Abstract
Objective:
To perform a systematic review to determine the healing time of the lateral ankle ligaments after an acute ankle sprain.
Data Sources:
We identified English-language research studies from 1964 to 2007 by searching MEDLINE, Physiotherapy Evidence Database (PEDro), SportDiscus, and CINAHL using the terms ankle sprain, ankle rehabilitation, ankle injury, ligament healing, and immobilization.
Study Selection:
We selected studies that described randomized, controlled clinical trials measuring ligament laxity either objectively or subjectively immediately after injury and at least 1 more time after injury.
Data Extraction:
Two reviewers independently scored the 7 studies that met the inclusion criteria. Because of differences in study designs, a meta-analysis could not be performed. Effect sizes and confidence intervals could be calculated only for 1 study. The percentages of subjective and objective instability were calculated for the remaining studies.
Data Synthesis:
Ankle laxity improved over a period of 6 weeks to 1 year. One author showed stress talar tilt values of 16.10 ± 8.8° immediately after injury and 3.4 ± 3.6° at 3 months after injury. In 2 articles, the authors reported that positive anterior drawer tests were still present in 3% to 31% of participants at 6 months after injury. Additionally, feelings of instability affected 7% to 42% of participants up to 1 year after injury.
Conclusions/Recommendations:
In the studies that we examined, it took at least 6 weeks to 3 months before ligament healing occurred. However, at 6 weeks to 1 year after injury, a large percentage of participants still had objective mechanical laxity and subjective ankle instability. Direct comparison among articles is difficult because of differences in methods. More research focusing on more reliable methods of measuring ankle laxity is needed so that clinicians can know how long ligament healing takes after injury. This knowledge will help clinicians to make better decisions during rehabilitation and for return to play.
Keywords: rehabilitation, tissue healing, laxity
Key Points.
The amount of time needed for ligament healing after ankle sprain is unknown.
Significant improvements in mechanical stability did not occur until at least 6 weeks to 3 months after injury, but a moderate percentage of participants still had objective mechanical laxity and subjective ankle instability.
Objective assessment of mechanical laxity immediately after an ankle sprain and for at least 1 year after injury is needed so clinicians can know how long to protect and immobilize an ankle after sprain, develop rehabilitation protocols to help stabilize the ankle, and make return-to-play decisions based on stability of the ankle ligaments, preventing further injury and damage.
Lateral ankle sprains are among the most common injuries that individuals experience during athletic or recreational activities. Specifically, more than 23 000 ankle sprains are estimated to occur each day in the United States, equating to approximately 1 sprain per 10 000 people daily.1 Even more concerning than the initial ankle sprain is the large percentage (as many as 70%)2 of patients who have repetitive ankle sprains and chronic symptoms after the initial injury. The development of repetitive ankle sprains and persistent symptoms after injury has been termed chronic ankle instability (CAI).3 Chronic ankle instability not only limits physical activity but also can lead to articular degeneration of the ankle joint and an increased risk of osteoarthritis.4
With the large percentage of patients developing CAI, researchers during the past 40 years have tried to determine why an ankle sprain often continues to affect the patient. When examining the potential causes of CAI, Hubbard et al5 reported that mechanical laxity was the largest predictor of the development of CAI, explaining 31.3% of the variance with CAI group membership in their study. Additionally, numerous investigators have reported increased ligamentous laxity in individuals with CAI.5–8 This mechanical laxity may be present because of incomplete healing of the ankle ligaments. The anterior talofibular ligament (ATFL) is reported to be the weakest and the first ligament injured with an ankle sprain.9 Injury to the ATFL typically is followed by injury to the calcaneofibular ligament (CFL) and the posterior talofibular ligament.9 Rupture of the ATFL occurs as an isolated injury in 66% of all ruptures of the ankle ligaments and occurs in combination with a rupture of the CFL in another 20%.9 Because of the damage to these ligaments, an associated increase in the motion present between the talocrural and subtalar joint occurs (hypermobility).
