two experiments performed in triplicate. Statistical analysis was performed by one-way analysis of variance with Tukey's posttest. Asterisks indicate significant differences (P < 0.05 to P < 0.001) in CFU recovered from MHB- and BHI-infected Mφ; arrows indicate the earliest time point at which CFU were significantly higher (P < 0.01) than at 3 h. (B) Two groups of BALB/c mice were intranasally infected with 5,000 or 10,000 CFU of MHB- or BHI-grown F. tularensis LVS and monitored daily for 21 days. Median survival times (days) are indicated within each panel above the survival curves, and P values (determined by the Kaplan-Meier log rank test, using GraphPad Prism 4 software) are indicated to the right of each group. No deaths occurred prior to day 3 or after day 16.
Growth in BHI also triggers host adaptation of human-virulent F. tularensis.
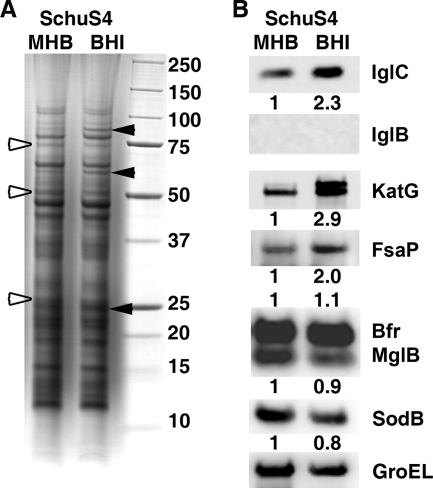
To determine if our findings with F. tularensis LVS would extend to type A strains, F. tularensis SchuS4 grown in MHB and BHI was analyzed by SDS-PAGE and Western blotting. As shown in Fig. 6, this strain also responded to growth in BHI by increasing expression of IglC, KatG, and FsaP and decreasing production of MglB and SodB. In contrast to strain LVS, in which IglB was detectable even in MHB-grown cells, in the SchuS4 strain this protein remained below our level of detection in both media. Similar findings for another type A strain (FSC033) were previously reported when the proteomes of MHB-grown and murine splenic bacteria were compared: IglC was upregulated in vivo, while IglB expression was not noted under either growth condition (44).
FIG. 6.
Growth in BHI triggers host adaptation of human-virulent F. tularensis. Lysates (10 μg/lane) of F. tularensis SchuS4 grown to late log phase in MHB and BHI were resolved by SDS-PAGE and stained with Coomassie blue (A) or transferred to nitrocellulose for Western blotting (B). The arrowheads in panel A and numerical values in panel B are as described in the legend to Fig. 1.
DISCUSSION
This study was prompted by two related facts. First, phenotypic variation in response to different growth conditions is well established among zoonotic bacteria, as is the impact of this variation on both vaccine development and basic research. A pertinent example is provided by the OspA/Lymerix vaccine against another zoonotic bacterium, Borrelia burgdorferi, the agent of Lyme disease. The abundant, immunogenic outer membrane protein OspA, which is expressed by in vitro-cultivated borreliae, was developed as a human vaccine (Lymerix) (22, 35, 37) prior to the recognition that OspA is downregulated as part of the bacterium's adaptation to the mammalian environment (1). As a result, immunity to OspA was inconsequential for the host-adapted spirochetes that were entering the host (3, 14); production of Lymerix was discontinued in 2002. The second impetus for our study is the established fact that MHB and CDM yield bacteria that are phenotypically dissimilar from those propagated during host infection (17, 44). Because our long-term goals include the direct biochemical identification of antibody-accessible OMPs that are expressed during infection, we considered the identification of appropriate in vitro cultivation conditions to be a requisite first step. Gratifyingly, these efforts appear to have been warranted, as MHB-grown bacteria contain a bevy of putative OMPs that are downregulated during host adaptation (data not shown).
