Abstract
Purpose
To determine which patient clinical and demographic factors are associated with short-term rate of recovery from arthroscopic partial meniscectomy in the year following surgery and how they differ from previously published associations with long-term outcome.
Methods
Depth of meniscal excision, involvement of one or both menisci, extent of meniscal tear, and extent of osteoarthritis were obtained at surgery, as well as age, BMI, and gender. Mixed model repeated measures analyses were used longitudinally to identify independent predictors of recovery, measured by prospectively assessing knee pain, knee function, and overall physical knee status pre-operatively and at regular intervals throughout postoperative recovery.
Results
Neither advanced age nor increased BMI had any influence on patient recovery over time, while gender was implicated with women having significantly poorer recovery scores than men (P < .04). Additionally, differences in variables indicating extent of meniscal tear and resection did not influence recovery scores over time, and the only surgical factor that impacted all three recovery variables was extent of osteoarthritis (P < .02).
Conclusions
We have shown that female gender and worse osteoarthritis are associated with a slower rate of short-term recovery from arthroscopic partial meniscectomy, while age, obesity, and amount of meniscal tear/resection showed no association with rate of recovery throughout the first year postoperatively.
Level of Evidence
Level I, high-quality prognostic prospective study (all patients were enrolled at the same point in their disease with >80% follow-up of enrolled patients).
Keywords: Knee, Meniscus, Osteoarthritis, Arthroscopy, Recovery, Meniscectomy
Introduction
The American Academy of Orthopedic Surgeons estimates that arthroscopy procedures of the knee total 636,000 cases per year in the United States.1 Patients are often greatly concerned with their short-term recovery in the days and weeks following surgery in addition to how they will fare in the future years ahead. Although there is a new growing interest in short-term recovery from orthopaedic surgery, current literature has stressed the importance of the end result of meniscectomy in the long-term2–14; there appears to be limited empirical evidence regarding immediate recovery following surgical intervention. Surgeons must be able to discuss evidence-based literature with surgical candidates that describe factors influencing short-term recovery.
The variables that affect long-term knee status are not necessarily what will affect the patient postoperatively. Because initial return to function following arthroscopic partial meniscectomy does not require several years, it is vital to identify clinical factors associated with patient rate of recovery in the short-term.
Long-term data are plentiful regarding the impact of surgical and demographic variables on result of meniscectomy. While most have contended that extensive meniscal resection predicts worse radiographic and functional long-term status,2, 3, 5, 8, 12 some researchers report no impact of greater removal.14 Many have supported an association between osteoarthritis at the time of surgery and poor surgical outcome.4, 6, 12, 13 Data regarding medial vs. lateral arthroscopic partial meniscectomy are mixed: although in vitro modeling postulates that lateral partial meniscectomy is more dangerous than medial partial meniscectomy,15 in vivo studies have shown no significant clinical differences.4 It has been shown that younger patient age predicts a better long-term prognosis after meniscectomy,4, 13 while obesity is associated with a worse result.6, 7 Additionally, although gender has not been shown to play a role before postoperative year 15,16, 17, 8 very long-term symptoms and functional limitations are worse in women who have undergone meniscectomy when compared to men13 and women tend to have more osteoarthritis 15 to 22 years after surgery.6 These studies, however, have only analyzed the end result of surgical intervention, and do not address patient recovery in the immediate postoperative period. Few studies have investigated short-term recovery from orthopaedic surgical procedures, and we are aware of no study to date that has reported patient surgical, demographic, and clinical factors influencing postoperative rate of recovery following surgical intervention.
Although it may appear depth of meniscal excision, involvement of both menisci, extent of meniscal tear, and degradation of the articular joint surface would adversely affect patient recovery immediately after surgical intervention as it does in the long-term, there is limited empirical evidence in the literature to support these clinical beliefs. Nor is it known which of these variables is most strongly associated with recovery from surgery, and which show a weak or no association at all. We utilized three physician-rated recovery variables - knee pain, knee function, and overall physical knee status– at baseline and regular intervals postoperatively to assess multiple indices of recovery from arthroscopy.
This study evaluates what factors the surgeon can apply to patients’ concerns regarding postoperative recovery, and how they differ from factors associated with long-term outcome. We hypothesized that depth of meniscal excision, involvement of both menisci, extent of meniscal tear, and degradation of the articular joint surface would all adversely affect postoperative rate of recovery from arthroscopic partial meniscectomy. In addition, relevant patient demographic factors of age, body mass index (BMI), and gender were also analyzed in the statistical model because of their potential impact on recovery.
