Abstract
OBJECTIVE—We assessed the effects of a 2-day in-hospital diabetes educational program in preventing or delaying progression of impaired glucose tolerance (IGT) to type 2 diabetes, including analysis of changes in serum lipids, body weight, and blood pressure after the program.
RESEARCH DESIGN AND METHODS—A total of 426 subjects (51 ± 9 years, BMI 24.6 ± 3.9 kg/m2) with newly diagnosed IGT were randomly assigned to three groups, 143 as the short-term hospitalization with diabetes education and support (STH) group, 141 as the nonhospitalization but diabetes education and support (DES) group, and 142 as the neither hospitalization nor education (control) group.
RESULTS—The average follow-up was 3.1 years. The incidence of diabetes was 8.0, 10.7, and 13.2 cases per 100 person-years for STH, DES, and control groups, respectively. The incidence of diabetes was 42% lower (95% CI 33–51%) in the STH group and 27% lower (15–37%) in the DES group than in the control group. The incidence of diabetes was 21% lower (10–31%) in the STH group than in the DES group.
CONCLUSIONS—The 2-day in-hospital program with diabetes education and support every 3 months was more effective in preventing or delaying the progression from IGT to diabetes than only diabetes education and support every 3 months.
In recent years, the number of new patients with type 2 diabetes and impaired glucose tolerance (IGT) has increased steadily around the world, and it is estimated that >300 million people worldwide will have type 2 diabetes by the year 2025 (1). Based on many large-scale clinical studies, it is clear that IGT is a major risk factor for cardiovascular disease (2–4). It is also clear that the prevention of diabetes before its onset and treatment of this disease in its early stages are important from the perspective of public health, medical treatment, and economic management (5). Thus, there have been several intervention studies with lifestyle modification that have demonstrated positive effects (5–8). However, in these studies, intensive monitoring was required, and there are many difficulties in carrying out similar interventions in general clinics. For example, in the Diabetes Prevention Program (DPP), only 38% of the participants in the intensive lifestyle intervention group had achieved the goal weight loss of ≥7% after 3 years. Furthermore, the program required the cooperation of many staff and substantial costs (6,7). Based on this background, we designed a 2-day in-hospital, simple and easy-to-apply educational program. The aim of this study was to assess the efficacy of such a program with diabetes education and support every 3 months in preventing or delaying progression to type 2 diabetes in patients with IGT.
RESEARCH DESIGN AND METHODS
We recruited the participants from 11 outpatient practices and a health evaluation and promotion center in the Joetsu area. The study was a community-based clinical trial. All participants were followed up at Niigata-Rousai Hospital using the prospective randomized open blinded end point (PROBE) design, which aims to create conditions similar to routine clinical practice (9). We screened for patients aged 20–70 years, with BMI 20–34 kg/m2, fasting plasma glucose concentration ≥100 mg/dl, or A1C level between 5.2 and 6.4%. The patients were eligible for our study if they had IGT, defined as a plasma glucose concentration ≤125 mg/dl in the fasting state and 140–199 mg/dl 2 h after a 75-g oral glucose load, according to the 2003 American Diabetes Association criteria (8). In addition, all participants were confirmed to have systolic blood pressure <150 mmHg, diastolic blood pressure <100 mmHg, total cholesterol <300 mg/dl, triglycerides <220 mg/dl, and LDL cholesterol <180 mg/dl and were not taking any medication that might affect glycemic control. All end points were assessed by an independent end point committee, whose members were unaware of the treatment status of the participants.
Written informed consent was obtained from all participants. The medical ethical committees of our hospital approved the trial protocol.
Interventions
Eligible participants were randomly assigned to one of three groups: the short-term hospitalization with diabetes support and education (STH) group, nonhospitalization but diabetes education and support (DES) group, or neither hospitalization nor education (control) group. Randomization was done centrally with a block design procedure and stratified according to age (three groups: 20–44, 45–59, and 60–70 years) and sex (two groups: male and female). The participant randomization list was kept in a secure location at a central coordination center and was not available to any individual.