In the process of comparing MHB-, Mφ-, and BHI-grown bacteria, we have made several unexpected observations which have implications for the broader Francisella research community. Perhaps the most profound is the simple observation that the infection-derived phenotype of this bacterium can be reproduced in vitro. The work of Golovliov et al. and Twine et al., comparing MHB- and CDM-grown F. tularensis to bacteria harvested from murine spleens and cultured macrophages, respectively, conclusively established that these media do not yield bacteria which mimic those derived from host infection (17, 44). Since differences between in vitro- and in vivo-grown bacteria are not uncommon and since MHB and CDM are established tools within the F. tularensis research community, the findings of Golovliov et al. and Twine et al. have largely been viewed within the context of “in vitro versus in vivo.” Our data indicate that many of the same genes examined in these previous studies are expressed by both BHI-grown and Mφ-grown extracellular bacteria. Since the splenic F. tularensis cells characterized by Twine et al. were harvested at 4 days postinfection (44), when the majority of bacteria in the circulation are extracellular (16), our protein expression data for MHB-grown and extracellular, Mφ-grown bacteria are highly concordant with those of Twine et al.
The bacterial differences imparted by the use of these media can markedly impact many bacterial and host systems currently under investigation. Multiple groups have utilized in vitro infection of macrophages by MHB-grown or similarly grown bacteria to examine the host receptors, signaling pathways, and cellular responses to infection with F. tularensis (9-11, 20, 21, 28, 42). With few exceptions, the cumulative picture painted by these reports is one in which F. tularensis engages TLR2 to activate NF-κB and the MAP kinase signaling pathways, which leads to the robust elaboration of proinflammatory cytokines, such as TNF-α, IL-6, IL-12p40, etc. We observed nearly identical outcomes with our MHB-grown bacteria. Accordingly, the findings described in the present study cannot be dismissed as the result of lab-to-lab variation in medium preparation. Experiments conducted in parallel with BHI- or Mφ-grown F. tularensis cells indicate that these host-adapted bacteria induce very low levels of MAP kinase activity and stimulate little or no secretion of proinflammatory cytokines. This was the case for an array of host cells (RAW 264.7 cells and BMDM from BALB/c, C57BL/6, and C3H/HeN mice) and was confirmed in two independent laboratories, using multiple, distinct batches of bacteria. Similarly muted responses to Mφ-grown bacteria have been noted for murine peritoneal Mφ, MHS cells (a murine alveolar Mφ line), and primary human monocytes (27). Because intranasally infected mice do not display measurable levels of proinflammatory cytokines in their lungs for the first ∼3 days postinfection (28), the use of host-adapted bacteria for in vitro infection models would seem to be an accurate reflection of the early disease process. The fulminant inflammatory response characteristic of late-stage disease presumably reflects the net accumulation of large numbers of bacteria. However, the possibility that the bacteria adopt a more inflammatory phenotype in this later stage has yet to be formally tested.
At this time, we cannot discern whether host adaptation induces downregulation of proinflammatory agonists, upregulation of active bacterial countermeasures that disrupt host signaling pathways, or a combination of both. Active suppression of host signaling networks by F. tularensis LVS has been suggested by the diminished responses to E. coli LPS (a TLR4 agonist) by infected Mφ (41); conversely, we have observed downregulation of at least one proven TLR2 ligand, Tul4A (43; data not shown). If preinfection of Mφ by BHI-grown bacteria were to blunt the subsequent cytokine responses elicited by superinfection with MHB-grown bacteria, we would be able to confirm active suppression as a component of the host-adapted phenotype. Conversely, downregulation of agonists (the stealth model) would be favored if cytokine responses to MHB-grown bacteria were unaffected by prior infection with BHI-grown Francisella.
