Abstract
Primary total hip arthroplasties have reported success rates of greater than 95% in many series with a longer than 10-year follow-up. Revision total hip arthroplasty due to such factors as increased high-activity levels, younger patients undergoing the procedure and increasing life expectancy has become more prevalent. An understanding of the mechanisms and timing of total hip arthroplasty failure can direct efforts aimed at reducing revision rates. This study was conducted to evaluate the indications for revision hip arthroplasty and relate these to the time after the index primary hip arthroplasty. A review of all revision hip arthroplasties at two centres over a 6-year time period identified 225 patients who underwent 237 revisions. The overall mean time to revision was 83 months (range: 0–360 months). The cause of failure was aseptic loosening in 123 hips (51.9%), instability in 40 hips (16.9%) and infection in 37 hips (5.5%). When stratified into two groups (less than 5 years, more than 5 years after the index primary hip arthroplasty), 118 of 237 (50%) revisions occurred in less than 5 years, with 33% due to instability and 24% resulting from infection. The majority of the causes of failure within 5 years in these early revisions were instability and deep infection. The success of hip arthroplasty is likely to be compromized if technical aspects of the surgery for appropriate component positioning and critical protocols to minimise complications such as infection are not given the proper attention.
Résumé
A dix ans de recul moyen les prothèses totales de hanches ont un taux de 95% de réussite dans la plupart des séries. Les facteurs ayant entraînés une réintervention, de type révision dépendent du niveau d’activité des sujets, de leurs jeunes âges, et de l’augmentation de la durée de vie. La compréhension des mécanismes d’échecs des prothèses totales de hanche devrait permettre de réduire le taux de révision. Cette étude a pour but d’évaluer les indications de révisions des prothèses totales de hanche. Pour cela, ont été revus, dans deux centres, avec six ans de recul moyen 225 patients qui ont bénéficié de 237 révisions. Le temps moyen pour la révision a été de 83 mois (0 à 360 mois). La cause de l’échec a été le descellement aseptique 123 hanches (51.9%), instabilité sur 40 hanches (16.9%) et infection sur 37 hanches (5.5%). Si l’on reclasse ces patients en deux groupes à moins et plus de 5 ans, 118 des 237 révisions (50%) surviennent dans une période de moins de 5 ans, 33% sont dues à l’instabilité, 24% à l’infection. Les causes d’échecs majeures avant 5 ans avec révisions, sont donc l’instabilité de la hanche et les infections profondes. Le succès d’une arthroplastie totale de hanche passe donc par le bon positionnement des implants et le respect du protocole de façon à éviter les complications infectieuses.
Introduction
Primary total hip arthroplasty is often described as one of the greatest advances in healthcare of the 20th century [1–3]. At present, the success rates of total hip arthroplasty at 10 years or longer exceeds 95% survivorship in patients older than 75 years [2, 4, 5]. Increasingly more patients are undergoing total hip arthroplasty, and they are generally expected to maintain a higher level of activity. In addition, life expectancy has increased, which has placed an increasing demand on these arthroplasties [6–9]. For these reasons, even though this is a highly successful operation, the number of revision procedures is expected to increase in the near future.
Revision hip arthroplasty, which constitutes close to one quarter of all arthroplasties performed in the USA, places immense financial burden on healthcare and has a less favourable outcome than primary total hip arthroplasty [1]. Potential reasons for hip revisions can be stratified into three groups: patient-related factors, implant-related factors and failures related to inadequate surgical technique [3, 10, 11]. Osteolysis and aseptic loosening, resulting from the failure of bearing surfaces, are considered to be the most common reasons for revision hip arthroplasty [3, 4]. These are failures that occur relatively long after the primary implantation. Other causes of failure which occur at earlier times include implant-related problems, such as periprosthetic fractures [12, 13], delamination of the porous coating [11], or other manufacturing problems. Patient-related factors leading to the failure of total hip arthroplasty include co-morbidities such as sickle cell anaemia [14], poor bone quality [15], or other variables that may predispose the patient to infections or dislocation. Surgical technique may also affect the outcome of total hip arthroplasty. This technical influence may be greater than previously believed as many revisions are required because of recurrent dislocation, malpositioning of components, or other technical problems [16–18]. Various other factors, such as high body mass index, use of non-steroidal anti-inflammatory drugs (NSAIDs) and smoking, are still subject to controversy in terms of being potential causes of prosthetic failure [19–23].