In the control group, participants were given general information about diabetes and IGT. Their physicians also provided diabetes information brochures with general instructions for diet and improvement of lifestyle; however, no individual instruction or formal group counseling sessions were conducted.
In the STH group, participants received a nine-lesson curriculum, designed as a clinical course, covering special diet, exercise, and behavior modification to help them change their behavior (supplemental Fig. 2 available in an online appendix at http://dx.doi.org/10.2337/dc07-2272). In a preliminary trial (T.K., K.T., T.A., T.T., Y.O., E.M., Y.T., unpublished observations), we found that a 2-day hospital stay and nine lessons had a maximal effect in maintaining motivation and in understanding diabetes and IGT. This was less costly than a 3-day or longer hospital stay and was also more effective than a 1-day hospital stay; therefore, we selected these parameters. Lessons were taught by nutritionists, pharmacists, physical therapists, nurses, medical technologists, and physicians on a one-to-one or group basis, and each lesson, which lasted 20–40 min, was flexible, culturally sensitive, and individualized. We set the diet at 25–30 kcal/kg of ideal body weight for each participant, and the goal of dietary intervention was a total daily intake of fat that was <20–25% of daily energy intake. In addition, participants received exercise therapy in the form of participation in a traditional Japanese physical exercise radio program. We instructed the participants to continue walking or doing the radio exercise routine for at least 30 min/day, a minimum of 5 times a week after discharge from hospital. Subsequent individual sessions every 3 months with nurses or nutritionists, designed to reinforce the behavioral changes, were similar to the program received by participants in the DES group.
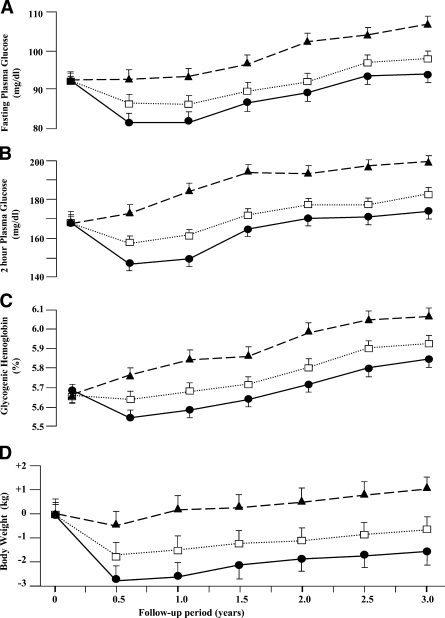
Figure 2.
Change in fasting plasma glucose (A), 2-h OGTT plasma glucose (B), A1C (C), and body weight (D) according to study group. Each data point represents the mean ± SE of the participants of the specific groups examined at the indicated time. •, STH group; □, DES group; ▴, control group.
In the DES group, participants were provided with written information and periodic 20- to 30-min individual sessions that emphasized the importance of a healthy lifestyle. Participants were encouraged to follow the diabetes guidebook (10) issued by the Japan Diabetes Society. They were also instructed to follow the equivalent of the food guidebook (11) to reduce their weight and to increase their physical activity.
Our study steering committee provided the guidelines, in which information about various teaching methods was described, to all staff involved in the study. All of the staff attended a 2-day training session each year in which they received standardized instructions on the diet and exercise interventions.
Follow-up procedures
All participants were given a reminder in which outpatient guidance was noted every 3 months. They were also seen at 3-month intervals by their physicians. Body weight, waist circumference, and blood pressure were measured, and blood and urine samples were taken for examination. The general health of each participant was assessed, and the results of blood and urine examinations were explained by the physician. Physicians gave advice about diabetes or IGT for 5–10 min in every interview. Thereafter, participants in the STH and DES groups received 20- to 30-min individual sessions as described above. All participants were surveyed at baseline and every 6 months about their adherence to recommendations. Self-assessment reports that referred to the DPS method were used for the survey (12).