Authors of several studies have reported increased mechanical laxity with damage to the lateral ligaments of the ankle.10–14 Kovaleski et al10 reported an increase in anterior displacement and in inversion-eversion of the ankle with sectioning of the ATFL and CFL compared with an intact condition. They also reported an increase in anterior displacement with sectioning of the ATFL alone compared with an intact condition. Bahr et al11 reported small but observable laxity changes with sectioning of the ATFL alone, but they observed changes in laxity with sectioning of the ATFL and CFL. In similar studies, investigators also have reported increased laxity after sectioning of the ATFL alone and of the ATFL combined with the CFL.12–14 These studies demonstrated that damage to the ATFL and CFL results in increased mechanical laxity. If left untreated, this increased mechanical laxity may lead to the development of CAI.
Management of acute ankle sprains typically involves rest, ice, compression, elevation, and functional rehabilitation. In more severe cases, the ankle normally is immobilized for a few days, and the patient must use crutches to avoid bearing weight on the injured ankle.15 However, McKay et al2 reported that 55% of individuals who sprain their ankles do not seek treatment from a health care professional and concluded that this may be why the ligaments of the ankle do not heal appropriately. If patients seek treatment after acute ankle sprains, they may receive immobilization and crutches and may be referred for further care and rehabilitation. If they do not receive care, they may not protect the joint to enable ligament healing to occur or may not perform rehabilitation. Rehabilitation is necessary to enable the newly replaced collagen to align with the stresses and forces applied at the ankle.15 Additionally, patients typically return to activity within 4 weeks after injury.15 In primate studies, investigators have reported that the tensile strength of ligament tissue is within 80% of normal preinjury strength at 12 months after injury.16 Therefore, most patients with ankle sprains are not performing rehabilitation, and those who are may be returning to exercise or physical activity well before the ligaments have undergone appropriate tissue healing. If patients return to activity before the ligaments have fully healed, the ligament may heal in an elongated state.17 This elongated ligament state could result in increased joint movement (mechanical laxity), which may lead to the development of CAI.
With these questions about ankle sprain rehabilitation and return to activity, numerous investigators have assessed the efficacy of rehabilitation techniques in improving clinical outcomes after a lateral ankle sprain.18–20 This research primarily has focused on short-term outcomes, including pain, range of motion, and return to work or activity. Although determining short-term outcomes is important, the bigger question is, “How long does it take for the ligaments to heal?” Researchers have suggested that ligament damage and mechanical laxity at the ankle joint are related.10–14 If ligament healing is occurring, the ankle should become more mechanically stable. Two methods can be used to assess ligament healing: direct and indirect. Direct methods commonly are used in animal studies. These typically involve damaging a ligament and then measuring markers of healing (inflammatory markers and proteins) or testing tensile strength of ligamentous tissues.16 These procedures are highly invasive and difficult to perform on human participants. Indirect techniques can be used clinically on human participants to quantify mechanical laxity. These are performed with manual stress tests (anterior drawer test), stress radiographs, or arthrometry. Obviously, the limitation is that they are not directly measuring ligament healing but are measuring mechanical laxity. However, based on the research discussed,10–14 we can use these clinical tests to infer indirectly that the ligaments are healing. When ankle mechanical laxity is determined, rehabilitation plans and return-to-play decisions can be made to enable ligament healing to occur. Therefore, the purpose of our study was to perform a systematic review to determine mechanical laxity of the lateral ankle ligaments after an acute lateral ankle sprain.
Data Sources
We searched databases, including MEDLINE, Physiotherapy Evidence Database (PEDro), SportDiscus, and CINAHL, to identify English-language studies from 1964 to 2007 of acute lateral ankle sprain treatment. Terms used were ankle sprain, ankle rehabilitation, ankle injury, ligament healing, and immobilization.
Research specific to treatment outcomes after an acute lateral ankle sprain was identified. To be included in our review, studies had to be randomized, controlled clinical trials that measured lateral ankle mechanical laxity immediately after injury and at least once more after the initial measurement. The initial search resulted in 147 articles. We read all abstracts to determine if the articles could be included in the review. If the abstract was unclear, we read the full article. The references of the identified articles were examined to identify additional articles that may have been missed during the original search. Our search resulted in 7 articles that met the inclusion criteria. We separated them into 2 categories: (1) studies that measured mechanical laxity with objective clinical tests to infer ligament healing (6 articles) and (2) studies that subjectively measured mechanical laxity (1 article).