A stratification of the different modes of failure in large populations of patients undergoing revision as related to the timing of the failure has rarely been described. The purpose of this study was to examine the causes of failure of total hip arthroplasties and to analyse these and other demographic parameters in relation to the time of the revision after the primary procedure.
Materials and methods
All patients who underwent revision total hip arthroplasty between January 1, 1996 and December 31, 2004 at two institutions were analysed. Patients were identified using a prospectively collected computerised database at each centre. Patients undergoing a revision of a bipolar implant or conversion of a fracture fixation to a hip arthroplasty and those undergoing a second or further revision were excluded. Sixteen hips were excluded because they followed a failure of bipolar arthroplasties or hemi-resurfacing arthroplasties.
Detailed demographic data for each patient were collected, including age at index hip arthroplasty, gender, primary diagnosis and time from index primary total hip arthroplasty to failure as well as the exact reason(s) for failure of arthroplasty. The data sources reviewed included peri-operative charts, operative notes, discharge summaries and relevant radiographs. The primary diagnosis was grouped into the following categories: osteoarthritis, inflammatory arthritis (including rheumatoid arthritis and ankylosing spondylitis), osteonecrosis, hip dysplasia, post-traumatic arthritis and a miscellaneous group of other causes (hip tumours, pigmented villonodular synovitis). For each hip, the reason for failure was classified into one of the following six categories: aseptic loosening, infection, instability, component failure, peri-prosthetic fracture, or pain. In 14 cases in which there were multiple reasons for the failure, the primary reason for failure was selected by a joint decision by three of the co-authors (MAM, IT, DB) and recorded.
The demographic data collected was subject to various stratifications. Age at time of the primary procedure and at time of revision arthroplasty was stratified into one of four categories: under 30 years, 30–50 years, 50–70, or 70 years or older. For further analysis, the patients were stratified into a group of patients under 50 of age or a group of patients 50 years or older.
Patient data was stratified on the basis of the time to failure, which was defined as the interval, in months, from the primary procedure to the revision. This was stratified initially into four groups: less than 2 years, 2–5 years, 5–10 years and more than 10 years. This was later stratified into two separate groups, less than 5 years and more than 5 years (which was the mean for the study).
All data were entered onto a spreadsheet to allow comparison between groups and the determination of the relationships between the different variables. A tabulation of the overall results for the five independent variables (age, diagnosis, gender, time to failure and reason for failure) was performed. These tabulated results were then stratified by analysing each variable in relation to the other four. Direct comparisons were made of data for the different age categories in terms of time to failure and reason for failure. The relationships between primary diagnoses, time to failure and reason for failure were also established.
Survivorship analysis was performed using Kaplan-Meier curves to determine the survival of the implant for each diagnosis. The starting point was the date of the index surgery (primary total hip arthroplasty) and the end point was the date of the revision surgery. Kaplan-Meier curves were used to determine the relationship between gender and failure, and between age at the time of index surgery and failure. The authors also used Kaplan-Meier curves stratified by indication for revision to determine whether they correlated with shorter or longer revision-free intervals.
The Breslow test and log rank test were used to analyse data. The Breslow test weights early events more heavily than later events, whereas the log rank test weights all failures equally, regardless of time of occurrence. Median, mean values and the probability of significance (p < 0.05) were determined with use of the SPSS statistical software package (SPSS, Chicago, Ill.).
Results
There were 225 patients (237 hips) in the study, 108 of whom were men (111 hips) and 117 women (126 hips). The mean age of the study group was 59 years (range: 24–89 years). The overall mean time to revision surgery was 83 months (range: 0–360 months). One hundred and twenty-three hips (51.9%) were revised because of aseptic loosening, 40 (16.9%) were revised due to instability and 37 (15.6%) were revised because of infection. Nineteen revisions (8%) were performed because of pain, 13 (5.5%) because of peri-prosthetic fracture and five (2.1%) because of component failure.