Methods
One hundred twenty six consecutive arthroscopic partial meniscectomy procedures were performed and prospective data were collected between August 2000 and August 2005 by one surgeon at a major University medical center. Demographic characteristics of patient sample are displayed in (Table 1). All patients were given a preoperative diagnosis of ‘torn medial meniscus,’ ‘torn lateral meniscus,’ or both by history, physical examination, and confirmatory MRI. In addition, inclusion criteria for the study included: ages 16–80 years, no history of injury to either knee that required surgical intervention or produced pain, swelling, mechanical symptoms, and/or activity restriction for greater than six months, no major varus or valgus deformities by clinical examination (estimated as requiring less than three-and-a-half fingerbreadths between medial femoral condyles, no ACL/PCL/LCL/MCL injury, no prior surgical treatment to either knee, no chronic comorbidities that resulted in restricted physical activity (e.g., insulin-dependant diabetes mellitus, severe coronary obstructive pulmonary disease), and not requiring emergency surgery for their injury. Previous knee injury (and treatment) was reported by the patient and confirmed by preoperative MRI. In summary, these were otherwise healthy patients with previously healthy knees who experienced relatively recent onset of knee symptoms caused by meniscal pathology.
Table 1.
Patient Characteristics of One Hundred Twenty Six Arthroscopic Partial Meniscectomy Candidates
| Variable | Value |
|---|---|
| Gender | |
| Male | 78 |
| Female | 48 |
| Race | |
| White | 120 |
| Black | 1 |
| Hispanic | 2 |
| Other | 3 |
| Age (years) | 49.3 ± 10.76 [23–78] |
| BMI | 28.4 ± 5.5 [19.3–47.2] |
| Marital Status | |
| Never Married | 19 |
| Divorced or Widowed | 13 |
| Married | 94 |