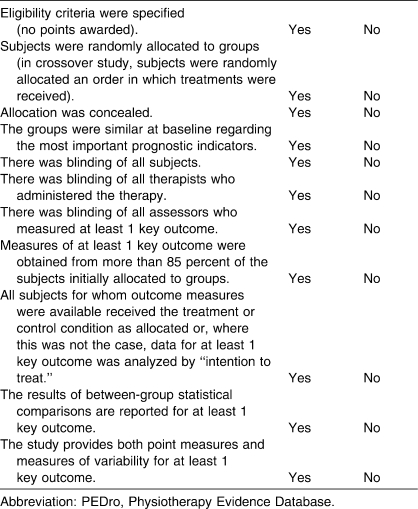
PEDro Scale
The PEDro Scale is an evaluation instrument developed for the Physiotherapy Evidence Database by the Centre for Evidence-Based Physiotherapy.21 The database provides access to controlled clinical trials and systematic reviews in physiotherapy. The trials in the database are rated for quality to help users identify studies of highest methodologic quality. We used the PEDro Scale to determine the methodologic quality of the 7 articles reviewed for our study. The PEDro Scale is a checklist that examines the “believability” (internal validity) and the “interpretability” of trial quality. The Scale “grades” the believability of a research report by considering aspects of study design, such as random allocation; concealment of allocation; comparability of groups at baseline; blinding of patients, therapists, and assessors; analysis by intention to treat; and adequacy of follow-up.22 The Scale measures the interpretability of the trials by examining between-groups statistical comparisons and descriptions of both point estimates and measures of variability. The 11-item checklist yields a maximum score of 10 points if all criteria are satisfied (no points are awarded for the first criterion).22 Table 1 lists the criteria that must be satisfied for a study to receive points on the PEDro Scale. We used the PEDro Scale to evaluate the 7 randomized, controlled trials that met the criteria of examining mechanical stability. Each of us independently reviewed and scored all 7 articles, then we met to discuss scores and findings. Full consensus was achieved over the scores given to the articles.
Table 1.
PEDro Scale21
Data Synthesis
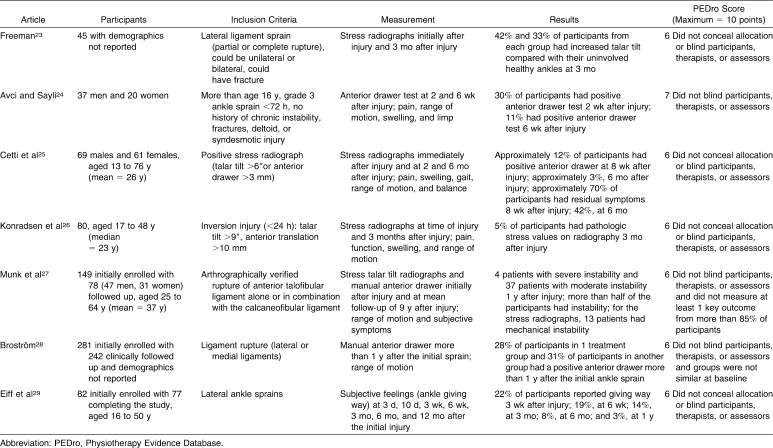
Scores on the PEDro Scale ranged from 6 to 7 of a maximum of 10 points (Table 2). In all 7 studies, ankle mechanical laxity improved over a period of 6 weeks to 1 year. One author23 showed stress talar tilt values of 16.10 ± 8.8° immediately after injury and 3.4 ± 3.6° at 3 months after injury (95% CI = 9.2, 16.2). Strong effect sizes, ranging from 1.47 to 1.72, were reported. In 2 articles,25,28 we noted that positive anterior drawer tests were still present in 3% to 31% of participants at 6 months after injury. In 3 other articles,27–29 from 7% to 42% of participants reported feelings of instability up to 1 year after injury.
Table 2.
