Abstract
Limb-saving therapy for primary bone tumours is the treatment of choice. We aimed at analysing the quality of life of this group of patients by combining three different tools. Eighty-seven patients (46 females, 41 males) with a primary bone tumour of the extremity who had undergone endoprosthetic reconstruction between 1982 and 2000 were included in this retrospective study. The median age at the time of evaluation was 30 (12–73) years. The Toronto Extremity Salvage Score (TESS) and the Reintegration to Normal Living index (RNL) were recorded an average of 5.8 years after reconstruction and the Musculoskeletal Tumour Society Score (MSTS) after an average of 6.5 years. The mean MSTS score was 77% (13–93%). The mean TESS was 82% (22–99%), and the mean RNL index was 87% (32–98%). The subjective satisfaction and acceptance of physical impairment were significantly higher than the objective score (p < 0.001). The TESS was 88% in patients aged 12–25 years, 81% in those aged 26–40 years and 57% in those aged 41–73 years. Parallel recording of the MSTS score, TESS and RNL index provides a better measure reflecting the complex situation of the patients by combining objective and subjective parameters.
Keywords: Bone tumour, Prosthetic replacement, Limb function, Quality of life, Outcome research
Résumé
La préservation du membre dans le traitement des tumeurs osseuses primitives des os doit être privilégiée. Le but de ce travail a été d’analyser la qualité de vie d’un groupe de patients dont le traitement a combiné différentes techniques. 87 patients (46 femmes et 41 hommes) présentant une tumeur primitive des extrémités osseuses et ayant bénéficié d’une endo prothèse entre 1982 et 2000 ont été inclus dans cette étude rétrospective. L’âge moyen au moment de l’évaluation des patients était de 30 ans (12 à 73 ans). Le score de Toronto ainsi que l’index RNL ont été utilisés en moyenne 5.8 ans après la reconstruction, de même que le score de la Société des Tumeurs Musculo-squeletiques. A à 6.5 ans en moyenne après le traitement. Le score MSTS moyen était de 77% (13 à 93%). Le score moyen TESS était de 82% (de 22 à 99%) et l’index RNL était de 87% (de 32 à 98%). La satisfaction des patients a été significativement plus élevée que l’évolution objective (p < 0.001). Le TESS était de 88% pour les patients âgés de 12 à 25 ans, de 81% chez les patients âgés de 26 à 40 ans et de 57% chez les patients plus âgés (de 41 à 73 ans). L’analyse des scores MSTS, TESS et de l’index RNL permet de mieux analyser les situations complexes de ces patients tant sur le plan objectif que subjectif.
Introduction
Limb-saving therapy has become the treatment of choice in primary bone tumours during the past decades. Reconstructive procedures as part of a multidisciplinary treatment concept have abolished primary amputation without compromising survival and local recurrence-free survival [12, 18]. Beyond survival, there is little information on physical impairment and disability [13–15, 20], but evaluation of the functional outcome is becoming increasingly important in the increasing proportion of long-term survivors.
This target group comprises mainly adolescents and young adults. Prolongation of survival resulted in subsequent surgical revisions of the implant and exchange operations as a result of endoprosthesis complications. These include periprosthetic infections, aseptic and septic loosening, and wear of the joint components, dislocations and fatigue fractures. The long-term outcome along with the oncological outcome is also determined by therapy-associated (late) complications. Another aspect is the functional result after limb-sparing surgery. When the complex medical treatment is finished, patients often must accept physical disability after implantation of a tumour endoprosthesis, which can lead to long-term impairment in the personal and social sphere [12, 18].
The aim of this study was to obtain a standardised evaluation and comparison of the functional long-term outcome of patients with primary bone tumours who were treated by means of an endoprosthesis, using independent scoring systems: the doctor-based MSTS score of the Musculoskeletal Tumour Society, the patient-oriented TESS (Toronto Extremity Salvage Score), and the RNL index (Reintegration to Normal Living).
Patients
The analysis included 87 consecutive patients with a primary bone tumour who had limb-sparing reconstruction with a tumour endoprosthesis between 1982 and 2000. The data were collected between September 1999 and December 2000. The median age at the time of operation was 20 (11–67) years, and at time of evaluation 30 (12–73) years. There were 41 male and 46 female patients. The MSTS score was recorded a median of 6.5 (0.5–17.2) years postoperatively, and the TESS/RNL index was recorded 5.8 (0.5–16.5) years postoperatively. With regard to the tumour type, osteosarcoma was the most common tumour at 61% (n = 53) (Table 1). Tumours were located in the lower limb in 78 patients (89.7%) and in the upper limb in 9 patients (10.3%). In the endoprosthetic reconstruction, distal femur replacement predominated at 47.1% (n = 41), followed by proximal tibia replacement (Table 1). Twenty-five patients who underwent revision due to endoprosthesis failure (loosening, infection, loosening, and mechanical failure) were not analysed separately, since they were evenly distributed among the overall population. The most common endoprosthetic-related complication was infection (early and late) in 13 patients (14.9%), followed by mechanical failure (e.g., fracture of the endoprosthesis) in 6 patients (6.9%), loosening in 4 patients (4.6%), and traumatic shaft fractures of the involved bone in 2 patients (2.3%). All endoprosthetic-related complications were treated surgically. A replacement of the endoprosthesis was performed in 21 of these 25 patients.