| Education (years) | 15.64 ± 1.72 |
| High School | 14 |
| College | 62 |
| Professional School | 50 |
Patients were typically identified 2 to 6 weeks before their surgery, and were screened and recruited by phone once identified by clinical staff as needing arthroscopy for a torn meniscus. All patients underwent arthroscopic partial meniscectomy on one knee. Approval for all procedures was obtained from the University Human Investigations Committee. Participation in this study was completely voluntary, and did not affect delivery of health care in any way.
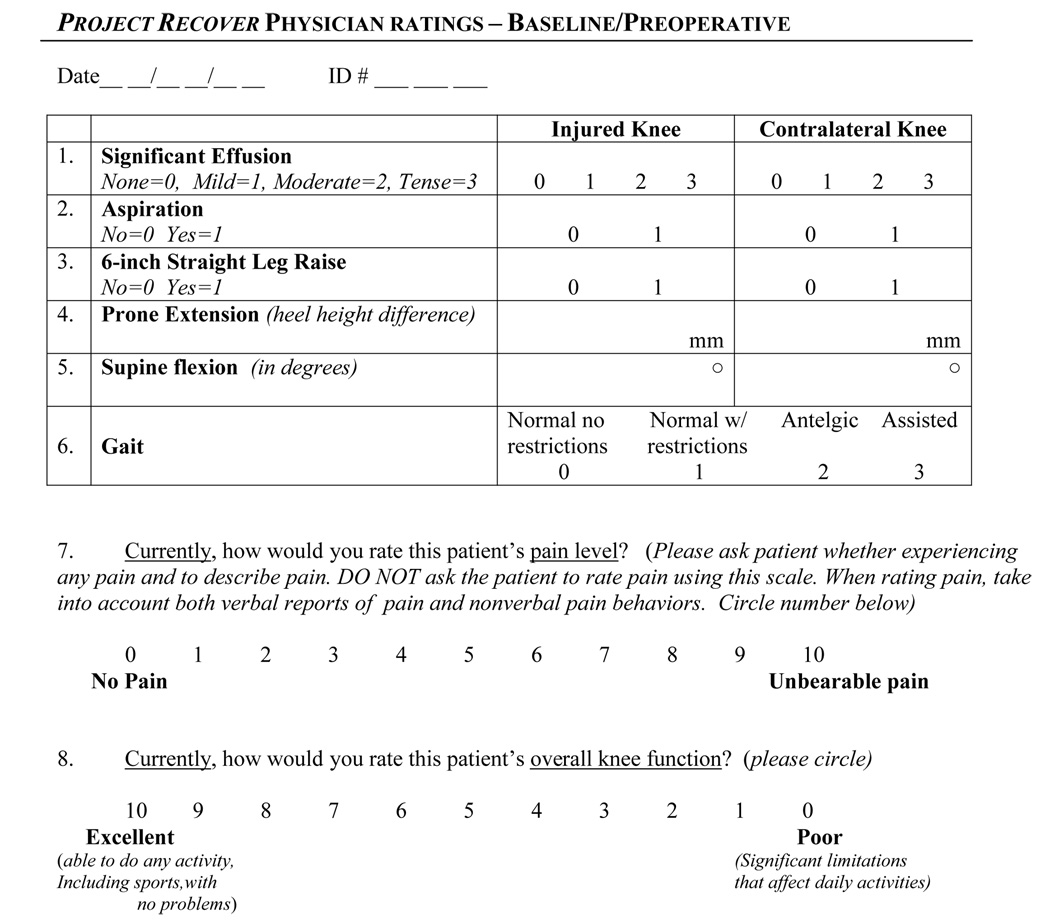
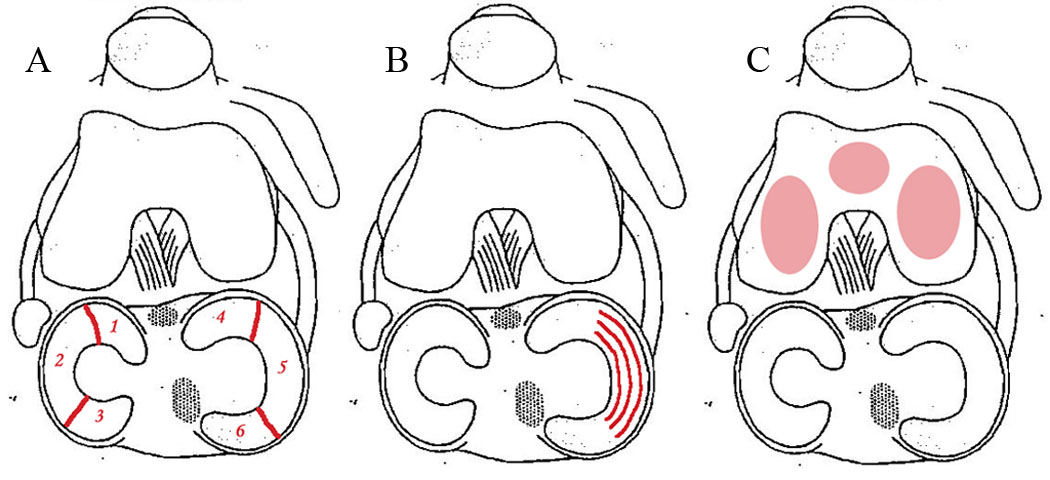
Patient demographic and initial clinical data were collected and measured by nursing staff during the preoperative interview, including age, BMI, and gender; more in-depth past medical and surgical history was collected by the surgeon. Surgical data were collected at the time of surgery by the surgeon (Figure 1a-1c); example intraoperative arthroscopic images are displayed in (Figure 2). Recovery variable data was collected by the surgeon 3–10 days preoperatively, and 1, 3, 8, 16, 24, and 48 weeks postoperatively. All data was collected on a formal data collection form (Figure 3). After meeting study inclusion criteria, 141 patients consented to participate. Fifteen patients (10.6%) were lost to follow-up, leaving 126 patients (89.4% retention) for analysis.
Figure 1.
Surgeon recorded location (A; in any of six clinically significant divisions (“zones”): the anterior horn, body, and posterior horn of each of the lateral and medial menisci) and depth (B; each zone divided into quarters along the width of the meniscus) of meniscus removed, as well as osteoarthritis by modified Outerbridge Score for medial, lateral, and patellar compartments (C).
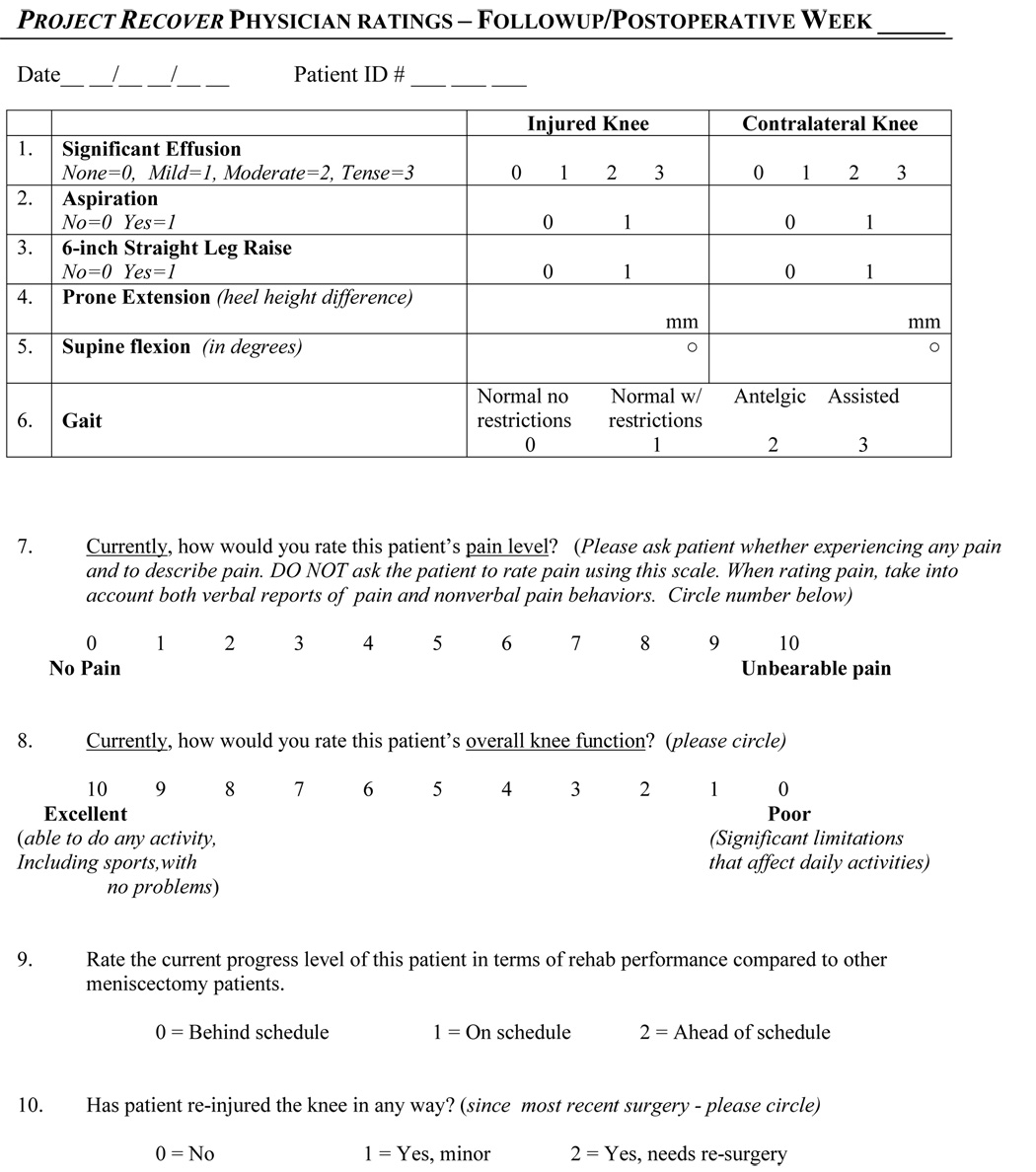
Figure 2.