The primary end point was the development of diabetes, diagnosed on the basis of an annual 75-g oral glucose tolerance test (OGTT) or a fasting plasma glucose check at every 3-month visit, according to the 2003 criteria of the American Diabetes Association (8): a plasma glucose value of ≥126 mg/dl in the fasting state or ≥200 mg/dl 2 h after taking a 75-g oral glucose load (Trelan-G75). All participants underwent the OGTT annually, but if the fasting plasma glucose concentration was ≥126 mg/dl at any 3-month visit, the participant was automatically scheduled to undergo an OGTT within 4 weeks. Participants who reached the primary end point discontinued this study. In addition, if total cholesterol increased to ≥300 mg/dl or triglycerides increased to ≥220 mg/dl or LDL cholesterol increased to ≥180 mg/dl, the participants discontinued this study and treatment with hypolipidemic agents was initiated by their physicians.
Laboratory investigations
All blood samples were transferred to the central laboratory at Niigata-Rousai Hospital, and aliquots were stored at −70°C until use. Plasma glucose levels were determined by the glucose oxidation method (chemical reagent and Glucose AUTO and STAT GA-1160 analyzer; ARKRAY). A1C (normal value 4.0–5.8%) was measured by high-performance liquid chromatography (ADAMS A1c HA-8160; ARKRAY). Total cholesterol and triglycerides were measured by cholesterol oxidation enzyme and enzymatic colorimetry methods (Daiichi-kayaku, H-7700; Hitachi). LDL cholesterol was measured by the direct method without deposition (Daiichi-kayaku H-7700).
Costs estimate
In our analyses, we followed the recommendations of the Panel on Cost-Effectiveness in Health and Medicine (13) and the method of estimating the costs in the Diabetes Prevention Program (14). In all analyses from a health system perspective, we included only direct medical costs. In analyses from a societal perspective, we included direct medical costs, direct nonmedical costs, and indirect costs to estimate the cost per case of diabetes prevented during the trial. We used the exchange rates in 2000 (1 U.S. dollar equal to 120 Japanese yen).
Statistical analysis
On the assumption of a conversion rate of 13% per year and a 40% risk reduction, we estimated that 138 patients were required in each of the three groups to achieve 80% power to detect a significant difference with a two-sided α error of 0.05. An intention-to-treat analysis that included all patients in their assigned trial groups, regardless of whether they actually underwent intervention, was performed. Cox proportional hazards models were used to estimate hazard ratios and 95% CI for the primary end point and to perform an analysis of the primary end point adjusted for age and sex. We used non–repeated-measures ANOVA and the χ2 test to compare the baseline variables between the three groups. We used person-years: total number of the participants who developed diabetes/summation of follow-up years of each participant, to show the incidence rate. We assessed changes in variables from baseline to the end point with repeated-measures ANOVA and the Bonferroni correction. All tests were two-tailed, and P values <0.05 were considered to indicate statistical significance. Statistical analysis was performed using Sigma Stat software (SPSS, Chicago, IL). All data are represented as means ± SD.
RESULTS
From June 2003 to July 2007, we randomly assigned 426 participants to one of the three groups (143 to STH, 141 to DES, and 142 to control) (supplemental Fig. 1). No significant differences were found in the baseline characteristics, including all measured risk factors for diabetes, among the three study groups (Table 1). The participants were followed for a mean period of 3.1 years (range 1.8–4.2).
Table 1.