Whether it is suppression or stealth, it is tempting to speculate that the immunologically quiescent phenotype we observe with BHI- and Mφ-grown F. tularensis is the same “nonstimulatory” phenotype that Francisella grown on Thayer-Martin plates adopts ∼5 h after Mφ infection (42). By following the activity of the NF-κB and MAP kinase signaling pathways and TNF-α production subsequent to infection of Mφ by F. tularensis, Telepnev et al. were able to observe a rapid increase in signaling (and subsequent TNF-α elaboration) which waned over time, reaching background levels at ∼5 h postinfection (42). Conversely, Mφ-grown bacteria lose ∼50% of their nonstimulatory phenotype after ∼6 h of incubation in MHB (27). Since these times (∼4 to 6 h) correlate with the timing of phagosome escape and entry into the cytoplasm, it is tempting to speculate that bacterial location dictates production of inflammatory mediators. This “location” hypothesis would seem to be supported by the observation that bacteria incapable of phagosome escape (killed bacteria and live mglA [or iglC] mutant strains) induce high levels of signaling and cytokine production (34, 42). However, because these phagosome escape mutants are incapable of host adaptation, the loss of host signaling is surely more complicated than simply a matter of location. Dissecting the influence of these interrelated processes and addressing the contributions of active silencing and/or stealth remain a formidable, yet intriguing, set of scientific objectives.
Our comparison between the phenotypes of MHB- and BHI-grown cells has offered important insights into factors in MHB which repress the host-adapted phenotype of F. tularensis. Like others before us (13, 26, 40), we noted that environmental iron levels influence bacterial gene expression. We observed increased levels of IglC in bacteria grown in Fe-depleted MHB, consistent with alleviation of Fur-dependent repression but not with activation of MglA/SspA. Since the struggle between host and pathogen for iron is a central paradigm of bacterial pathogenesis (31, 33, 45), the observation that select virulence genes are repressed by elevated iron (a well-characterized signal that cues bacteria to repress mammal-associated virulence genes [31, 33, 45]) is predictable. The concentration of free iron within the mammalian environment is estimated to be 10−9 μM (45). The high concentration of iron (335 μM) in MHB does not mimic the mammalian environment and serves to repress the host-adapted phenotype of this pathogen.
Expression of IglC, IglB, and KatG (and likely others) is induced in BHI. Supplementation of BHI with FePPi failed to reverse this effect, suggesting that iron depletion is not the activating signal for these genes in BHI. Induction of these proteins could be blunted by supplementation of BHI with free amino acids. Since IglB and IglC are regulated by PmrA (FTL0552), MglA, and SspA (FTL1606), it is tempting to hypothesize that one or more of these factors are responsive to amino acid levels. Since the prototypical SspA protein of E. coli is responsive to nutrient levels (47), it is reasonable to assume that either MglA (an SspA ortholog) or F. tularensis SspA may be similarly responsive. Using a different approach, Guina et al. recently concluded that MglA regulates the Francisella novicida response to starvation and oxidative stress, although the nature of the starvation was not defined (18). In vivo, the levels of free amino acids vary from ∼2 mM in plasma to ∼35 mM within the host cell (4), such that the bacterium is routinely exposed to amino acid fluctuations during mammalian infection. We speculate that amino acid levels may contribute to the modulation of intracellular versus extracellular gene expression (Fig. 3). An additional component of MHB, Isovitalex (which contributes 15 mM glutamine and ∼4 mM cystine), also contributes to the repression of the host-adapted phenotype (data not shown). The level of free amino acids in MHB (120 mM; 75 mM in CDM) is not representative of any mammalian niche and further serves to repress the bacterium's host-adapted phenotype. Thus, for investigations seeking to elucidate in vitro the behavior and physiology of this pathogen as it exists during mammalian infection, BHI represents a choice which better replicates the mammalian environment. While it is unlikely that BHI-grown bacteria are an exact match of the extracellular bacteria found during mammalian infection, they do appear to be a much closer approximation than those grown in MHB.