Intraoperative arthroscopic images showing examples of depth of meniscus removed: 25% (A), 50% (5mm probe shown for scale) (B), and 100% (C).
Figure 3.
Example data scoring sheets used during this study. Data collection forms were designed by epidemiologists and statisticians at a major university hospital.
Because of their impact on end result of surgical intervention as indicated in the literature, the four surgical variables of interest were: depth of meniscal excision, involvement of one or both menisci, extent of meniscal tear, and extent of osteoarthritis. Involvement of one or both (lateral and medial) menisci was recorded. In addition, to determine depth of meniscal excision and extent of meniscal tear, the menisci were divided into six clinically significant divisions (“zones”): the anterior horn, body, and posterior horn of each of the lateral and medial menisci. Depth of meniscal excision was determined as the greatest amount of meniscus removed from any zone. Extent of meniscal tear was designated as the total number of zones involved in the meniscal tear on the worst side (medial or lateral), maximum of three zones. Extent of osteoarthritis was assessed using the Modified Outerbridge articular surface grading (ASG) scale.18 A score for each of the medial, lateral, and patellar joint surfaces by the surgeon at the time of surgery was recorded. The ASG scale score of the most arthritic of the three joint surfaces was used as the final score.
Three measures of physician-rated recovery were obtained at each of the pre-and postoperative time points: knee pain, knee function, and overall physical knee status. The surgeon rated both knee pain and function on a standardized 0 – 10 scale with higher scores reflecting more severe pain and higher knee function. This was done with the patient responding to benchmarks in order to standardize scoring (e.g. score of 0 is no pain, score of 5 is pain interfering with daily activities, and score of 10 is worst pain of patient’s life). This scale has been used extensively to assess both pain and function in a variety of surgical settings, including knee arthroscopy.19–26 Additionally, it has been shown that physician ratings better predict postoperative knee pain and function scores than did patients’ ratings.23 Overall physical knee status included ratings of effusion, extension, flexion, gait, and general progress as determined by the physician at each office visit. Presence of effusion was determined by physical examination. Prone flexion (heel height difference between affected and contralateral legs, in millimeters) and extension were measured in degrees using a goniometer. Normal vs. abnormal gait and general progress were subjective measures determined by the surgeon at each follow-up visit. The five physical status variables were assessed individually as described above. In order to illustrate a general idea of patient status at each followup visit, a dichotomized score of normal/abnormal was generated for each variable, and a summary score was calculated, with 0 indicating normal ratings across all five variables and 5 indicating abnormal ratings across all five. Examples of ‘abnormal’ ratings include presence of effusion, difference in flexion/extension between affected and unaffected knees, and abnormal gait (i.e. observed limp and/or loss of range of motion that visibly interfered with gait). This summation variable, in addition to the standardized variables of pain and function described above were used as the three postoperative recovery variables of interest.
Three mixed model repeated measures analyses were run to identify independent surgical predictors of recovery. This analytic approach allows use of all available data from all patients, and is able to analyze several independent variables separately (while controlling for all other independent variables) over an entire window of time rather than at a single specific endpoint. Additionally, the mixed model repeated measures analysis design is a ‘within-subject’ design which inherently has greater statistical power than a ‘between-subject’ design.27 Adequate patient sample size (power) was confirmed within the mixed model repeated measures analyses. The variables included in each analysis were as follows: the four surgical variables (depth of meniscal excision, involvement of one or both menisci, extent of meniscal tear, and extent of osteoarthritis), and three demographic variables (age, gender, and BMI). Three mixed model analyses were run, and the three physician-rated recovery variables of knee pain, knee function, and overall physical knee status were included, respectively, as the dependent variables.