Reviewed Articles
In the first group of studies, the researchers objectively measured mechanical laxity through manual stress tests or stress radiographs. One of the original studies on mechanical laxity was performed by Freeman.23 In that study, participants had partial or complete ruptures of the lateral ligaments of the ankle. They were placed into treatment groups based on the type of immobilization that they received. The investigator measured mechanical laxity with talar tilt stress radiographs. Stress radiographs were performed under general anesthesia or regional analgesia. A positive talar tilt was defined as an inversion tilt of the talus of 6° or more on the affected side when compared with the unaffected ankle. This was the only study in which effect sizes could be calculated. Mean talar tilt values were 13.5° in the group receiving mobilization and 17.8° in the group receiving immobilization for 6 weeks. After 3 months, the talar tilt angle decreased to an average of 3.58° and 3.05°, respectively.23 Strong effect sizes, ranging from 1.47 to 1.72, were calculated before and after treatment. Effect sizes helped the researcher determine the clinical significance. Based on the effect sizes, Freeman23 was confident that the immobilization used in the study significantly helped mechanical laxity. Although mechanical laxity did improve over 3 months, 42% of participants receiving mobilization and 33% of participants receiving immobilization for 6 weeks had increased talar tilt compared with their uninvolved healthy ankles at 3 months.
Avci and Sayli24 measured anterior drawer at 2 weeks and again at 6 weeks after an acute lateral ankle sprain. To participate in the study, individuals had to have a positive anterior drawer test, pain in the anterior talofibular ligament, and lateral hematoma. They classified these participants as having a grade 3 inversion ligament injury. Individuals were excluded if they had a history of chronic instability or fracture or current tenderness of the deltoid or syndesmotic ligaments. The authors did not specify what constituted a positive anterior drawer test. They stated that the anterior drawer test of the injured ankle was compared with that of the opposite, healthy ankle. The authors reported that 30% of participants had a positive anterior drawer test at 2 weeks after injury and 11% had a positive anterior drawer test at 6 weeks after injury.24
Cetti et al25 measured anterior drawer and talar tilt in participants with an acute lateral sprain at 8 weeks and again at 24 weeks after injury. The authors did not define what constituted a positive anterior drawer or talar tilt test. Before the study began, all participants underwent stress anterior drawer and talar tilt radiographs. To participate in the study, volunteers had to have a difference in talar tilt of 6° or more and/or a difference of 3 mm or more on the anterior drawer stress radiograph compared with the opposite ankle. Participants returned for clinical re-examination at 8 and 24 weeks after injury. The authors reported that approximately 12% of participants had a positive anterior drawer at 8 weeks after injury. The number decreased to approximately 3% at 6 months after injury. Despite the small percentage of participants who had mechanical laxity as determined with manual stress tests, the authors reported that approximately 70% of participants had residual symptoms at 8 weeks after injury; 42%, at 6 months.25 Residual disability included functional instability, swelling, pain, abnormal gait, and tenderness. The authors defined functional instability as a feeling of insecurity in the ankle joint and tendency of the foot to “give way.”
Konradsen et al26 took stress radiographs of the ankle immediately after injury and at 3 months after injury. All patients were diagnosed with a grade III lateral ankle sprain. A Telos ankle stress device was used to standardize the amount of stress applied to the ankles. In 76% of the ankles, stress radiographs were preceded by injection of local anesthesia in the area of the lateral ligaments to reduce pain. For both the anterior drawer and talar tilt stress tests, the investigators applied 150 N of force to the ankle. An anterior drawer of more than 10 mm and/or a talar tilt of more than 9° was considered indicative of ligament injury. They reported that talar tilt and anterior talar translation were reduced at 3 months after injury. However, 5% of participants had pathologic stress values at 3 months. The authors did not present means or laxity values, so improvements could not be quantified.26
Munk et al27 also used stress radiographs and a manual stress examination to measure mechanical laxity after an ankle sprain. All patients in the study had a rupture of the ATFL alone or in combination with the CFL. Rupture was verified arthrographically in all participants. Of the original 149 patients enrolled in the study, 78 were evaluated at follow-up. Participants were examined with a manual anterior drawer test at neutral flexion and with a stress talar tilt test. The mean follow-up time with participants was 11 years (range, 9–13 years). They reported that 4 patients had severe mechanical laxity as assessed by a manual anterior drawer test and 37 patients had moderate mechanical laxity. The manual anterior drawer test revealed stable ankles in 37 patients. The authors did not state what constituted a positive anterior drawer test or severe or moderate mechanical laxity. Therefore, more than half of the participants had mechanical laxity at 1 year after injury.27 Stress talar tilt tests showed mechanical laxity in 12 patients when the talar tilt limit of ≥3 mm was used. Only 1 patient had mechanical laxity when the limit of ≥6° was used. The authors also reported that moderate arthrosis was present in 4 ankle joints. The exact timeline when patients were examined was not reported. The role that recurrent injury may have played in the study is also unknown.