The mean time to failure for hips was the shortest – a mean of 64 months (range: 3–360 months) – in patients with a primary diagnosis of osteonecrosis and the longest – a mean of 148 months (range: 24–312 months) – for patients with inflammatory arthritis. Patients with a diagnosis of hip dysplasia, post-traumatic arthritis and primary osteoarthritis had intermediate mean times to failure of 83 months (range: 8–204 months), 73 months (range: 3–312 months) and 82 months (range: 0–300 months), respectively. The percentage of patients at each interval of time whose hips had failed is shown in Table 1. The table shows an increase in the incidence of aseptic loosening as a cause of failure as time progresses. For example, aseptic loosening was the cause of approximately 18% of revisions at less than 2 years; this increased to over 90% in hips that failed after 10 years. It is also evident that most of the failures occurring within the first 2 years can be attributed to joint instability and infection (57% of this group). These factors were less important in patients who underwent revision after 10 years (5.8%).
Table 1.
Relationship between cause of failurea and time to failure (time interval to revision)
| Time interval to revision | Number of hips requiring revision | Aseptic loosening (%) | Infection (%) | Instability (%) | Component failure (%) | Periprosthetic fracture (%) | Pain (%) |
|---|---|---|---|---|---|---|---|
| <2 years | 79 | 17.70 | 24 | 33 | 3.80 | 6.30 | 15.20 |
| 2–5 years | 39 | 46.20 | 10.30 | 25.60 | 0.00 | 5.10 | 12.80 |
| 5–10 years | 49 | 67.30 | 14.30 | 10.30 | 0.00 | 2 | 6.10 |
| >10 years | 70 | 90 | 5.80 | 0.00 | 0.00 | 2.80 | 1.40 |
| <5 years | 118 | 27.10 | 19.60 | 30.5 | 2.50 | 5.90 | 14.40 |
| >5 years | 119 | 80.70 | 9.20 | 4.20 | 0.00 | 2.50 | 3.40 |
| Total | 237 | 51.90 | 15.60 | 16.90 | 2.10 | 5.50 | 8 |
aCause of failure is given in the table as the percentage of the group
When the data on timing and mode of failure were further stratified into two groups with a mean time to failure of less than 5 years versus 5 years or longer, approximately one-half of the hips (118 of 237) that were revised had survived less than 5 years. Differences were also noted between the causes of failure for the two groups (Table 1). The major cause of failure after 5 years was aseptic loosening.
The relationship between primary diagnosis and mechanism of failure is shown in Table 2. This analysis illustrated higher rates of failure by aseptic loosening in the inflammatory arthritis (75%) and hip dysplasia (60%) groups versus the osteonecrosis (41.9%) and osteoarthritis groups (50.5%). The results reflect the longer mean time to failure in these groups. There was a markedly higher rate of failure by instability in the osteonecrosis group, which paralleled the higher incidence of early revisions in this group.
Table 2.
Relationship between cause of failurea and primary diagnosis
| Diagnosis | Number of hips requiring revision | Causes of failure | |||||
|---|---|---|---|---|---|---|---|
| Aseptic loosening (%) | Infection (%) | Instability (%) | Component failure (%) | Peri-prosthetic fracture (%) | Pain (%) | ||
| Osteoarthritis | 111 | 56 (50.5) | 24 (21.6) | 17 (15.3) | 2 (1.8) | 9 (8.1) | 4 (3.6) |
| Inflammatory arthritis | 20 | 15 (70) | 2 (10) | 1 (5) | 0 (0.0) | 2 (10) | 0 (0.0) |
| Osteonecrosis | 62 | 26 (41.9) | 6 (9.7) | 13 (21) | 2 (3.2) | 1 (1.6) | 14 (22.6) |
| Dysplasia | 25 | 15 (60) | 1 (4) | 6 (24) | 1 (4) | 1 (4) | 1 (4) |
| Post-traumatic arthritis | 14 | 6 (42.9) | 6 (42) | 4 (28.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Other | 5 | 5 (100) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
aCause of failure is given in the table as the number of hips, with the percentage given in parentheses
The relationship between time of revision and diagnosis is shown in Table 3. The highest proportion of early revisions occurred in the post-traumatic arthritis (57.1%) and osteonecrosis groups (53.2%). The lowest proportion of early revisions (10%) and the largest proportion of late revisions occur in the inflammatory arthritis group (55%). While the revision of osteoarthritic hips is represented evenly throughout the time interval, revision of hips replaced for inflammatory arthritis is concentrated after 10 years.