Our work takes no position on the relative merits of studying amoeba- or arthropod-adapted Francisella cells or on the study of mammalian responses to these bacteria. Given the multiple potential sources of infection with F. tularensis, all types of bacteria are of concern in considering the initial infection. In this vein, it would be interesting to determine if growth in MHB or CDM mimics that in an environmental niche. In any case, bacteria from all sources will presumably adapt to the mammalian environment by ∼8 to 12 h postinfection, and it is these adapted bacteria that continue the disease for the next week or so until death. Accordingly, studies of host-adapted bacteria and the responses to these organisms should elucidate the mechanisms of disease progression and pathogenesis that exist during the bulk of the mammalian infection. The choice of bacterial medium is perhaps less important for experiments that exclusively register murine survival. However, the use of adapted bacteria is more critical for in vitro models seeking to mimic the pathogen-host cell interactions that drive tularemia pathogenesis. Such models could include those delineating the engagement of host receptors, the initiation of host cell signaling pathways, host transcriptional responses, cytokine elaboration, etc. Since the readouts from such assays can be triggered prior to the ∼8 to 12 h required for host adaptation, the use of nonadapted bacteria for these in vitro models may not report the cellular and/or immunological responses which occur during the majority of the disease process.
Supplementary Material
Acknowledgments
We are indebted to Francis E. Nano (University of Victoria) and Terry Otto (Immuno-Precise Antibodies, Ltd.) for antibodies/antiserum against MglB, IglC, and IglB; to Daniel L. Clemens (UCLA) for antisera against GroEL, KatG, SodB, and Bfr; to Micheal V. Norgard and Jason F. Huntley (UTSW) for antisera against Tul4A, Mip, Pal, and FopA; and to Eric R. LaFontaine (University of Georgia) for anti-FspA sera. We thank Joseph Mazurkiewicz for electron microscopy as well as James Drake and Robert K. Ernst for critical reviews of the manuscript.
This work was supported by institutional startup funds (K.R.O.H.) and by Public Health Service grants NIH AI056320 (D.W.M., T.J.S., and D.J.L.) and AI057158 (G.S.K.).
Editor: W. A. Petri, Jr.
Footnotes
Published ahead of print on 21 July 2008.
Supplemental material for this article may be found at http://iai.asm.org/.
REFERENCES
- 1.Akins, D. R., K. W. Bourell, M. J. Caimano, M. V. Norgard, and J. D. Radolf. 1998. A new animal model for studying Lyme disease spirochetes in a mammalian host-adapted state. J. Clin. Investig. 1012240-2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baron, G. S., and F. E. Nano. 1998. MglA and MglB are required for the intramacrophage growth of Francisella novicida. Mol. Microbiol. 29247-259. [DOI] [PubMed] [Google Scholar]
- 3.Barthold, S. W., E. Fikrig, L. K. Bockenstedt, and D. H. Persing. 1995. Circumvention of outer surface protein A immunity by host-adapted Borrelia burgdorferi. Infect. Immun. 632255-2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bergstrom, J., P. Furst, L. O. Noree, and E. Vinnars. 1974. Intracellular free amino acid concentration in human muscle tissue. J. Appl. Physiol. 36693-697. [DOI] [PubMed] [Google Scholar]