Finally, Broström28 also objectively measured mechanical stability. He reported that all patients had a recent ankle sprain and had a ligament rupture verified by arthography. He did not specify the degree of injury or the ligaments that were ruptured. To document mechanical laxity and instability, the author took both objective and subjective measurements. Follow-up time ranged from 1 to more than 4 years. Of the 281 participants originally enrolled in the study, 242 participants were available for clinical follow-up. The manual anterior drawer test was performed to test mechanical laxity. The anterior drawer test was considered positive if a distinct depression was present between the talus and malleolus compared with the opposite ankle. To subjectively assess instability, participants were asked about residual symptoms, particularly a feeling of instability in the ankle, swelling, aching, pain on movement, and further sprains. Objectively, the investigator reported that 28% of participants in 1 treatment group and 31% of participants in another group had a positive anterior drawer more than 1 year after the initial ankle sprain.28 The difference between the 2 treatment groups was in the type of immobilization received after injury. Although most participants were symptom free at follow-up, 20% reported that their ankles felt unstable. Specifically, those participants reported that their ankles felt weaker and gave way.
Of the 7 articles reviewed, 1 set of authors only subjectively assessed ankle mechanical stability. Eiff et al29 assessed subjective feelings (ankle giving way) at 3 days, 10 days, 3 weeks, 6 weeks, 3 months, 6 months, and 12 months after the initial injury. The authors did not report the grade of ankle injury. They initially measured talar tilt on stress radiographs, but they did not perform this examination again. The authors also did not report the results of the stress radiographs. At each follow-up session, they obtained information regarding current symptoms (pain and swelling), current activity and work level, functional instability (giving way), treatment agents used, and rehabilitation performed. The ankle also was examined for swelling, ecchymosis, tenderness, range of motion, and weight-bearing ability. Twenty-two percent of participants reported giving way in the ankle at 3 weeks after injury. This number decreased to 19% at 6 weeks, 14% at 3 months, 8% at 6 months, and 3% at 1 year.29
Discussion
Despite rehabilitation and treatment, a moderate percentage (approximately 30%) of participants appeared to have objective mechanical laxity and subjective instability up to 1 year after an initial ankle sprain. These studies suggested that mechanical stability may be regained after injury. All of the studies included a period of immobilization as part of the treatment for ankle sprains, but immobilization may not allow mechanical stability to return. An exact timeline of ligament healing cannot be provided based on the articles reviewed; however, researchers reported that improvements in mechanical stability were not seen until at least 6 weeks to 3 months. Based on these findings, patients may be returning to activity before the ligaments of the ankle have healed fully.
The reliability of the methods to measure mechanical laxity have been questioned.12,30–33 In the 6 studies that objectively assessed ankle mechanical laxity, the investigators used either a manual stress test or stress radiographs. Two of the most common manual stress tests for the ankle are the anterior drawer and talar tilt tests. The anterior drawer test is performed with the application of an anterior load applied to the ankle. For the talar tilt test, an inversion-eversion torque is applied to the ankle. The anterior drawer test is used to assess stability of the ATFL, and the inversion stress of talar tilt tests the CFL. Stress radiographs of the ankle are performed with application of an inversion (for the CFL) or anterior load (for the ATFL) to the ankle during x-ray exposure. This stress can be applied manually or with a device to assist in positioning. Investigators have questioned the reliability of these tests.12,30–33
Manual examination relies on the clinician's subjectivity and experience. Fujii et al34 reported that manual stress tests are not sufficient for accurate diagnosis of specific ligament involvement because of the large amount of individual variation. Investigators in 2 of the studies that we reviewed used only manual stress tests to assess mechanical laxity.24,25 With the low sensitivity of manual tests, the reported mechanical laxity in these 2 studies (approximately 30% of participants) may be inaccurate. One concern with manual stress tests may be that examiners are unsure of how much force they are applying when performing the tests. Tohyama et al30 reported that 30 N of force should be applied during a manual anterior drawer test. The authors measured ankle displacement at different forces before and after sectioning the lateral ligaments of the ankle. At forces of more than 30 N, they found no increases in ankle displacement.30 Therefore, clinicians need to ensure that they are not applying too much force to the ankle when performing an anterior drawer or talar tilt test because increasing the force will not increase displacement.