Table 3.
Relationship between primary diagnosis and timing of revisiona
| Diagnosis | Number of hips requiring revision | Timing of revision | |||
|---|---|---|---|---|---|
| <2 years (%) | 2–5 years (%) | 5–10 years (%) | >10 years (%) | ||
| Osteoarthritis | 111 | 27 (24.3) | 27 (24.3) | 24 (21.6) | 33 (29.8) |
| Inflammatory arthritis | 20 | 2 (10) | 0 (0.00) | 7 (35) | 11 (55) |
| Osteonecrosis | 62 | 33 (53.2) | 9 (14.5) | 8 (12.9) | 12 (19.4) |
| Dysplasia | 25 | 9 (36) | 2 (8) | 7 (28) | 7 (28) |
| Post-traumatic arthritis | 14 | 8 (57.1) | 0 (0.00) | 2 (14.3) | 4 (28.6) |
| Other | 5 | 0 (0.00) | 1 (20) | 1 (20) | 3 (60) |
| Total | 237 | 79 (33.3) | 39 (16.5) | 49 (20.7) | 70 (29.5) |
aCause of failure is given in the table as the number of hips, with the percentage given in parentheses
There was an increase in the mean time to failure as the age of the patient increased. The mean time to failure for patients under 30 years of age at the time of revision was 25 months; for patients between 30 and 50 years of age, the mean time to failure was 65 months, and for patients aged 50–70 years, the mean time was 82 months. In the oldest group (patients over 70 years), the mean time to failure was 99 months.
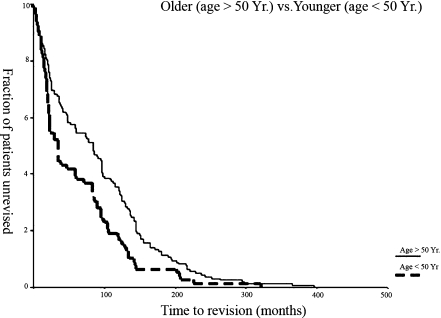
Kaplan-Meier survival curves were compared for several grouping factors. Survival curves based on gender were not statistically significantly different (Breslow statistic = 0.70, p = 0.40). Survival curves based on age at index surgery between the younger (less than 50 years old) and older (more than 50 years old) groups were significantly different (Breslow statistic = 8.26, p = 0.0040; log rank statistic = 8.61, p = 0.0033). The younger group had earlier failure that required revision surgery. The mean survival time to failure in the younger group was 63 months [95% confidence interval (CI): 49–77 months], whereas mean survival time for failure in the older group was 91 months (95% CI: 79–103 months) (Fig. 1).
Fig. 1.