Baseline characteristics of participants in the STH, DES, and control groups
| All subjects | STH | DES | Control | |
|---|---|---|---|---|
| n | 426 | 143 | 141 | 142 |
| Age (years) | 51.4 ± 9.1 | 52.6 ± 8.9 | 51.1 ± 9.3 | 51.8 ± 9.2 |
| Sex (male/female) | 199/227 | 67/78 | 65/76 | 67/73 |
| Family history of diabetes (%) | 64 | 65 | 62 | 64 |
| Graduated high school (%) | 78 | 78 | 77 | 79 |
| Body weight (kg) | 65.4 ± 10.4 | 65.7 ± 11.2 | 64.9 ± 10.3 | 65.5 ± 9.8 |
| BMI (kg/m2) | 24.6 ± 3.9 | 24.7 ± 4.2 | 24.4 ± 3.8 | 24.7 ± 3.6 |
| Waist circumference (cm) | 87.5 ± 13.2 | 88.2 ± 13.6 | 86.7 ± 12.9 | 87.4 ± 13.1 |
| Systolic blood pressure (mmHg) | 131.5 ± 12.3 | 131.9 ± 11.6 | 132.0 ± 12.3 | 130.7 ± 12.3 |
| Diastolic blood pressure (mmHg) | 72.4 ± 6.1 | 72.3 ± 5.8 | 73.3 ± 6.2 | 71.5 ± 6.1 |
| Fasting plasma glucose (mg/dl) | 92.5 ± 12.8 | 93.0 ± 11.5 | 91.7 ± 12.9 | 92.2 ± 12.4 |
| Plasma glucose at 2 h after oral glucose load (mg/dl) | 168.7 ± 23.2 | 169.2 ± 22.8 | 169.3 ± 21.6 | 168.5 ± 22.4 |
| A1C (%) | 5.6 ± 0.3 | 5.7 ± 0.28 | 5.6 ± 0.23 | 5.6 ± 0.27 |
| Serum total cholesterol (mg/dl) | 188.7 ± 26.5 | 189.3 ± 27.1 | 187.2 ± 25.8 | 188.6 ± 26.2 |
| Serum LDL cholesterol (mg/dl) | 127.7 ± 18.2 | 128.3 ± 18.7 | 127.1 ± 17.3 | 127.3 ± 17.6 |
| Serum triglycerides (mg/dl) | 123.6 ± 20.1 | 124.2 ± 20.3 | 123.5 ± 21.2 | 123.4 ± 19.7 |
Data are means ± SD or n (%). There were no significant differences in all variables among the groups.
Attendance at follow-up visits was almost the same in each group (STH 97%, DES 96%, and control 94%). There were no significant differences in the adherence to recommendations (measure of physical activity and diet composition) among the three groups (data not shown).
Incidence of diabetes and change in glucose parameters
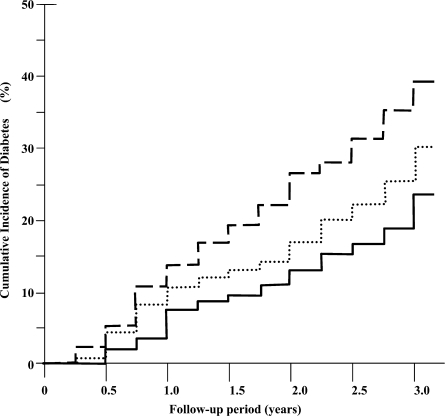
The incidence of diabetes was 8.0, 10.7, and 13.2 cases per 100 person-years in the STH, DES, and control groups, respectively (Fig. 1). The incidence of diabetes was 42% lower (95% CI 33–51%) in the STH group and 27% lower (95% CI 15–37%) in the DES group than in the control group. The incidence of diabetes was 21% lower (95% CI 10–31%) in the STH group than in the DES group. The results of all three pairwise group comparisons were statistically significant (P < 0.01). The estimated cumulative incidence of diabetes at 3 years was 23.9, 29.6, and 38.8% in the STH, DES, and control groups, respectively. On the basis of these rates, the number needed to treat to prevent one case of diabetes was seven (95% CI 5–11) in the STH group and 11 (95% CI 8–16) in the DES group over 3 years.
Figure 1.
Cumulative incidence of diabetes according to study group. The diagnosis of diabetes was based on the 2003 criteria of the American Diabetes Association. The incidence of diabetes differed significantly among the three groups (P < 0.01 for each comparison). Full line, STH group; dotted line, DES group; broken line, control group.