Researchers also have questioned the reliability and usefulness of stress radiographs.31 Overall, both the anterior stress and the talar tilt tests have been reported to have low sensitivity values (50% and 36%, respectively).31 However, specificity values are quite high (100%) for both the anterior stress and talar tilt tests.31 In 4 of the reviewed articles, the investigators used stress radiographs to assess mechanical stability.23,26–28 The low sensitivity of these stress radiographs also could have led to inaccurate assessment of mechanical laxity.
The most recent of the articles that we reviewed was published in 1998.24 Since then, more objective assessments of ankle stability have been developed. One example is an instrumented ankle arthrometer. The ankle arthrometer has been reported to be a highly reliable and valid tool for assessing stability of the ankle ligaments.10,33,35 The arthrometer is a 6 degrees-of-freedom spatial kinematic linkage system. The arthrometer consists of an adjustable plate that is fixed to the foot, a load-measuring handle that is attached to the footplate through which the load is applied, and a tibial pad that is attached to the tibia. Laxity is measured from total anterior-posterior displacement (millimeters) during loading to 125 N of anterior-posterior force and from total inversion-eversion rotation (degrees of range of motion) during loading to 4000 N mm. During measurement, the force and torque loads that are produced through the arthrometer's loading handle are transferred to the skeletal and soft tissues of the ankle-subtalar joint complex. The spatial kinematic linkage of the arthrometer measures the relative motion between the arthrometer footplate and the reference pad attached onto the tibia.
Most recently, diagnostic ultrasound (DUS) has been investigated as another possible objective measure of ankle ligament stability. It quantifies ligament integrity and structure.36 Ultrasound uses dynamic imaging techniques so that the ligaments can be observed throughout the range of motion or with stress applied to the joint. Two of the advantages of DUS are that it is not painful and it is noninvasive. The reliability and validity of using DUS to assess ankle ligament stability have not been examined. Therefore, further investigation with DUS and ankle sprains is needed. Using more objective measurement may help clinicians better understand the management and treatment of ankle sprains.
Because the exact timeline of ankle ligament healing is unknown, making sound, evidence-based rehabilitation and return-to-play decisions is difficult. Investigators and clinicians know that the percentage of reinjury and chronic instability in patients after an acute ankle sprain is large, and they need to determine the reason for these large rates. Research has demonstrated increased laxity in this population.5–8 Therefore, could mechanical laxity secondary to improper ligament healing lead to this problem? At the time of this review, researchers in only 7 studies23–29 had objectively or subjectively assessed mechanical laxity after an acute ankle sprain. However, these studies were relatively short term and used methods of assessing ankle mechanical laxity that have been questioned regarding sensitivity. Objective assessment that measures mechanical laxity immediately after an ankle sprain and for at least 1 year after injury is needed. When mechanical laxity after an acute ankle sprain is understood, evidence-based rehabilitation can be developed to help stability and potentially decrease reinjury and the development of CAI. Specifically, clinicians would know the length of time necessary to protect and immobilize an ankle after a sprain to facilitate stability. Additionally, return-to-play decisions could be made based on the stability status of the ankle ligaments. By understanding the healing process, we can make better decisions to help prevent further injury.
Conclusions
In the studies examined, mechanical stability did not occur until at least 6 weeks to 3 months after injury. However, at 6 weeks up to 1 year after injury, a moderate percentage of participants still had objective mechanical laxity and subjective ankle instability. The reliability of the methods used to assess mechanical laxity has been questioned in the recent literature. Based on the available evidence and the knowledge of the large rate of ankle reinjury and development of CAI, we believe that more research is needed. This research should focus on more reliable methods of measuring ankle laxity and on measuring laxity for at least 1 year after injury. By measuring mechanical laxity indirectly, we can infer how long ligament healing may take after injury. Knowledge of optimal healing time will help clinicians make better decisions during rehabilitation and for return to play. Even more important, this knowledge could prevent further injury and damage to the ankle.
Footnotes
Tricia J. Hubbard, PhD, ATC, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. Charlie A. Hicks-Little, MS, ATC, contributed to analysis and interpretation of the data and drafting, critical revision, and final approval of the article.