- 5.Brotcke, A., D. S. Weiss, C. C. Kim, P. Chain, S. Malfatti, E. Garcia, and D. M. Monack. 2006. Identification of MglA-regulated genes reveals novel virulence factors in Francisella tularensis. Infect. Immun. 746642-6655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carlson, P. E., Jr., J. A. Carroll, D. M. O'Dee, and G. J. Nau. 2007. Modulation of virulence factors in Francisella tularensis determines human macrophage responses. Microb. Pathog. 42204-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chamberlain, R. E. 1965. Evaluation of live tularemia vaccine prepared in a chemically defined medium. Appl. Microbiol. 13232-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charity, J. C., M. M. Costante-Hamm, E. L. Balon, D. H. Boyd, E. J. Rubin, and S. L. Dove. 2007. Twin RNA polymerase-associated proteins control virulence gene expression in Francisella tularensis. PLoS Pathog. 3e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cole, L. E., K. L. Elkins, S. M. Michalek, N. Qureshi, L. J. Eaton, P. Rallabhandi, N. Cuesta, and S. N. Vogel. 2006. Immunologic consequences of Francisella tularensis live vaccine strain infection: role of the innate immune response in infection and immunity. J. Immunol. 1766888-6899. [DOI] [PubMed] [Google Scholar]
- 10.Cole, L. E., K. A. Shirey, E. Barry, A. Santiago, P. Rallabhandi, K. L. Elkins, A. C. Puche, S. M. Michalek, and S. N. Vogel. 2007. Toll-like receptor 2-mediated signaling requirements for Francisella tularensis live vaccine strain infection of murine macrophages. Infect. Immun. 754127-4137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collazo, C. M., A. Sher, A. I. Meierovics, and K. L. Elkins. 2006. Myeloid differentiation factor-88 (MyD88) is essential for control of primary in vivo Francisella tularensis LVS infection, but not for control of intra-macrophage bacterial replication. Microbes Infect. 8779-790. [DOI] [PubMed] [Google Scholar]
- 12.Daffertshofer, A., C. J. Lamoth, O. G. Meijer, and P. J. Beek. 2004. PCA in studying coordination and variability: a tutorial. Clin. Biomech. (Bristol, Avon) 19415-428. [DOI] [PubMed] [Google Scholar]
- 13.Deka, R. K., Y. H. Lee, K. E. Hagman, D. Shevchenko, C. A. Lingwood, C. A. Hasemann, M. V. Norgard, and J. D. Radolf. 1999. Physicochemical evidence that Treponema pallidum TroA is a zinc-containing metalloprotein that lacks porin-like structure. J. Bacteriol. 1814420-4423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Silva, A. M., S. R. Telford III, L. R. Brunet, S. W. Barthold, and E. Fikrig. 1996. Borrelia burgdorferi OspA is an arthropod-specific transmission-blocking Lyme disease vaccine. J. Exp. Med. 183271-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eigelsbach, H. T., W. Braun, and R. D. Herring. 1951. Studies on the variation of bacterium tularense. J. Bacteriol. 61557-569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Forestal, C. A., M. Malik, S. V. Catlett, A. G. Savitt, J. L. Benach, T. J. Sellati, and M. B. Furie. 2007. Francisella tularensis has a significant extracellular phase in infected mice. J. Infect. Dis. 196134-137. [DOI] [PubMed] [Google Scholar]
- 17.Golovliov, I., M. Ericsson, G. Sandstrom, A. Tarnvik, and A. Sjostedt. 1997. Identification of proteins of Francisella tularensis induced during growth in macrophages and cloning of the gene encoding a prominently induced 23-kilodalton protein. Infect. Immun. 652183-2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guina, T., D. Radulovic, A. J. Bahrami, D. L. Bolton, L. Rohmer, K. A. Jones-Isaac, J. Chen, L. A. Gallagher, B. Gallis, S. Ryu, G. K. Taylor, M. J. Brittnacher, C. Manoil, and D. R. Goodlett. 2007. MglA regulates Francisella tularensis subsp. novicida (Francisella novicida) response to starvation and oxidative stress. J. Bacteriol. 1896580-6586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hansen, L. K., J. Larsen, F. A. Nielsen, S. C. Strother, E. Rostrup, R. Savoy, N. Lange, J. Sidtis, C. Svarer, and O. B. Paulson. 1999. Generalizable patterns in neuroimaging: how many principal components? Neuroimage 9534-544. [DOI] [PubMed] [Google Scholar]