Fasting plasma glucose, 2-h OGTT plasma glucose, and A1C increased gradually in all three groups over the 3-year follow-up in comparison with baseline values (P < 0.01). Changes in the three parameters over the 3-year period were significantly different among the three groups (P < 0.01) (Fig. 2A–C).
Changes in body weight, waist circumference, and systolic blood pressure
Participants in the STH group showed a greater weight loss than those in the DES and control groups (Fig. 2D). The mean changes in weight at the 3-year follow-up were −2.1, −1.2, and +0.4 kg in the STH, DES, and control groups, respectively (P < 0.01). When we analyzed the incidence of diabetes adjusted by the change in body weight, there were no significant differences among three groups (STH vs. control P = 0.054; STH vs. DES P = 0.067; and DES vs. control P = 0.059).
Waist circumference increased in all groups over 3 years in comparison with the baseline values (P < 0.01). Changes in waist circumference over the 3-year period among the three groups were significantly different (P < 0.01) (supplemental Fig. 3A). There was no significant difference between the STH and DES groups in systolic blood pressure, but the values of the two groups were significantly lower than that in the control group (P < 0.01) (supplemental Fig. 3B).
Changes in serum lipids (triglycerides and total, LDL, and HDL cholesterol)
Serum triglycerides increased gradually in all three groups over the 3-year follow-up in comparison with baseline values (P < 0.01). Changes in serum triglycerides over the 3-year period were significantly different among the three groups (P < 0.01).
Total cholesterol of the control group increased significantly in comparison with baseline values (P < 0.01). On the other hand, that of the STH and DES groups decreased over the 3-year period. Changes in total cholesterol over the 3-year period were significantly different among the three groups (P < 0.01).
The decrease in LDL cholesterol at 6 months was significantly greater in the STH group than in the DES and control groups. However, at the end of the first year, there was no significant difference between the STH and DES groups, but the values of the two groups were significantly lower than that in the control group (P < 0.01).
HDL cholesterol of the control group decreased significantly in comparison with baseline values (P < 0.01), whereas that of the STH and DES groups increased significantly over the 3-year period. There was no significant difference between the STH and DES groups (supplemental Fig. 3C–F).
Cost benefits
From a health system perspective, the STH and DES groups cost $1,470 and $1,090 per patient, respectively, over 3 years. From a societal perspective, the STH and DES groups cost $21,800 and $26,350, respectively, for one case of diabetes prevented during each trial (15).
CONCLUSIONS
Our results showed that intervention of a 2-day in-hospital program with diabetes education and support every 3 months for participants with IGT could prevent or delay progression to type 2 diabetes. The annual incidence of diabetes in our IGT population in the control group was 13.2%, which was within the range suggested by epidemiological data (1.5–15.7%) (6,12,16–22). The data of the STH group, showing a reduced incidence of type 2 diabetes (42% reduction in 3 years), was slightly inferior to that in the DPP (58% in 2.8 years) and the Diabetes Prevention Study (DPS) (58% in 3.2 years), but was similar to that in the Da Qing study (31, 42, and 46% in 6 years) and was superior to that of the Malmö study (33% in 5 years) (6,12,16,17). Although the exact mechanism(s) of the outcome noted in our study after a 2-day in-hospital program is not clear at present, the reasons that we were able to achieve these results with such a program are as follows. Patients with high blood glucose levels and a diagnosis of IGT during a routine medical checkup often do not have sufficient knowledge about diabetes. However, through our 2-day in-hospital program, the participants had the opportunity to be instructed on a diabetic diet four times, to undergo various types of guidance classes and education seminars, and to receive enough information about diabetes and the risk of complications to boost motivation. At the first follow-up at 3 months after the beginning of the intervention, most participants’ body weight and laboratory data had improved, and they were praised for achieving that goal, which might have built their confidence and increased motivation. These results suggest that diabetes education and support every 3 months are probably sufficient for maintaining knowledge and motivation.