Results of the Kaplan-Meier survivorship analysis for the patients younger and older than 50 years of age, respectively
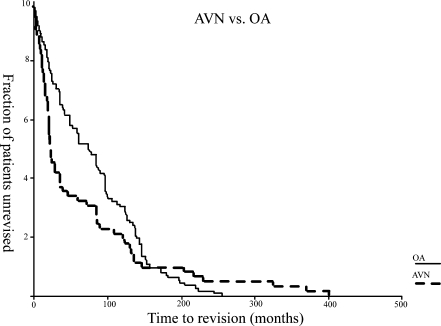
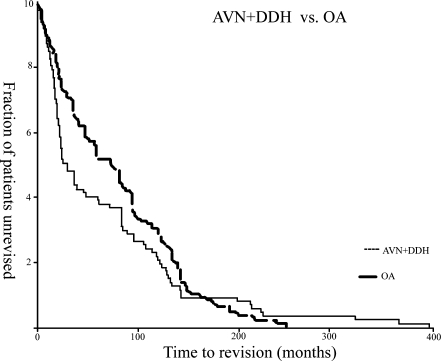
Survival curves based on diagnosis at the index surgery in terms of osteoarthritis and osteonecrosis are shown in Fig. 2. The differences between these two diagnoses are significantly different (Breslow statistic = 8.76, p = 0.0031), with patients with osteonecrosis requiring earlier revision surgery. The mean survival time for failure in the osteonecrosis group was 66 months (95% CI: 44–87 months), whereas, the mean survival time for failure in the osteoarthritis group was 81 months (95% CI: 69–92 months). Age at the time of index surgery may be one explanation for these results: mean age of the osteonecrosis group was 48 years (SE = 1.53, SD = 12.02), while the mean age of the osteoarthritis group was 67 years (SE = 1.049, SD = 11.10). When the osteonecrosis and hip dysplasia groups were analysed together as a similar group (because of the younger age at the time of primary total hip replacement) and compared to the osteoarthritis group (who were older when they underwent primary total hip arthroplasty), the survival curves (Fig. 3) were significantly different (Breslow statistic = 5.57, p = 0.0182)., with the patients with a diagnosis of osteonecrosis or hip dysplasia at index surgery having earlier revisions. The Mean survival time in this combined osteonecrosis and hip dysplasia group was 70 months (95% CI: 53–87 months), and the mean survival time in the osteoarthritis group was 81 months (95% CI: 69–92 months). Age at the time of the index surgery may be one explanation for these results.
Fig. 2.
Results of the Kaplan-Meier survivorship analysis for the osteonecrosis (=AVN, avascular necrosis ) and osteoarthritis (OA) groups
Fig. 3.
Results of the Kaplan-Meier survivorship analysis for osteonecrosis (AVN) in relation to the development of disorders of the hip (DDH) and osteoarthritis (OS)
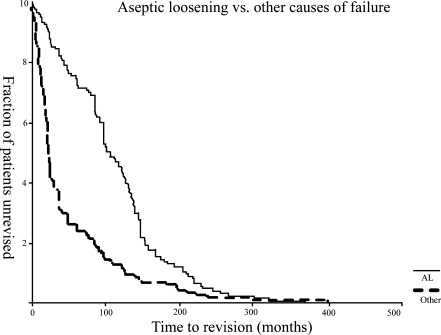
Aseptic loosening was the most common cause of total hip arthroplasty failure in our study. A comparison of the survival curves based on the cause of failure at revision surgery in terms of aseptic loosening and other groups revealed a significant difference (Breslow statistic = 67.10, p = 0.00; log rank statistic = 39.14, p = 0.00. This is shown in Fig. 4. Other causes of failure, such as instability and infection, led to revision surgery earlier than aseptic loosening. The mean survival time for failure due to aseptic loosening was 112 months (95% CI: 100–125 months), whereas mean survival time to failure due to other causes was 50 months (95% CI: 38–62 months).
Fig. 4.
Results of the Kaplan-Meier survivorship analysis for aseptic loosening (AL) and other causes of failure
No significant correlation between the initial diagnosis at index surgery and causes of failure was found. In addition, no significant correlation between age at primary surgery (younger than 50 years and older than 50 years) and cause of failure was found. The older group was most likely to fail because of aseptic loosening, while the younger group failed due to a variety of other causes.
Discussion
This study revealed that half of the hips were revised within less than 5 years of the primary index total hip arthroplasty. The mode of failure of the implanted hips was dependent on the length of the time interval following the index surgery – more or less than 5 years. In the late group, the primary reason for revision was aseptic loosening, whereas for the early failures, instability and deep infection proved to be the most important causes. These early failures were often directly related to errors in surgical technique, such as component malposition, soft tissue laxity, or operative field inoculation with bacteria.