- 20.Hong, K. J., J. R. Wickstrum, H. W. Yeh, and M. J. Parmely. 2007. Toll-like receptor 2 controls the gamma interferon response to Francisella tularensis by mouse liver lymphocytes. Infect. Immun. 755338-5345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Katz, J., P. Zhang, M. Martin, S. N. Vogel, and S. M. Michalek. 2006. Toll-like receptor 2 is required for inflammatory responses to Francisella tularensis LVS. Infect. Immun. 742809-2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keller, D., F. T. Koster, D. H. Marks, P. Hosbach, L. F. Erdile, and J. P. Mays. 1994. Safety and immunogenicity of a recombinant outer surface protein A Lyme vaccine. JAMA 2711764-1768. [PubMed] [Google Scholar]
- 23.Kirimanjeswara, G. S., J. M. Golden, C. S. Bakshi, and D. W. Metzger. 2007. Prophylactic and therapeutic use of antibodies for protection against respiratory infection with Francisella tularensis. J. Immunol. 179532-539. [DOI] [PubMed] [Google Scholar]
- 24.Lauriano, C. M., J. R. Barker, S. S. Yoon, F. E. Nano, B. P. Arulanandam, D. J. Hassett, and K. E. Klose. 2004. MglA regulates transcription of virulence factors necessary for Francisella tularensis intraamoebae and intramacrophage survival. Proc. Natl. Acad. Sci. USA 1014246-4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee, B. Y., M. A. Horwitz, and D. L. Clemens. 2006. Identification, recombinant expression, immunolocalization in macrophages, and T-cell responsiveness of the major extracellular proteins of Francisella tularensis. Infect. Immun. 744002-4013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lenco, J., M. Hubalek, P. Larsson, A. Fucikova, M. Brychta, A. Macela, and J. Stulik. 2007. Proteomics analysis of the Francisella tularensis LVS response to iron restriction: induction of the F. tularensis pathogenicity island proteins IglABC. FEMS Microbiol. Lett. 26911-21. [DOI] [PubMed] [Google Scholar]
- 27.Loegering, D. J., J. R. Drake, J. A. Banas, T. L. McNealy, D. G. Mc Arthur, L. M. Webster, and M. R. Lennartz. 2006. Francisella tularensis LVS grown in macrophages has reduced ability to stimulate the secretion of inflammatory cytokines by macrophages in vitro. Microb. Pathog. 41218-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malik, M., C. S. Bakshi, B. Sahay, A. Shah, S. A. Lotz, and T. J. Sellati. 2006. Toll-like receptor 2 is required for control of pulmonary infection with Francisella tularensis. Infect. Immun. 743657-3662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mohapatra, N. P., S. Soni, B. L. Bell, R. Warren, R. K. Ernst, A. Muszynski, R. W. Carlson, and J. S. Gunn. 2007. Identification of an orphan response regulator required for the virulence of Francisella spp. and transcription of pathogenicity island genes. Infect. Immun. 753305-3314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oyston, P. C., A. Sjostedt, and R. W. Titball. 2004. Tularaemia: bioterrorism defence renews interest in Francisella tularensis. Nat. Rev. Microbiol. 2967-978. [DOI] [PubMed] [Google Scholar]
- 31.Payne, S. M. 1993. Iron acquisition in microbial pathogenesis. Trends Microbiol. 166-69. [DOI] [PubMed] [Google Scholar]
- 32.Rajan, K. 2005. Materials informatics. Mater. Today 838-45. [Google Scholar]
- 33.Ratledge, C., and L. G. Dover. 2000. Iron metabolism in pathogenic bacteria. Annu. Rev. Microbiol. 54881-941. [DOI] [PubMed] [Google Scholar]
- 34.Santic, M., M. Molmeret, K. E. Klose, S. Jones, and Y. A. Kwaik. 2005. The Francisella tularensis pathogenicity island protein IglC and its regulator MglA are essential for modulating phagosome biogenesis and subsequent bacterial escape into the cytoplasm. Cell. Microbiol. 7969-979. [DOI] [PubMed] [Google Scholar]
