Abstract
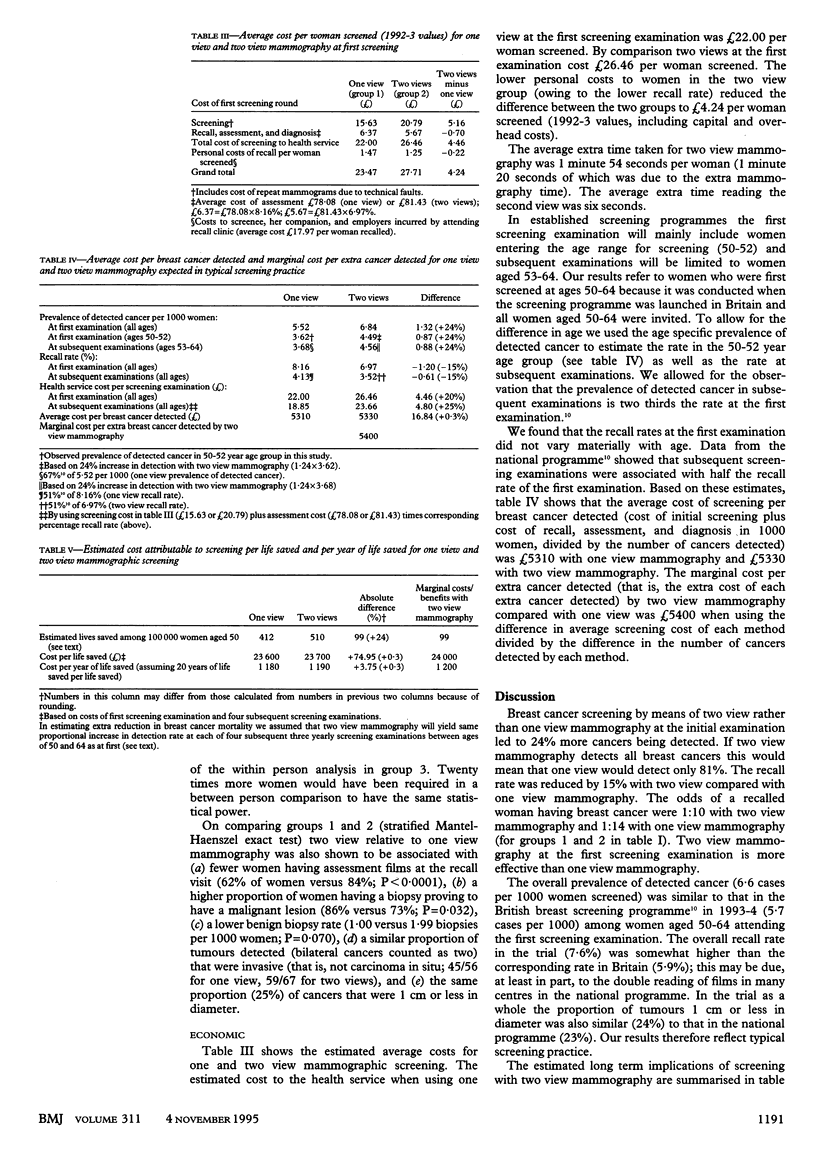
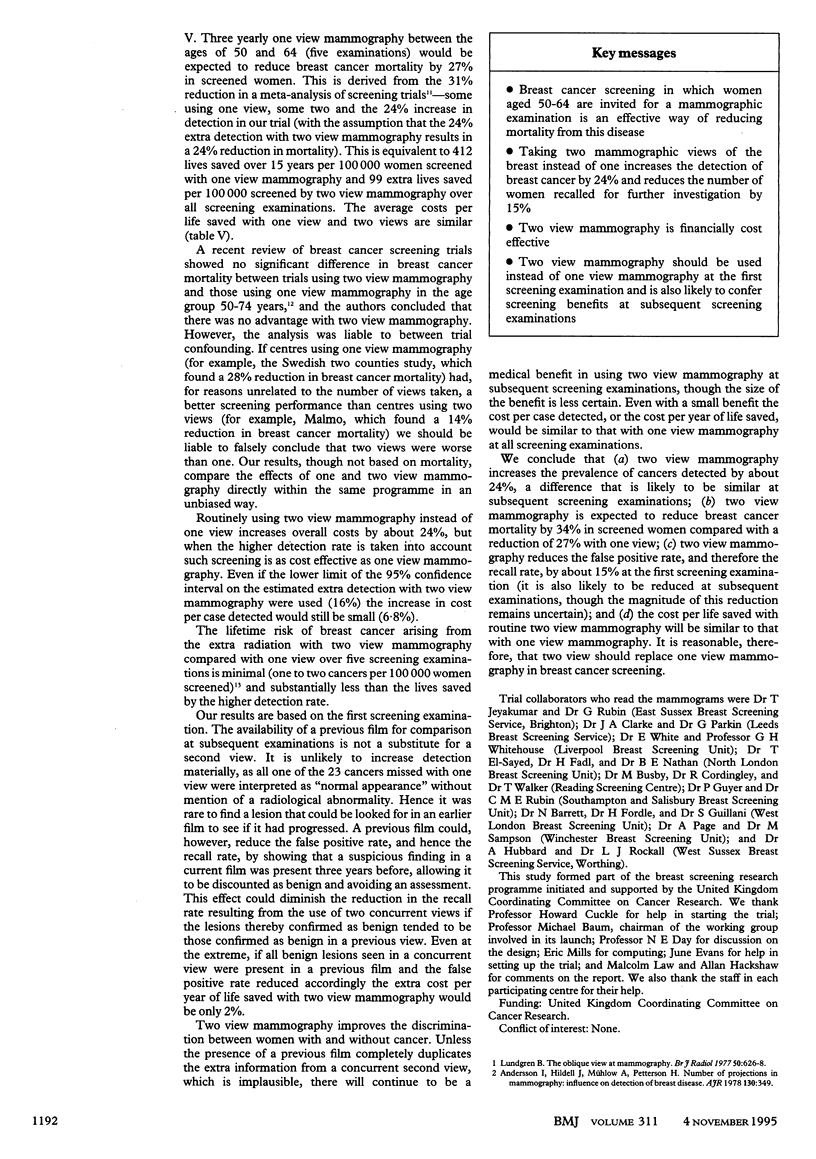
OBJECTIVE--To compare one view (oblique) and two view (oblique and craniocaudal) mammography in breast cancer screening. DESIGN--Randomised controlled trial. SETTING--Nine breast screening centres in England. SUBJECTS--40,163 women aged 50-64 attending their first breast screening examination. INTERVENTIONS--Women were randomised to have one view mammography, two view mammography, or two view mammography in which one view was read by one reader and both views were read by another. MAIN OUTCOME MEASURES--Prevalence of cancer detected, recall rates, cost per cancer detected, and marginal cost per extra cancer detected. RESULTS--Two view mammography detected 24% more women with breast cancer (95% confidence interval 16% to 31%) than one view mammography. Prevalence of detected cancer was 6.84 with two view mammography and 5.52 per 1000 women with one view. The proportion of women recalled for assessment was 15% lower (95% confidence interval 6% to 23%) with two view (6.97%) than with one view (8.16%) mammography. The cost of two view screening was higher (26.46 pounds compared with 22.00 pounds per examination) but the average cost per cancer detected was similar (5330 pounds compared with 5310 pounds) and the marginal cost per extra cancer detected with two views was similar to the average cost (5400 pounds). CONCLUSION--Two view mammography is medically more effective than one view; it detects more cancers and reduces recall rates; it is also similarly cost effective financially.