Aseptic loosening continues to represent the predominant mode of failure of hip arthroplasty, with 52% of the revision cases being performed for this reason alone. This result was expected and to an extent justifies the large research effort which is currently being expended to reduce this problem. Aseptic loosening of modern cementless prosthetic designs has been associated with the use of NSAIDs and excessive smoking [23, 24]. Malik et al. [20] reported on the effects of both NSAID usage and smoking on early aseptic loosening and found no statistical significance between these variables. However, when assessed in the context of the relatively small number of total hip arthroplasties that fail early by aseptic loosening, the importance of other causes of failure must be recognised. In particular, this study again emphasizes the importance of meticulous surgical technique to minimise the technical errors which can cause early failure. It is likely that a joint that fails early – after only a few months – may be much more devastating to the patient than one which eventually succumbs after 15 or more years of excellent clinical service. A hip which fails due to sepsis often creates a greater operative challenge for the revision surgeon than a joint which has failed because of aseptic loosening.
A review of the recent literature revealed several papers which have discussed reasons for revision total hip surgery. A summary of selected studies published since 2000 in which more than 50 hip revisions are discussed is shown in Table 4 [13, 25–32]. Most of these reports have focused on technical aspects of the revision or longevity, or outcome of the revision procedure. The time interval from the index arthroplasty to revision arthroplasty was not documented in these studies or most other reports of revision hip arthroplasty in the literature. This study has demonstrated the relationships that exist between the reasons for failure of hip replacements, the time to failure, the primary diagnosis and patient age.
Table 4.
Hip revision arthroplasty studies since 2000
| Author | Year | Number of hips | Findings related to revision in total hip arthroplasty |
|---|---|---|---|
| Lachiewicz et al. [10] | 2005 | 100a | • 38% (15%)c loosening components |
| • Loosening acetabular cup 22% {24%} | |||
| • Loose hemiarthroplasty 13% (6%) | |||
| • Infection 10% (7%) | |||
| • Loosening femoral comp 8% (22%) | |||
| • Periprosthetic fracture 2% (3%) | |||
| • recurrent dislocation 2% (16%) | |||
| • osteolysis poly wear 1% (7%) | |||
| Clohisy et al. [4] | 2004 | 439a | • 7% infection |
| • 5% for periprosthetic fracture | |||
| Weeder et al. [24] | 2002 | 188a | • 82% aseptic loosening |
| • 8% infection | |||
| • 5% periprosthetic fracture | |||
| • 14% instability | |||
| Lind et al. [11] | 2002 | 87b | • 83 aseptic loosening |
| • 4 infection | |||
| Ullmak et al. [22] | 2002 | 57b | • 59 aseptic loosening |
| • 3 infection | |||
| Bohm et al. [3] | 2001 | 129b | • 97 aseptic loosening |
| • 16 infection | |||
| • 13 periprosthetic fracture | |||
| Templeton et al. [21] | 2001 | 61b | • 56 aseptic loosening |
| • 2 instability | |||
| • 3 periprosthetic fracture | |||
| Crwaford et al. [5] | 2000 | 74b | • 4 instability |
| • 3 component failure |
aReasons for failure; given as a percentage of the group
bReason for failure; given as the number of patients
cPercentage of patients 10 years apart is given in parentheses
In their recent Insall Award paper, Sharkey et al. [33] analyse the causes of failure after total knee replacement. They report that 55.6% of 212 total knee revision arthroplasties were performed within 2 years of the index procedure, with many of these early failures being related to technical errors which gave rise to instability. This finding correlates closely with the results of our study in which 50% of the failures occurred within 5 years of the index procedure. Both these sets of results may demonstrate that many of the factors that cause early failure are surgeon-related.
It is recognised that there are limitations to this study. First, clinical outcomes were reviewed retrospectively. Next, the two centres in this study are tertiary referral centres that receive large numbers of patients specifically for revision surgery. Therefore, the proportion of early failure might be higher than expected in a general practice. Nevertheless, the reasons and times of these failures have been accurately tabulated. In addition, the authors did not further analyse the effect of various risk factors such as body mass index, smoking and the use of NSAIDS.
In conclusion, although total hip arthroplasty has become an extremely successful operation, a proportion of failures are inevitable. As the procedure has evolved, significant resources have been deployed to reduce the rate of failure attributable to implant design or manufacturing technique. It is the contention of these authors that surgeons must remain focused on the technical aspects of the procedure and vigilant for errors in surgical technique which can give rise to early failure.