Results
Tear characteristics, including incidence of one vs. both menisci, number of zones involved, and depth of meniscal excision are shown in (Table 2). Distribution of Modified Outerbridge scores are shown in (Table 3); intercorrelations between the four surgical predictor variables are displayed in (Table 4).
Table 2.
Frequency of Severity of Patient Knee Pathology and Depth of Meniscal Excision
| One vs. Both Menisci | Number of Zones | Involved (max 6) | Depth of Meniscal Excision (max 100%) |
|---|---|---|---|
| 1 Zone | 76 | ||
| One Meniscus: 87 | 2 Zones | 31 | 25% :37 |
| Both Menisci: 39 | 3 Zones | 14 | 50% :60 |
| 4 Zones | 3 | 75% :27 | |
| 5 Zones | 2 | 100% :2 | |
| 6 Zones | 0 | ||
| (126 Total) | (126 Total) | (126 Total) | |
Table 3.
Distribution of Modified Outerbridge Scores
| Score | Frequency |
|---|---|
| 0 | 14 |
| 1 | 16 |
| 2 | 45 |
| 3 | 40 |
| 4 | 11 |
| (Total: 126) | |
Table 4.
Intercorrelations Among Surgical Predictor Variables
| ASG | Depth of Meniscal Excision | One/Both Menisci | |
|---|---|---|---|
| Depth of Meniscal Excision | 0.042 | ||
| One or Both Menisci Involved | 0.108 | 0.217* | |
| Extent of Meniscal Involvement | 0.192* | 0.471*** | 0.408*** |
Pearson correlation values demonstrating intercorrelations between each of the surgical predictor variables.
p ≤ 0.05
p ≤0.001
Results of the mixed model repeated measures analyses are shown in (Table 5). Of the demographic variables, gender was significantly associated with rate of improvement in knee pain, knee function, and overall physical knee status over time (P = 0.04, P = 0.01, P = 0.01) respectively. Age and BMI were not were not predictive of recovery in any of the three models (P > 0.05). Time was also included in the model as a factor to confirm that recovery scores would improve linearly over time during recovery (P = .001 for all analyses).
Table 5.
Summary of Mixed Model Repeated Measures Analyses Examining Influence of Predictor Variables on Recovery Over the Recovery Period
| Predictor Variable | Recovery Variable | |||||
|---|---|---|---|---|---|---|
| Pain | Function | Overall Physical Knee Status | ||||
| Parameter Estimate | T Value | Parameter Estimate | T Value | Parameter Estimate | T Value | |
| Modified Outerbridge ASG Score | 0.29 | 2.64** | −0.32 | −0.28 ** | 0.15 | 2.37* |
| Depth of Meniscal Excision | −0.08 | −0.81 | 0.03 | 0.3 | −0.25 | −0.46 |
| One vs. Both Menisci | −0.14 | −0.75 | 0.04 | 0.19 | 0.10 | 0.94 |
| Extent of Meniscal Tear | 0.24 | 1.6 | −0.25 | −1.6 | 0.17 | 2.14* |
| Gender | 0.38 | 2.13* | −0.49 | −0.26** | 0.25 | 2.59** |
| Age | 0.00 | 0.37 | 0.00 | −0.09 | 0.00 | −0.51 |
| Body Mass Index (BMI) | −0.01 | −0.44 | 0.01 | 0.41 | 0.02 | 1.94 |
| Time | −0.04 | 99.55*** | 0.05 | 17.73*** | −0.02 | −9.69*** |
p ≤0.05
p ≤0.01
p ≤0.001
The first mixed model repeated measures analysis investigating the association of the surgical predictor variables with postoperative physician-rated knee pain revealed that extent of osteoarthritis was significantly associated with rate of recovery (P = 0.01). Depth of meniscal excision, involvement of one or both menisci, and extent of meniscal tear, however, were not associated with rate of recovery with regard to knee pain. The second mixed model repeated measures analysis analyzed the impact of the surgical predictor variables on physician-rated postoperative knee function. Again, this analysis revealed an overall main effect for extent of osteoarthritis (P = 0.01), supporting that greater osteoarthritis was associated with lower knee function postoperatively over time. Depth of meniscal excision, involvement of one or both menisci, and extent of meniscal tear were not associated with rate of improvement in knee function. Finally, the third mixed model repeated measures analysis investigating the influence of the surgical variables on overall physical knee status revealed that both extent of osteoarthritis (P = 0.02) and extent of meniscal tear (P = 0.04), were significantly associated with rate of improvement of overall physical knee status over the recovery period. Depth of meniscal excision and involvement of one or both menisci were not associated with rate of recovery with regard to patients’ overall physical knee status score. These results are summarized alongside previously mentioned long-term outcome data in (Table 6).
Table 6.
