Abstract
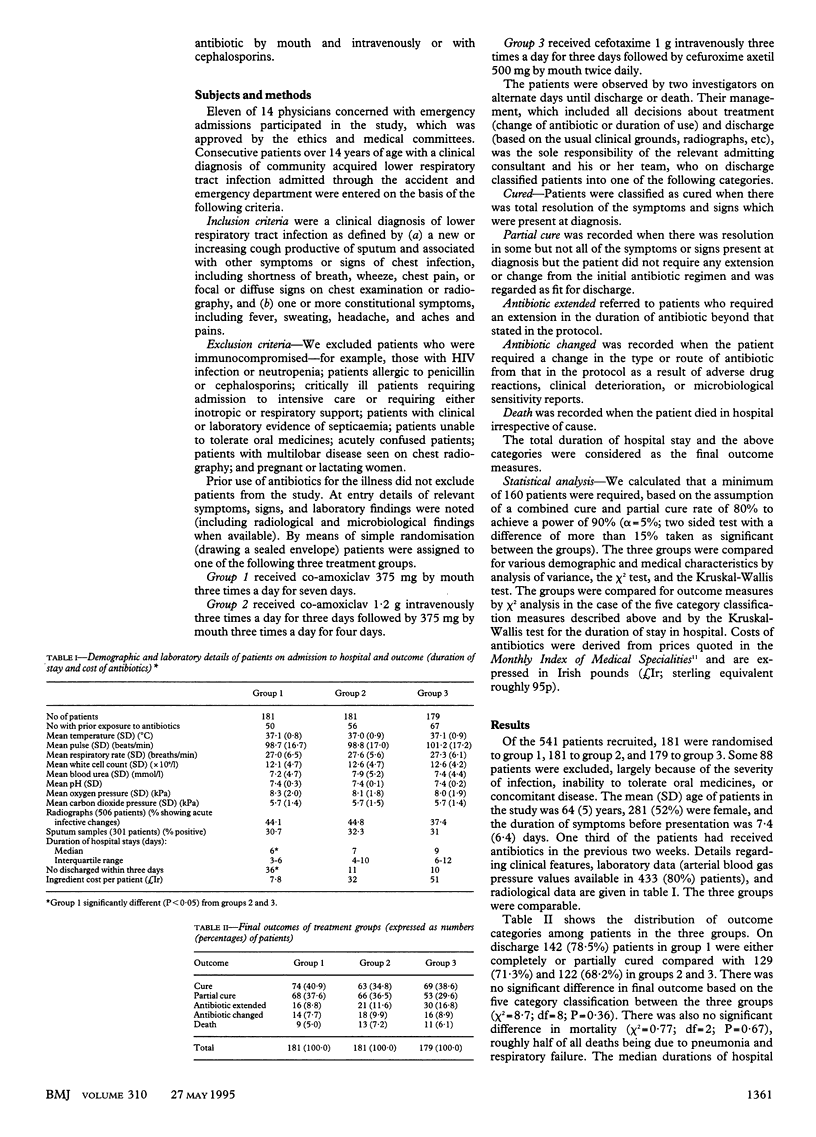
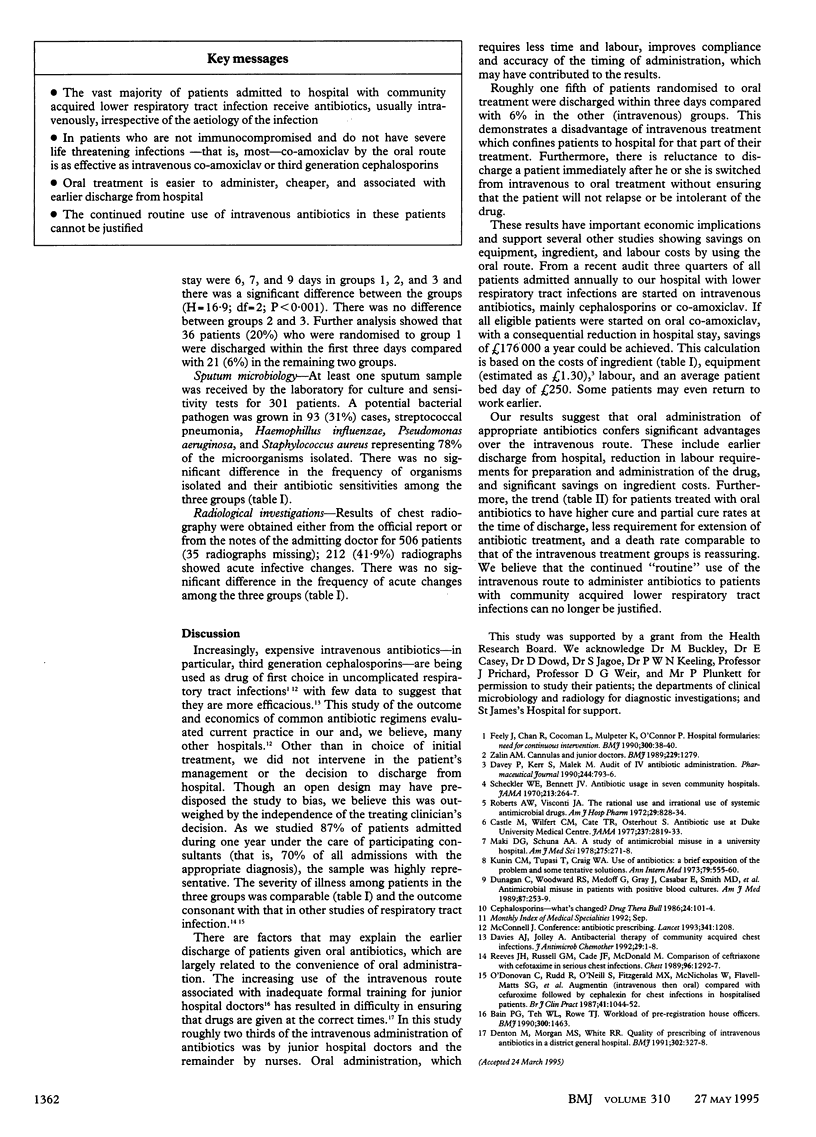
OBJECTIVE--To see whether there is a difference in outcome between patients treated with oral and intravenous antibiotics for lower respiratory tract infection. DESIGN--Open controlled trial in patients admitted consecutively and randomised to treatment with either oral co-amoxiclav, intravenous followed by oral co-amoxiclav, or intravenous followed by oral cephalosporins. SETTING--Large general hospital in Dublin. PATIENTS--541 patients admitted for lower respiratory tract infection during one year. Patients represented 87% of admissions with the diagnosis and excluded those who were immunocompromised and patients with severe life threatening infection. MAIN OUTCOME MEASURES--Cure, partial cure, extended antibiotic treatment, change of antibiotic, death, and cost and duration of hospital stay. RESULTS--There were no significant differences between the groups in clinical outcome or mortality (6%). However, patients randomised to oral co-amoxiclav had a significantly shorter hospital stay than the two groups given intravenous antibiotic (median 6 v 7 and 9 days respectively). In addition, oral antibiotics were cheaper, easier to administer, and if used routinely in the 800 or so patients admitted annually would lead to savings of around 176,000 pounds a year. CONCLUSIONS--Oral antibiotics in community acquired lower respiratory tract infection are at least as efficacious as intraveous therapy. Their use reduces labour and equipment costs and may lead to earlier discharge from hospital.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Castle M., Wilfert C. M., Cate T. R., Osterhout S. Antibiotic use at Duke University Medical Center. JAMA. 1977 Jun 27;237(26):2819–2822. [PubMed] [Google Scholar]
- Davies A. J., Jolley A. Antibacterial therapy of community-acquired chest infections. J Antimicrob Chemother. 1992 Jan;29(1):1–4. doi: 10.1093/jac/29.1.1. [DOI] [PubMed] [Google Scholar]