References
- 1.Mahomed NN, Barrett JA, Katz JN, et al. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Jnt Surg Am. 2003;85-A(1):27–32. doi: 10.2106/00004623-200301000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Eisler T, Svensson O, Tengstrom A, et al. Patient expectation and satisfaction in revision total hip arthroplasty. J Arthroplasty. 2002;17(4):457–462. doi: 10.1054/arth.2002.31245. [DOI] [PubMed] [Google Scholar]
- 3.Wroblewski BM. Current trends in revision of total hip arthroplasty. Int Orthop. 1984;8(2):89–93. doi: 10.1007/BF00265830. [DOI] [PubMed] [Google Scholar]
- 4.Furnes O, Lie SA, Espehaug B, et al. Hip disease and the prognosis of total hip replacements. A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987–99. J Bone Jnt Surg Br. 2001;83(4):579–586. doi: 10.1302/0301-620X.83B4.11223. [DOI] [PubMed] [Google Scholar]
- 5.Older J. Charnley low-friction arthroplasty: a worldwide retrospective review at 15 to 20 years. J Arthroplasty. 2002;17(6):675–680. doi: 10.1054/arth.2002.31973. [DOI] [PubMed] [Google Scholar]
- 6.Kuster MS. Exercise recommendations after total joint replacement: a review of the current literature and proposal of scientifically based guidelines. Sports Med. 2002;32(7):433–445. doi: 10.2165/00007256-200232070-00003. [DOI] [PubMed] [Google Scholar]
- 7.Seyler TM, Mont MA, Ragland PS, et al. Sports activity after total hip and knee arthroplasty: specific recommendations concerning tennis. Sports Med. 2006;36(7):571–583. doi: 10.2165/00007256-200636070-00003. [DOI] [PubMed] [Google Scholar]
- 8.Mont MA, LaPorte DM, Mullick T, et al. Tennis after total hip arthroplasty. Am J Sports Med. 1999;27(1):60–64. doi: 10.1177/03635465990270011801. [DOI] [PubMed] [Google Scholar]
- 9.Meek RM, Allan DB, McPhillips G, et al. Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res. 2006;447:9–18. doi: 10.1097/01.blo.0000218754.12311.4a. [DOI] [PubMed] [Google Scholar]
- 10.Berry DJ, Harmsen WS, Cabanela ME, et al. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Jnt Surg Am. 2002;84-A(2):171–177. doi: 10.2106/00004623-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Ong A, Wong KL, Lai M, et al. Early failure of precoated femoral components in primary total hip arthroplasty. J Bone Jnt Surg Am. 2002;84-A(5):786–792. doi: 10.2106/00004623-200205000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Sarvilinna R, Huhtala HS, Puolakka TJ, et al. Periprosthetic fractures in total hip arthroplasty: an epidemiologic study. Int Orthop. 2003;27(6):359–361. doi: 10.1007/s00264-003-0493-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bohm P, Bischel O. Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Jnt Surg Am. 2001;83-A(7):1023–1031. [PubMed] [Google Scholar]
- 14.Vichinsky EP, Neumayr LD, Haberkern C, et al. The perioperative complication rate of orthopedic surgery in sickle cell disease: report of the National Sickle Cell Surgery Study Group. Am J Hematol. 1999;62(3):129–138. doi: 10.1002/(SICI)1096-8652(199911)62:3<129::AID-AJH1>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 15.Kobayashi S, Saito N, Horiuchi H, et al. Poor bone quality or hip structure as risk factors affecting survival of total-hip arthroplasty. Lancet. 2000;355(9214):1499–1504. doi: 10.1016/S0140-6736(00)02164-4. [DOI] [PubMed] [Google Scholar]
- 16.Phillips CB, Barrett JA, Losina E, et al. Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Jnt Surg Am. 2003;85-A(1):20–26. doi: 10.2106/00004623-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty : an analysis of risk factors and treatment options. J Bone Jnt Surg Am. 2002;84-A(10):1788–1792. [PubMed] [Google Scholar]