- 35.Sigal, L. H., J. M. Zahradnik, P. Lavin, S. J. Patella, G. Bryant, R. Haselby, E. Hilton, M. Kunkel, D. dler-Klein, T. Doherty, J. Evans, P. J. Molloy, A. L. Seidner, J. R. Sabetta, H. J. Simon, M. S. Klempner, J. Mays, D. Marks, S. E. Malawista, et al. 1998. A vaccine consisting of recombinant Borrelia burgdorferi outer-surface protein A to prevent Lyme disease. N. Engl. J. Med. 339216-222. [DOI] [PubMed] [Google Scholar]
- 36.Sjostedt, A. 2006. Intracellular survival mechanisms of Francisella tularensis, a stealth pathogen. Microbes Infect. 8561-567. [DOI] [PubMed] [Google Scholar]
- 37.Steere, A. C., V. K. Sikand, F. Meurice, D. L. Parenti, E. Fikrig, R. T. Schoen, J. Nowakowski, C. H. Schmid, S. Laukamp, C. Buscarino, D. S. Krause, et al. 1998. Vaccination against Lyme disease with recombinant Borrelia burgdorferi outer-surface lipoprotein A with adjuvant. N. Engl. J. Med. 339209-215. [DOI] [PubMed] [Google Scholar]
- 38.Su, J., J. Yang, D. Zhao, T. H. Kawula, J. A. Banas, and J. R. Zhang. 2007. Genome-wide identification of Francisella tularensis virulence determinants. Infect. Immun. 753089-3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Suh, C., A. Rajagopalan, X. Li, and K. Rajan. 2002. The application of principal component analysis to materials science data. Data Sci. J. 119-26. [Google Scholar]
- 40.Sullivan, J. T., E. F. Jeffery, J. D. Shannon, and G. Ramakrishnan. 2006. Characterization of the siderophore of Francisella tularensis and role of fslA in siderophore production. J. Bacteriol. 1883785-3795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Telepnev, M., I. Golovliov, T. Grundstrom, A. Tarnvik, and A. Sjostedt. 2003. Francisella tularensis inhibits Toll-like receptor-mediated activation of intracellular signalling and secretion of TNF-alpha and IL-1 from murine macrophages. Cell. Microbiol. 541-51. [DOI] [PubMed] [Google Scholar]
- 42.Telepnev, M., I. Golovliov, and A. Sjostedt. 2005. Francisella tularensis LVS initially activates but subsequently down-regulates intracellular signaling and cytokine secretion in mouse monocytic and human peripheral blood mononuclear cells. Microb. Pathog. 38239-247. [DOI] [PubMed] [Google Scholar]
- 43.Thakran, S., H. Li, C. L. Lavine, M. A. Miller, J. E. Bina, X. R. Bina, and F. Re. 2008. Identification of Francisella tularensis lipoproteins that stimulate the Toll-like receptor (TLR) 2/TLR1 heterodimer. J. Biol. Chem. 2833751-3760. [DOI] [PubMed] [Google Scholar]
- 44.Twine, S. M., N. C. Mykytczuk, M. D. Petit, H. Shen, A. Sjostedt, C. J. Wayne, and J. F. Kelly. 2006. In vivo proteomic analysis of the intracellular bacterial pathogen, Francisella tularensis, isolated from mouse spleen. Biochem. Biophys. Res. Commun. 3451621-1633. [DOI] [PubMed] [Google Scholar]
- 45.Vasil, M. L., and U. A. Ochsner. 1999. The response of Pseudomonas aeruginosa to iron: genetics, biochemistry and virulence. Mol. Microbiol. 34399-413. [DOI] [PubMed] [Google Scholar]
- 46.Vonkavaara, M., M. V. Telepnev, P. Ryden, A. Sjostedt, and S. Stoven. 2008. Drosophila melanogaster as a model for elucidating the pathogenicity of Francisella tularensis. Cell. Microbiol. 101327-1338. [DOI] [PubMed] [Google Scholar]
- 47.Williams, M. D., T. X. Ouyang, and M. C. Flickinger. 1994. Starvation-induced expression of SspA and SspB: the effects of a null mutation in sspA on Escherichia coli protein synthesis and survival during growth and prolonged starvation. Mol. Microbiol. 111029-1043. [DOI] [PubMed] [Google Scholar]
- 48.Yu, J. J., E. K. Raulie, A. K. Murthy, M. N. Guentzel, K. E. Klose, and B. P. Arulanandam. 2008. The presence of infectious extracellular Francisella tularensis subsp. novicida in murine plasma after pulmonary challenge. Eur. J. Clin. Microbiol. Infect. Dis. 27323-325. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.