Abstract
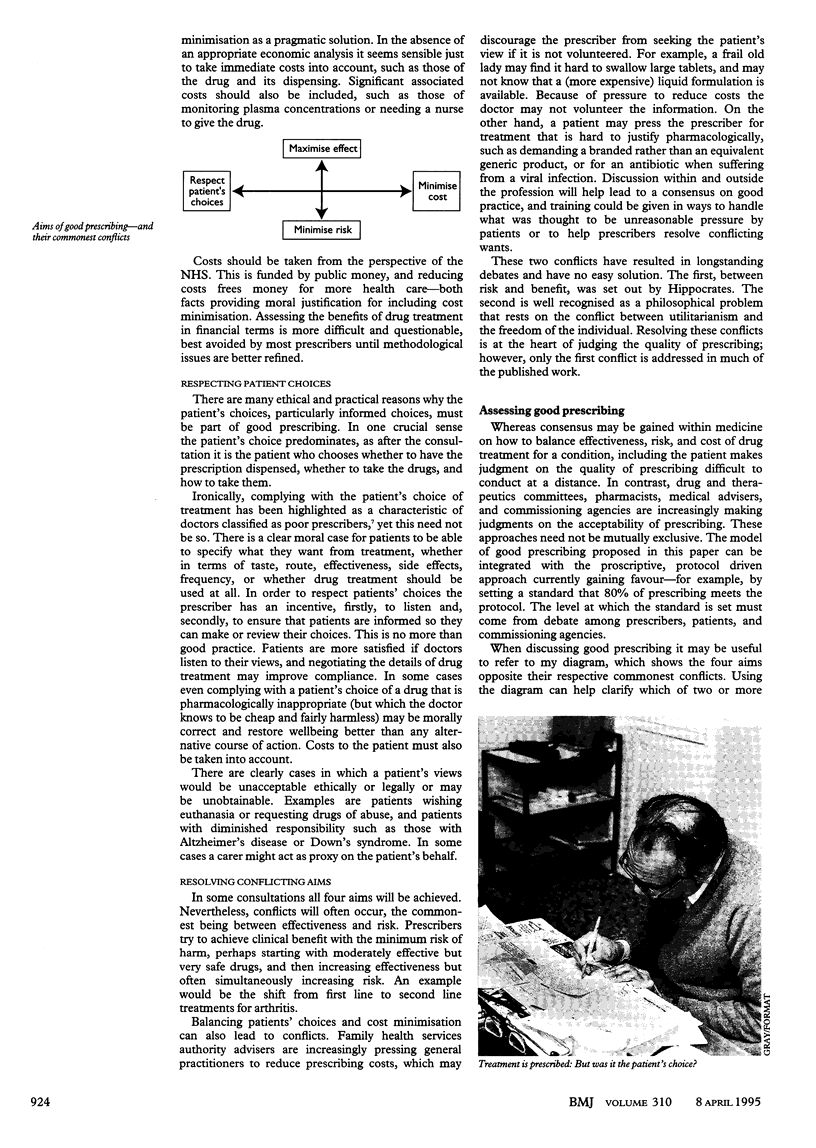
Drugs are the mainstay of medical treatment, yet there are few reports on what constitutes "good prescribing." What is more the existing guidance tends to imply that right answers exist, rather than recognising the complex trade offs that have to be made between conflicting aims. This paper proposes four aims that a prescriber should try to achieve, both on first prescribing a drug and on subsequently monitoring it. They are: to maximise effectiveness, minimise risks, minimise costs, and respect the patient's choices. This model of good prescribing brings together the traditional balancing of risks and benefits with the need to reduce costs and the right of the patient to make choices in treatment. The four aims are shown as a diagram plotting their commonest conflicts, which may be used as an aid to discussion and decision making.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bradley C. P. Decision making and prescribing patterns--a literature review. Fam Pract. 1991 Sep;8(3):276–287. doi: 10.1093/fampra/8.3.276. [DOI] [PubMed] [Google Scholar]
- FINNEY D. J. THE DESIGN AND LOGIC OF A MONITOR OF DRUG USE. J Chronic Dis. 1965 Jan;18:77–98. doi: 10.1016/0021-9681(65)90054-8. [DOI] [PubMed] [Google Scholar]
- Karch F. E., Lasagna L. Adverse drug reactions. A critical review. JAMA. 1975 Dec 22;234(12):1236–1241. [PubMed] [Google Scholar]
- Schwartz R. K., Soumerai S. B., Avorn J. Physician motivations for nonscientific drug prescribing. Soc Sci Med. 1989;28(6):577–582. doi: 10.1016/0277-9536(89)90252-9. [DOI] [PubMed] [Google Scholar]