Long and Short Term Predictors of Poor Outcome/Recovery
| Predictor Variable | Effects on Postoperative Recovery (This Study) | Effects on Long-Term Outcome (Literature) |
|---|---|---|
| Depth of Meniscal Excision | No Association | Significant Predictor of Poor Outcome |
| Involvement of One or Both Menisci | No Association | No Literature Available at This Time |
| Extent of Meniscal Tear | No Association | No Literature Available at This Time |
| Extent of Osteoarthritis | Significant Predictor of Poor Recovery Scores | Significant Predictor of Poor Outcome |
| Age | No Association | Significant Predictor of Poor Outcome |
| Obesity/BMI | No Association | Significant Predictor of Poor Outcome |
| Female Gender | Significant Predictor of Poor Recovery Scores | Significant Predictor of Poor Outcome |
Discussion
Currently, physicians are forced to advise patients regarding their short-term recovery based on anecdotal evidence from their own experience, including intuitions about how patients will recover based on their age, weight, incentive to recover, amount of tissue resected, and amount of physical therapy they receive, rather than being able to refer to published data. While one previous study reported general information concerning when patients could return to work, school, or daily activity to show that arthroscopy is reliable and cost effective with rapid return of good knee function,28 it did not discuss specific factors that would influence patient recovery time and/or return to everyday activities. Similarly, some describe the effectiveness of supervised physical therapy for recovery from arthroscopic partial meniscectomy,29 while others have asserted that postoperative recovery with supervised physical therapy was no better than independent home physical therapy.10
The present study sought to determine which patient variables are associated with rate of recovery from surgery after arthroscopic partial meniscectomy by examining the influence of four surgical variables on postoperative recovery over time: depth of meniscal excision, involvement of one or both menisci, extent of meniscal tear, and extent of osteoarthritis. Using these results, physicians can inform their patients that even though they are older or must have a large amount of tissue resected, this will not affect their recovery when compared to other patients undergoing arthroscopic partial meniscectomy. Conversely, they can notify patients with significant osteoarthritis that even though they have a small meniscal tear, they may have poorer postoperative recovery than someone without significant OA changes despite the small amount of tissue that needs to be resected, and may elect for nonoperative management.
Interestingly, the extent of meniscal tear affected only overall physical knee status, but not knee pain or function, while depth of meniscal excision and involvement of one or both menisci had no impact on any aspect of recovery. This is contrasted by studies that have shown that increased meniscal tear and/or greater amount of meniscal tissue excision have resulted in poorer outcome.2, 3, 5 Of the surgical predictor variables, only extent of osteoarthritis was predictive of recovery across all three recovery variables (knee pain, knee function, and overall physical knee status), with worse osteoarthritis negatively impacting the rate of recovery across all three recovery variables significantly. It is possible that these results may be explained by the aneural nature of meniscal tissue. Thus although greater extent of meniscal tear may impact overall physical knee status variables (such as flexion, extension, etc.) throughout the recovery period, knee pain and function are not impacted by extent of meniscal tear during the year after surgery. Variables that have been shown to affect long-term patient status cannot necessarily be generalized to implicate similar associations when considering short-term recovery from surgery.
Of the demographic and clinical variables included in our model, patient age and BMI were not associated with any postoperative recovery variable over time, although older patient age4, 13 and obesity6, 7 have been shown to be associated with worse long-term result. Beginning preoperatively, women had greater knee pain, worse knee function, and poorer overall physical knee status than men. Postoperatively, these differences continued, with women continuing to show delayed recovery across all three recovery variables throughout the postoperative year. These findings are consistent with results of previous research reporting worse long-term knee status in women.6, 13
While depth of meniscal excision, involvement of one or both menisci, and extent of meniscal tear were not associated with poorer scores across all three postoperative recovery variables, extent of osteoarthritis as assessed by Modified Outerbridge articular surface grading was the only surgical variable that predicted how a patient would recover from arthroscopic partial meniscectomy. In a multirater, multicenter agreement study of articular cartilage grading, arthroscopic grading of articular cartilage was reliably assessed across surgeons and centers.30 Not only can osteoarthritis be reliably assessed, but the present study supports that it has important implications for recovery: worse osteoarthritis as graded arthroscopically by the surgeon indicates poorer patient recovery from arthroscopic partial meniscectomy.
In a randomized control trial determining the effectiveness of treating osteoarthritis with arthroscopic debridement, arthroscopic lavage with or without debridement was no better than placebo for treatment of advanced osteoarthritis of the knee.31 Since patients with severe osteoarthritis already have extensive loss of cartilage and soft tissue, our study attests that further soft tissue removal appears to have minimal impact on patient knee pain and regaining function in the short-term.
Notable strengths of this study are the prospective longitudinal design and the specific patient population, with all patients enrolled at the same time in their disease. Less than 10% of patients were lost to follow-up. This classifies the data as meeting stage I criteria. Also, mixed model repeated measures analyses were used to determine how the predictor variables were associated with recovery over the entire recovery period, rather than predicting knee status at a single specific timepoint.