References
- 1.Kannus P, Renström P. Treatment for acute tears of the lateral ligaments of the ankle: operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991;73(2):305–312. [PubMed] [Google Scholar]
- 2.McKay G.D, Goldie P.A, Payne W.R, Oakes B.W. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35(2):103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 4.Harrington K.D. Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am. 1979;61(3):354–361. [PubMed] [Google Scholar]
- 5.Hubbard T.J, Kramer L.C, Denegar C.R, Hertel J. Contributing factors to chronic ankle instability. Foot Ankle Int. 2007;28(3):343–354. doi: 10.3113/FAI.2007.0343. [DOI] [PubMed] [Google Scholar]
- 6.Hertel J, Denegar C.R, Monroe M.M, Stokes W.L. Talocrural and subtalar joint instability after lateral ankle sprain. Med Sci Sports Exerc. 1999;31(11):1501–1508. doi: 10.1097/00005768-199911000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Bass B, Lentell G.B, Lopez D, McGuire L, Sarrels M, Synder P. The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Sports Phys Ther. 1995;21(4):206–215. doi: 10.2519/jospt.1995.21.4.206. [DOI] [PubMed] [Google Scholar]
- 8.Louwerens J.W, Ginai A.Z, van Linge B, Snijders C.J. Stress radiography of the talocrural and subtalar joints. Foot Ankle Int. 1995;16(3):148–155. doi: 10.1177/107110079501600308. [DOI] [PubMed] [Google Scholar]
- 9.Broström L. Sprained ankles, I: anatomic lesions in recent sprains. Acta Chir Scand. 1964;128:483–495. [PubMed] [Google Scholar]
- 10.Kovaleski J.E, Hollis J.M, Heitman R.J, Gurchiek L.R, Pearsall AW I.V. Assessment of ankle-subtalar-joint-complex laxity using an instrumented ankle arthrometer: an experimental cadaveric investigation. J Athl Train. 2002;37(4):467–474. [PMC free article] [PubMed] [Google Scholar]
- 11.Bahr R, Pena F, Shine J, et al. Mechanics of the anterior drawer and talar tilt tests: a cadaveric study of lateral ligament injuries of the ankle. Acta Orthop Scand. 1997;68(5):435–441. doi: 10.3109/17453679708996258. [DOI] [PubMed] [Google Scholar]
- 12.Tohyama H, Beynnon B.D, Renström P.A, Theis M.J, Fleming B.C, Pope M.H. Biomechanical analysis of the ankle anterior drawer test for anterior talofibular ligament injuries. J Orthop Res. 1995;13(4):609–614. doi: 10.1002/jor.1100130417. [DOI] [PubMed] [Google Scholar]
- 13.Hollis J.M, Blasier R.D, Flahiff C.M. Simulated lateral ankle ligamentous injury: changes in ankle stability. Am J Sports Med. 1995;23(6):672–677. doi: 10.1177/036354659502300606. [DOI] [PubMed] [Google Scholar]
- 14.Hollis J.M, Blasier R.D, Flahiff C.M, Hofmann O.E. Biomechanical comparison of reconstruction techniques in simulated lateral ankle ligament injury. Am J Sports Med. 1995;23(6):678–682. doi: 10.1177/036354659502300607. [DOI] [PubMed] [Google Scholar]
- 15.Mattacola C.G, Dwyer M.K. Rehabilitation of the ankle after acute sprain or chronic instability. J Athl Train. 2002;37(4):413–429. [PMC free article] [PubMed] [Google Scholar]
- 16.Martin R.B, Burr D.B, Sharkey N.A. Skeletal Tissue Mechanics. New York, NY: Springer-Verlag; p. 1998. [Google Scholar]
- 17.Denegar C.R, Miller SJ I.I.I. Can chronic ankle instability be prevented? Rethinking management of lateral ankle sprains. J Athl Train. 2002;37(4):430–435. [PMC free article] [PubMed] [Google Scholar]
- 18.Bernier J.N, Perrin D.H. Effect of coordination training on proprioception of the functionally unstable ankle. J Orthop Sports Phys Ther. 1998;27(4):264–275. doi: 10.2519/jospt.1998.27.4.264. [DOI] [PubMed] [Google Scholar]
- 19.Mattacola C.G, Lloyd J.W. Effects of a 6-week strength and proprioception training program on measures of dynamic balance: a single-case design. J Athl Train. 1997;32(2):127–135. [PMC free article] [PubMed] [Google Scholar]
- 20.Wester J.U, Jespersen S.M, Nielsen K.D, Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: a prospective randomized study. J Orthop Sports Phys Ther. 1996;23(3):332–336. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- 21.PEDro Scale. http://www.pedro.fhs.usyd.edu.au/scale_item.html. Accessed March 2007.