- Denton M., Morgan M. S., White R. R. Quality of prescribing of intravenous antibiotics in a district general hospital. BMJ. 1991 Feb 9;302(6772):327–328. doi: 10.1136/bmj.302.6772.327-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunagan W. C., Woodward R. S., Medoff G., Gray J. L., 3rd, Casabar E., Smith M. D., Lawrenz C. A., Spitznagel E. Antimicrobial misuse in patients with positive blood cultures. Am J Med. 1989 Sep;87(3):253–259. doi: 10.1016/s0002-9343(89)80146-9. [DOI] [PubMed] [Google Scholar]
- Guidelines for writing papers. BMJ. 1990 Jan 6;300(6716):38–40. [PMC free article] [PubMed] [Google Scholar]
- Kunin C. M., Tupasi T., Craig W. A. Use of antibiotics. A brief exposition of the problem and some tentative solutions. Ann Intern Med. 1973 Oct;79(4):555–560. doi: 10.7326/0003-4819-79-4-555. [DOI] [PubMed] [Google Scholar]
- Maki D. G., Schuna A. A. A study of antimicrobial misuse in a university hospital. Am J Med Sci. 1978 May-Jun;275(3):271–282. doi: 10.1097/00000441-197805000-00005. [DOI] [PubMed] [Google Scholar]
- McConnell J. Antibiotic prescribing. Lancet. 1993 May 8;341(8854):1208–1208. doi: 10.1016/0140-6736(93)91025-h. [DOI] [PubMed] [Google Scholar]
- O'Donovan C., Rudd R., O'Neill S., Fitzgerald M. X., McNicholas W., Flavell-Matts S. G., Howell F., McKenzie A., Whittaker J. Augmentin (intravenous then oral) compared with cefuroxime followed by cephalexin for chest infections in hospitalised patients. Br J Clin Pract. 1987 Dec;41(12):1044–1052. [PubMed] [Google Scholar]
- Reeves J. H., Russell G. M., Cade J. F., McDonald M. Comparison of ceftriaxone with cefotaxime in serious chest infections. Chest. 1989 Dec;96(6):1292–1297. doi: 10.1378/chest.96.6.1292. [DOI] [PubMed] [Google Scholar]
- Roberts A. W., Visconti J. A. The rational and irrational use of systemic antimicrobial drugs. Am J Hosp Pharm. 1972 Oct;29(10):828–834. [PubMed] [Google Scholar]
- Scheckler W. E., Bennett J. V. Antibiotic usage in seven community hospitals. JAMA. 1970 Jul 13;213(2):264–267. [PubMed] [Google Scholar]
- Zalin A. M. Cannulas and junior doctors. BMJ. 1989 Nov 18;299(6710):1279–1279. doi: 10.1136/bmj.299.6710.1279. [DOI] [PMC free article] [PubMed] [Google Scholar]