Because patients are interested in the practical aspects of short-term recovery, that is, when will they be pain-free and thus able to return to work, sports, leisure time activities, and activities of daily living, identifying the surgical and demographic variables associated with short-term recovery has great practical significance for the orthopaedic surgeon. This study opens the door for future research to determine what variables are associated with short-term recovery from orthopaedic procedures other than arthroscopic partial meniscectomy. By allowing the patient to be able to better know and understand their likely timeline for recovery from arthroscopic partial meniscectomy, “the process of shared medical decision making between patient and clinician becomes much more informed, educated, and confident.”23
One limitation of this study is that the recovery variables used differ from the outcome variables used in the previously mentioned studies, thus presenting a possible concern of confounding differences. In addition the study population, although representative of the university in which this study took place, is not representative of the average population. Patients were largely drawn from a university community; the population was not ethnically diverse (5% ethnic minorities) and included mostly a highly educated patient base (88% were educated through college or graduate/professional school).
Conclusion
We have shown that female gender and worse osteoarthritis are associated with a slower rate of recovery from arthroscopic partial meniscectomy, while age, body mass index, depth of meniscal excision, involvement of one or both menisci, and extent of meniscal tear showed no association throughout the first year postoperatively.
Acknowledgements
Funding for this research came from the National Institute of Arthritis and Musculoskeletal and Skin Disorders (NIAMS) (No. R01 AR46299). Additional funding was contributed by the Felix Freshwater Student Research Fellowship. The Authors would also like to acknowledge Dr. Michael Medvecky for contributing example intraoperative arthroscopic images for this manuscript (Figure 2).
Supported by outside funding or grant(s) from the National Institute of Arthritis and Musculoskeletal and Skin Disorders (NIAMS) (No. R01 AR46299). Additional funding was contributed by the Felix Freshwater Student Research Fellowship.
One or more of the researchers or an affiliated institute _N/A_ **(supply specific name(s)/initials or enter "N/A")** has received (or agreed to receive) from a commercial entity something of value (exceeding the equivalent of US$500) related in any way to this manuscript or research. ***Enter "N/A" or supply the name(s) of the commercial entity(ies)*** _N/A_.
Research was performed at Yale University School of Medicine.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors wish to report that there is no conflict of interest.
References
- 1.Praemer A, Furner S, Rice DP. Musculoskeletal Conditions in the United States. Illinois: American Academy of Orthopaedic Surgeons; 1999. [Google Scholar]
- 2.Andersson-Molina H, Karlsson H, Rockborn P. Arthroscopic partial and total meniscectomy: A long-term follow-up study with matched controls. Arthroscopy. 2002;18:183–189. doi: 10.1053/jars.2002.30435. [DOI] [PubMed] [Google Scholar]
- 3.Bonneux I, Vandekerckhove B. Arthroscopic partial lateral meniscectomy long-term results in athletes. Acta Orthop Belg. 2002;68:356–361. [PubMed] [Google Scholar]
- 4.Chatain F, Adeleine P, Chambat P, Neyret P. A comparative study of medial versus lateral arthroscopic partial meniscectomy on stable knees: 10-year minimum follow-up. Arthroscopy. 2003;19:842–849. doi: 10.1016/s0749-8063(03)00735-7. [DOI] [PubMed] [Google Scholar]
- 5.Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum. 2003;48:2178–2187. doi: 10.1002/art.11088. [DOI] [PubMed] [Google Scholar]
- 6.Englund M, Lohmander LS. Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum. 2004;50:2811–2819. doi: 10.1002/art.20489. [DOI] [PubMed] [Google Scholar]
- 7.Harrison M, Morrell J, Hopman WM. Influence of obesity on outcome after knee arthroscopy. Arthroscopy. 2004;20:691–695. doi: 10.1016/j.arthro.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Higuchi H, Kimura M, Shirakura K, Terauchi M, Takagishi K. Factors affecting long-term results after arthroscopic partial meniscectomy. Clin Orthop. 2000:161–168. doi: 10.1097/00003086-200008000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Jager A, Starker M, Herresthal J. Can meniscus refixation prevent early development of arthrosis in the knee joint? Long-term results. Zentralblatt fur Chirurgie. 2000;125:532–535. [PubMed] [Google Scholar]
- 10.Jokl P, Stull PA, Lynch JK. Independant Home Versus Supervised Rehabilitation Following Arthroscopic Knee Surgery - A Prospective Randomized Trial. Arthroscopy. 1989;5:298–305. doi: 10.1016/0749-8063(89)90145-x. [DOI] [PubMed] [Google Scholar]