- 22.Hubbard T.J, Aronson S.L, Denegar C.R. Does cryotherapy hasten return to participation? A systematic review. J Athl Train. 2004;39(1):88–94. [PMC free article] [PubMed] [Google Scholar]
- 23.Freeman M.A.R. Treatment of ruptures of the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47(4):661–668. [PubMed] [Google Scholar]
- 24.Avci S, Sayli U. Comparison of the results of short-term rigid and semi-rigid cast immobilization for the treatment of grade 3 inversion injuries of the ankle. Injury. 1998;29(4):581–584. doi: 10.1016/s0020-1383(98)00129-6. [DOI] [PubMed] [Google Scholar]
- 25.Cetti R, Christensen S.E, Corfitzen M.T. Ruptured fibular ankle ligament: plaster or Pliton brace. Br J Sports Med. 1984;18(2):104–109. doi: 10.1136/bjsm.18.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Konradsen L, Hølmer P, Søndergaard L. Early mobilizing treatment for grade III ankle ligament injuries. Foot Ankle. 1991;12(2):69–73. doi: 10.1177/107110079101200202. [DOI] [PubMed] [Google Scholar]
- 27.Munk B, Holm-Christensen K, Lind T. Long-term outcome after ruptured lateral ankle ligaments: a prospective study of three different treatments in 79 patients with 11-year follow-up. Acta Orthop Scand. 1995;66(5):452–454. doi: 10.3109/17453679508995586. [DOI] [PubMed] [Google Scholar]
- 28.Broström L. Sprained ankles, V: treatment and prognosis in recent ligament ruptures. Acta Chir Scand. 1966;132(5):537–550. [PubMed] [Google Scholar]
- 29.Eiff M.P, Smith A.T, Smith G.E. Early mobilization versus immobilization in the treatment of lateral ankle sprains. Am J Sports Med. 1994;22(1):83–88. doi: 10.1177/036354659402200115. [DOI] [PubMed] [Google Scholar]
- 30.Tohyama H, Yasuda K, Ohkoshi Y, Beynnon B.D, Renstrom P.A. Anterior drawer test for acute anterior talofibular ligament injuries of the ankle: how much load should be applied during the test. Am J Sports Med. 2003;31(2):226–232. doi: 10.1177/03635465030310021201. [DOI] [PubMed] [Google Scholar]
- 31.Harper M.C. Stress radiographs in the diagnosis of lateral instability of the ankle and hindfoot. Foot Ankle. 1992;13(8):435–438. doi: 10.1177/107110079201300801. [DOI] [PubMed] [Google Scholar]
- 32.Frost S.C.L, Amendola A. Is stress radiography necessary in the diagnosis of acute or chronic ankle instability. Clin J Sport Med. 1999;9(1):40–45. doi: 10.1097/00042752-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Kovaleski J.E, Gurchiek L.R, Heitman R.J, Hollis J.M, Pearsall AW I.V. Instrumented measurement of anteroposterior and inversion-eversion laxity of the normal ankle joint complex. Foot Ankle Int. 1999;20(12):808–814. doi: 10.1177/107110079902001210. [DOI] [PubMed] [Google Scholar]
- 34.Fujii T, Luo Z.P, Kitaoka H.B, An K.N. The manual stress test may not be sufficient to differentiate ankle ligament injuries. Clin Biomech (Bristol, Avon) 2000;15(8):619–623. doi: 10.1016/s0268-0033(00)00020-6. [DOI] [PubMed] [Google Scholar]
- 35.Hubbard T.J, Kovaleski J.E, Kaminski T.W. Reliability of intratester and intertester measurements derived from an instrumented ankle arthrometer. J Sport Rehabil. 2003;12(3):208–220. [Google Scholar]
- 36.Moosmayer S, Smith H.J. Diagnostic ultrasound of the shoulder: a method for experts only? Results from an orthopedic surgeon with relative inexpensive compared to operative findings. Acta Orthop. 2005;76(4):503–508. doi: 10.1080/17453670510041484. [DOI] [PubMed] [Google Scholar]