We observed a reduced incidence of diabetes in the STH and DES groups. At present, we propose a theoretical basis for this result. Our study showed that there were no significant differences in the incidence of diabetes after adjustment for the change in body weight. It indicated that the weight reduction mostly affected the incidence of diabetes. But the result was actually quite close to the criteria of P < 0.05 and indicated that another factor might also affect it. We found weight reduction to be −4.3% at 1 year and −2.3% at 3 years in the STH group. However, our results were lower than those in the DPP (−6.9% at 1 year and −4.3% at 3 years) and DPS (−4.7% at 1 year and −3.9% at 2 years) (6,12). The DPP and DPS were more effective because the interventions were more intense and costly. On the other hand, our intervention is more reasonable and has a lesser, but significant, effect in reducing diabetes risk. In addition to the effect of the intervention program, we consider the possibility that ethnic background also affects the difference in weight reduction, as suggested by Chen et al. (23).
Several large-scale studies have indicated that lifestyle improvement is effective in prevention of diabetes, but in most studies this required intensive supervision and several staff and was costly (13,24). As direct and indirect medical costs in Japan may be different from those in the U.S. or other countries, because of how health care is financed in general among other issues, these cannot easily be directly compared. Because our program is more simplified and requires fewer staff than conventional studies, we speculate that the STH intervention may be able to save both personnel and training costs for one case of diabetes prevented compared with the DPP lifestyle intervention group or other conventional studies.
Starting treatment with glucose-lowering agents before the establishment of diabetes is another way of reducing progression to diabetes. However, this is problematic from the point of view of health insurance and compliance, which is often unfavorable when patients who are asymptomatic for a chronic disease are medicated (25,26). The system for health insurance may be different in various countries. For example, in Japan, the use of medications for IGT is not covered under the government-sponsored health insurance system, whereas educational hospitalization for IGT is. Although we realize that insurance limitations may exist in some countries, it would be desirable if the use of insurance for educational hospitalization for IGT was permitted.
The present study had several limitations. The most important of these was the open-label study design, but we used the PROBE design, which has great similarity to routine clinical practice. The sample of participants, from the Joetsu area of Japan, was geographically, racially, and ethnically limited. We speculated that the results of self-assessment about adherence to recommendations that showed no significant differences among the groups reflected the relative insensitivity of our assessment of diet and physical activity to measure change or differences in change between the intervention groups. In addition, the groups may have differed in various ways that may have biased the results, e.g., readiness for change, but we did not evaluate such factors.
In summary, we found in the present study that diabetes education and support every 3 months for participants with IGT could prevent or delay progression to type 2 diabetes from IGT. Furthermore, this program was more effective when a 2-day in-hospital program was added, which might improve the motivation and will of participants with IGT.
Supplementary Material
Acknowledgments
We thank Yuchi Naruse (Toyama University, Japan) and Hiroshi Mizuma (Chiba University, Japan) for the discussion on statistical analysis of study results.
Published ahead of print at http://care.diabetesjournals.org on 30 June 2008.
Clinical trial reg. no. UMIN000000911, www.umin.ac.jp.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C Section 1734 solely to indicate this fact.