- 11.Menterey J, Siegrist O, Fritschy D. Medial meniscectomy in patients over the age of fifty: a six year follow-up study. Swiss Surgery. 2002;8:113–119. doi: 10.1024/1023-9332.8.3.113. [DOI] [PubMed] [Google Scholar]
- 12.Meredith D, Losina E, Mahomed NN, Wright J, Katz JN. Factors predicting functional and radiographic outcomes after arthroscopic partial meniscectomy: a review of the literature. Arthroscopy. 2005;21:211–223. doi: 10.1016/j.arthro.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 13.Roos E, Ostenberg A, Roos H, Ekdahl C, Lohmander LS. Long-term outcome of meniscectomy: symptoms, function, and performance tests in patients with or without radiographic osteoarthritis compared to matched controls. Osteoarthritis & Cartilage. 2001;9:316–324. doi: 10.1053/joca.2000.0391. [DOI] [PubMed] [Google Scholar]
- 14.Shelbourne K, Carr DR. Meniscal repair compared with meniscectomy for bucket-handle medial meniscal tears in anterior cruciate ligament-reconstructed knees. Am J Sports Med. 2003;31:718–723. doi: 10.1177/03635465030310051401. [DOI] [PubMed] [Google Scholar]
- 15.Pena E, Calvo B, Martinez MA, Palanca D, Doblare M. Why lateral meniscectomy is more dangerous than medial meniscectomy. A finite element study. J Orthop Res. 2006;24:1001–1010. doi: 10.1002/jor.20037. [DOI] [PubMed] [Google Scholar]
- 16.Burks R, Metcalf MH, Metcalf RW. Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy. 1997;13:673–679. doi: 10.1016/s0749-8063(97)90000-1. [DOI] [PubMed] [Google Scholar]
- 17.Faunø P, Nielsen AB. Arthroscopic partial meniscectomy: A long-term follow-up. Arthroscopy. 1992;8:345–349. doi: 10.1016/0749-8063(92)90066-k. [DOI] [PubMed] [Google Scholar]
- 18.Cameron M, Briggs KK, Steadman JR. Reproducibility and Reliability of the Outerbridge Classification for Grading Chondral Lesions of the Knee Arthroscopically. Am J Sports Med. 2003;31:83–86. doi: 10.1177/03635465030310012601. [DOI] [PubMed] [Google Scholar]
- 19.Barrett G, Rook RT, Nash CR, Coggin MR. The Effect of Workers' Compensation on Clinical Outcomes of Arthroscopic-Assisted Autogenous Patella Tendon Anterior Cruciate Ligament Reconstruction in the Acute Population. Arthroscopy. 2001:132–137. doi: 10.1053/jars.2001.21785. [DOI] [PubMed] [Google Scholar]
- 20.Capdevila X, Barthlet Y, Biboulet P, Ryckwaert Y, Rubenovitch J, D'Athis F. Effects of Perioperative Analgesic Technique on the Surgical Outcome and Duration of Rehabilitation After Major Knee Surgery. Anesthesiology. 1999:8–15. doi: 10.1097/00000542-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Flandry F, Hunt JP, Terry GC, Hughston JC. Analysis of Subjective Knee Complaints using Visual Analog Scales. Am J Sports Med. 1991:112–118. doi: 10.1177/036354659101900204. [DOI] [PubMed] [Google Scholar]
- 22.Gatt C, Parker RD, Tetzlaff JE, Szabo MZ, Dickerson AB. Preemptive analgesia: Its Role and Efficacy in Anterior Cruciate Ligament reconstruction. Am J Sports Med. 1998;26:524–529. doi: 10.1177/03635465980260040901. [DOI] [PubMed] [Google Scholar]
- 23.Rosenberger P, Jokl P, Cameron A, Ickovics JR. Shared decision making, preoperative expectations, and postoperative reality: differences in physician and patient predictions and ratings of knee surgery outcomes. Arthroscopy. 2005;21:562–569. doi: 10.1016/j.arthro.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 24.Scoggin J, Mayfield G, Awaysa DJ, Pi M, Prentiss J, Takehashi J. Subacromial and Intra-Articular Morphine Versus Bupivicaine After Shoulder Arthoroscopy. Arthroscopy. 2002:464–468. doi: 10.1053/jars.2002.29895. [DOI] [PubMed] [Google Scholar]
- 25.Scott J, Huskisson EC. Graphic Representation of Pain. Pain. 1976:175–184. [PubMed] [Google Scholar]
- 26.Wang J, Ho ST, Lee SC, Tang JJS, Liaw WJ. Intraarticular TriamcinoloneAcetonide for Pain Control After Arthoroscopic Knee Surgery. Anesth Analg. 1998:1113–1116. doi: 10.1097/00000539-199811000-00024. [DOI] [PubMed] [Google Scholar]
- 27.Bryk A, Raudenbush SW. Application of Hierarchical Linear-Models to Assessing Change. Psychol Bull. 1987;101:147–158. [Google Scholar]
- 28.Umar M. Ambulatory arthroscopic knee surgery results of partial meniscectomy. JPMA. 1997;47:210–213. [PubMed] [Google Scholar]
- 29.Goodwin P, Morrissey MC. Supervised physiotherapy after arthroscopic partial meniscectomy: is it effective? Br J Sports Med. 2005;39:692. doi: 10.1136/bjsm.2004.016790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marx R, Connor J, Lyman S, Amendola A, Andrish JT, Kaeding C, McCarty EC, Parker RD, Wright RW, Spindler KP. Multirater Agreement of Arthroscopic Grading of Knee Articular Cartilage. Am J Sports Med. 2005;33:1654–1657. doi: 10.1177/0363546505275129. [DOI] [PubMed] [Google Scholar]
- 31.Moseley B, O'Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, Hollingsworth JC, Ashton CM, Wray NP. A Controlled Trial of Arthroscopic Surgery For Osteoarthritis of the Knee. N Engl J Med. 2002;347:81–88. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]