- 18.Parvizi J, Wade FA, Rapuri V, et al. Revision hip arthroplasty for late instability secondary to polyethylene wear. Clin Orthop Relat Res. 2006;447:66–69. doi: 10.1097/01.blo.0000218751.14989.a6. [DOI] [PubMed] [Google Scholar]
- 19.Ibrahim T, Hobson S, Beiri A, et al. No influence of body mass index on early outcome following total hip arthroplasty. Int Orthop. 2005;29(6):359–361. doi: 10.1007/s00264-005-0012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malik MH, Gray J, Kay PR. Early aseptic loosening of cemented total hip arthroplasty: the influence of non-steroidal anti-inflammatory drugs and smoking. Int Orthop. 2004;28(4):211–213. doi: 10.1007/s00264-004-0556-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McLaughlin JR, Lee KR. The outcome of total hip replacement in obese and non-obese patients at 10- to 18-years. J Bone Jnt Surg Br. 2006;88(10):1286–1292. doi: 10.1302/0301-620X.88B10.17660. [DOI] [PubMed] [Google Scholar]
- 22.Espehaug B, Havelin LI, Engesaeter LB, et al. Patient-related risk factors for early revision of total hip replacements. A population register-based case-control study of 674 revised hips. Acta Orthop Scand. 1997;68(3):207–215. doi: 10.3109/17453679708996686. [DOI] [PubMed] [Google Scholar]
- 23.Meldrum RD, Wurtz LD, Feinberg JR, et al. Does smoking affect implant survivorship in total hip arthroplasty? A preliminary retrospective case series. Iowa Orthop J. 2005;25:17–24. [PMC free article] [PubMed] [Google Scholar]
- 24.Persson PE, Nilsson OS, Berggren AM. Do non-steroidal anti-inflammatory drugs cause endoprosthetic loosening? A 10-year follow-up of a randomized trial on ibuprofen for prevention of heterotopic ossification after hip arthroplasty. Acta Orthop. 2005;76(6):735–740. doi: 10.1080/17453670510045309. [DOI] [PubMed] [Google Scholar]
- 25.Crawford SA, Siney PD, Wroblewski BM. Revision of failed total hip arthroplasty with a proximal femoral modular cemented stem. J Bone Jnt Surg Br. 2000;82(5):684–688. doi: 10.1302/0301-620X.82B5.10685. [DOI] [PubMed] [Google Scholar]
- 26.Templeton JE, Callaghan JJ, Goetz DD, et al. Revision of a cemented acetabular component to a cementless acetabular component. A ten to fourteen-year follow-up study. J Bone Jnt Surg Am. 2001;83-A(11):1706–1711. doi: 10.2106/00004623-200111000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Lind M, Krarup N, Mikkelsen S, et al. Exchange impaction allografting for femoral revision hip arthroplasty: results in 87 cases after 3.6 years’ follow-up. J Arthroplasty. 2002;17(2):158–164. doi: 10.1054/arth.2002.29391. [DOI] [PubMed] [Google Scholar]
- 28.Weeden SH, Paprosky WG. Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty. 2002;17(4 Suppl 1):134–137. doi: 10.1054/arth.2002.32461. [DOI] [PubMed] [Google Scholar]
- 29.Ullmark G, Hallin G, Nilsson O. Impacted corticocancellous allografts and cement for revision of the femur component in total hip arthroplasty. J Arthroplasty. 2002;17(2):140–149. doi: 10.1054/arth.2002.29397. [DOI] [PubMed] [Google Scholar]
- 30.Lachiewicz PF, Soileau ES. Changing indications for revision total hip arthroplasty. J Surg Orthop Adv. 2005;14(2):82–84. [PubMed] [Google Scholar]
- 31.Khatod M, Barber T, Paxton E, et al. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res. 2006;447:19–23. doi: 10.1097/01.blo.0000218752.22613.78. [DOI] [PubMed] [Google Scholar]
- 32.Clohisy JC, Calvert G, Tull F et al (2004) Reasons for revision hip surgery: a retrospective review. Clin Orthop Relat Res (429):188–192 [DOI] [PubMed]
- 33.Sharkey PF, Hozack WJ, Rothman RH et al (2002) Insall award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res (404):7–13 [DOI] [PubMed]