References
- 1.King H, Aubert RE, Herman WH: Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care 21:1414–1431, 1998 [DOI] [PubMed] [Google Scholar]
- 2.DECODE Study Group: Glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria. Lancet 354:617–621, 1999 [PubMed] [Google Scholar]
- 3.Fujishima M, Kiyohara Y: Diabetes and cardiovascular disease prospective population survey in Japan: the Hisayama Study. Diabetes 45(Suppl. 3):S14–S16, 1996 [DOI] [PubMed] [Google Scholar]
- 4.Tominaga M, Eguchi H: Impaired glucose tolerance is a risk factor for cardiovascular disease, but not impaired fasting glucose: the Funagata Diabetes Study. Diabetes Care 22:920–924, 1999 [DOI] [PubMed] [Google Scholar]
- 5.Harris MI: Diabetes in America: epidemiology and scope of the problem. Diabetes Care 21(Suppl. 3):C11–C14, 1998 [DOI] [PubMed] [Google Scholar]
- 6.Knowler WC, Barrett-Connor E, Fowler SE: Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346:393–403, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herman WH, Hoerger TJ, Brandle M: The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance: Ann Intern Med 142:323–332, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus: Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 26:3160–3167, 2003 [DOI] [PubMed] [Google Scholar]
- 9.Hansson I, Hender T, Dahlöf B: Prospective randomised open blinded endpoint (PROBE) study: a novel design for intervention trials. Blood Press 1:113–119, 1992 [DOI] [PubMed] [Google Scholar]
- 10.Diabetes Treatment Guide Editing Committee: Diabetes Treatment Guide 2003–2004. Tokyo, Japan Diabetes Society, 2003
- 11.Food Exchange List Editing Committee: Food Exchange List for Diabetes Diet Therapy. Version 6. Tokyo, Japan Diabetes Society, 2002
- 12.Tuomilehto J, Lindstrom J, Eriksson J: Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344:1343–1350, 2001 [DOI] [PubMed] [Google Scholar]
- 13.Gold MR, Siegel JE, Russell LB: Cost-Effectiveness in Health and Medicine. New York, Oxford University Press, 1996
- 14.Diabetes Prevention Program Research Group: Cost associated with the primary prevention of type 2 diabetes mellitus in the Diabetes Prevention Program. Diabetes Care 26:36–47, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Diabetes Prevention Program Research Group: Within-trial cost-effectiveness of lifestyle intervention or metformin for the primary prevention of type 2 diabetes. Diabetes Care 26:2518–2523, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pan XR, Li GW, Hu YH: Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: the Da Qing IGT and Diabetes Study. Diabetes Care 20:537–544, 1997 [DOI] [PubMed] [Google Scholar]
- 17.Eriksson KF, Lindgärde E: Prevention of type 2 (non-insulin-dependent) diabetes mellitus by diet and physical exercise: the 6-year Malmö feasibility study. Diabetologia 34:891–898, 1991 [DOI] [PubMed] [Google Scholar]
- 18.Chiasson JL, Josse RG, Gomis R: Acarbose for prevention of type 2 diabetes mellitus the STOP-NIDDM randomised trial. Lancet 359:2027–2077, 2002 [DOI] [PubMed] [Google Scholar]
- 19.Harris MI: Impaired glucose tolerance-prevalence and conversion to NIDDM. Diabet Med 13:S9–S11, 1996 [PubMed] [Google Scholar]
- 20.King H: Study in Tanzania of IGT: effect of regression to the mean. Diabetes Care 15:114–115, 1992 [DOI] [PubMed] [Google Scholar]
- 21.Kadowaki T, Miyake Y, Hagura R: Risk factors for worsening to diabetes in subjects with impaired glucose tolerance. Diabetologia 26:44–49, 1984 [DOI] [PubMed] [Google Scholar]
- 22.Modan M, Karasik A, Halkin H: Effect of past and current body mass index on prevalence of glucose intolerance and type 2 non-insulin-dependent diabetes and on insulin response: the Israel study of glucose intolerance, obesity and hypertension. Diabetologia 29:82–89, 1986 [DOI] [PubMed] [Google Scholar]
- 23.Chen HS, Shaw CK, Tseng WP: Prevalence of diabetes mellitus and impaired glucose tolerance in Aborigines and Chinese in eastern Taiwan. Diabetes Res Clin Pract 38:199–205, 1997 [DOI] [PubMed] [Google Scholar]
- 24.Diabetes Prevention Program Research Group: The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care 25:2165–2171, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohenx JS: Adverse drug effects, complications, and initial dose of anti hypertensive drugs recommended by the Joint National Committee vs. Physicians Desk Reference. Arch Intern Med 161:880–885, 2001 [DOI] [PubMed] [Google Scholar]
- 26.Mitka M: DASH dietary plan could benefit many, but few hypertensive patients follow it. JAMA 298:164–165, 2007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.