Full text
PDF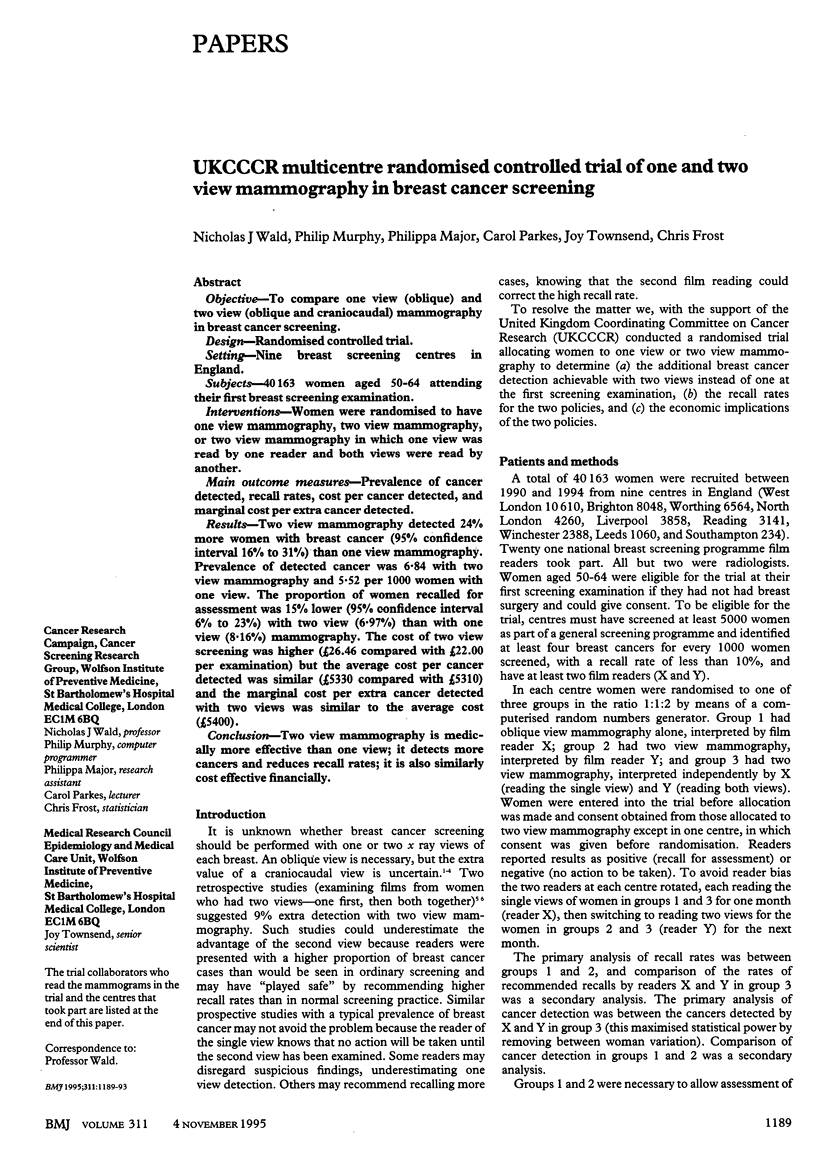


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andersson I., Hildell J., Mühlow A., Pettersson H. Number of projections in mammography: influence on detection of breast disease. AJR Am J Roentgenol. 1978 Feb;130(2):349–351. doi: 10.2214/ajr.130.2.349. [DOI] [PubMed] [Google Scholar]
- Andersson I. Radiographic screening for breast carcinoma. III. Appearance of carcinoma and number of projections to be used at screening. Acta Radiol Diagn (Stockh) 1981;22(4):407–420. doi: 10.1177/028418518102200404. [DOI] [PubMed] [Google Scholar]
- DerSimonian R., Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986 Sep;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Feig S. A. Radiation risk from mammography: is it clinically significant? AJR Am J Roentgenol. 1984 Sep;143(3):469–475. doi: 10.2214/ajr.143.3.469. [DOI] [PubMed] [Google Scholar]
- Kerlikowske K., Grady D., Rubin S. M., Sandrock C., Ernster V. L. Efficacy of screening mammography. A meta-analysis. JAMA. 1995 Jan 11;273(2):149–154. [PubMed] [Google Scholar]
- Lundgren B. The oblique view of mammography. Br J Radiol. 1977 Sep;50(597):626–628. doi: 10.1259/0007-1285-50-597-626. [DOI] [PubMed] [Google Scholar]
- Sickles E. A., Weber W. N., Galvin H. B., Ominsky S. H., Sollitto R. A. Baseline screening mammography: one vs two views per breast. AJR Am J Roentgenol. 1986 Dec;147(6):1149–1153. doi: 10.2214/ajr.147.6.1149. [DOI] [PubMed] [Google Scholar]
- Tabár L., Faberberg G., Day N. E., Holmberg L. What is the optimum interval between mammographic screening examinations? An analysis based on the latest results of the Swedish two-county breast cancer screening trial. Br J Cancer. 1987 May;55(5):547–551. doi: 10.1038/bjc.1987.112. [DOI] [PMC free article] [PubMed] [Google Scholar]