Table 1.
Histological classification of primary bone tumours and endoprosthetic reconstructions (n = 87)
| n | % | |
|---|---|---|
| Histological classification of primary bone tumours (n = 87) | ||
| Osteosarcoma | 53 | 61 |
| Chondrosarcoma | 14 | 16.1 |
| Giant cell tumour | 9 | 10.4 |
| Malignant fibrous histiocytoma | 5 | 5.7 |
| Ewing sarcoma | 4 | 4.6 |
| Leiomyosarcoma | 1 | 1.1 |
| Alveolar cell sarcoma | 1 | 1.1 |
| Total | 87 | 100 |
| Tumour endoprostheses (n = 87) | ||
| Distal femur replacement | 41 | 47.1 |
| Proximal femur replacement | 4 | 4.6 |
| Total femur replacement | 6 | 6.9 |
| Proximal tibia replacement | 27 | 31 |
| Proximal humerus replacement | 8 | 9.2 |
| Total humerus replacement | 1 | 1.1 |
| Total | 87 | 100 |
The various types of endoprostheses (Link® 1982–1993, Howmedica® 1993–1999, Mutars® since 1999), cemented or cement-free implantation, were not separately analysed. The patients in this analysis did not develop local recurrences. Furthermore, the various multimodal therapies were ignored.
Methods
The MSTS score (Musculoskeletal Tumour Society Score [5]) evaluates the functional condition (impairment) after completed tumour treatment. It is calculated on the basis of a standardised physical examination by the physician. This clinical examination assesses six criteria and differs slightly between the upper and lower limb. For the lower limb the components are pain, function, emotional acceptance of the treatment outcome, need for walking aids, walking and gait. For all criteria, the estimate is made from bad to very good with parallel awarding of points (0 to 5). There is thus a numerical value for each of the six criteria. These six values are added and divided by the maximum possible number of points (30). The percentage value is obtained by multiplying the calculated point value by 100.
Two questionnaires were used to record the patients’ self-assessment. The TESS (Toronto Extremity Salvage Score) was developed to record the physical and functional impairment in daily life (disability) with the intention of describing individuals at a certain point in time and in the event of changes [2–4]. As a disease-specific measurement method, it was developed for patients aged between 12 and 80 years. The TESS was developed as a measure of physical function. It comprises restrictions in mobility, in personal care and in carrying out activities of daily life. Physical function, as described in the TESS, is classified according to the International Classification of Impairments, Disabilities, and Handicaps (ICIDH) [23, 24]. Patients require about 40 min to complete the questionnaire. After the point score has been obtained, the percentage is calculated.
The RNL index (Reintegration to Normal Living index) is used for personal assessment of handicap in daily life [22]. It is a measurement instrument (questionnaire) for evaluating the consequences of a disease and the required therapy on the patient’s life. “Reintegration to normal living” is defined as the reorganisation of the physical, mental and social characteristics of an individual into a harmonious whole. To complete the RNL questionnaire takes about 10 min. A percentage value is calculated so that a comparison can be made. The RNL index was not completed by 10 patients so that the analysis refers to 77 patients. The MSTS score was calculated during follow-up examinations between September 1999 and December 2000. The questionnaires used to determine the TESS and RNL index were sent by post to the patients, who filled them out at home and sent them back to the clinic using a post-paid envelope. This led to the timely difference between the evaluation of the MSTS scores and that of the TESS and RNL index.
Statistical analysis was performed using SPSS (Statistical Package for the Social Sciences, Version 9.0). The group comparison was made by means of confirmatory analysis. For the statistical analysis the parameter-free rank analysis of variance with repeated measurements according to Brunner (SAS) followed by non-parametric tests as post hoc test with two linked samples (Wilcoxon test) and two independent samples (Mann-Whitney test) was used. The Pearson chi-square test was used to analyse nominally scaled data. Significance levels were also determined [1, 7].
Results
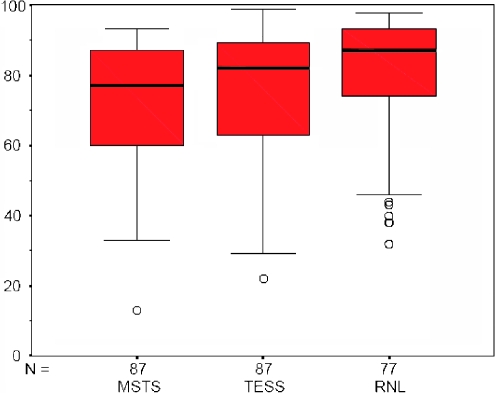
A median MSTS score of 77% (13–93%), a median TESS of 82% (22–99%) and a median RNL index of 87% (32–98%) were obtained for all patients. There were significant differences between the MSTS score and the RNL index (p = 0.002) and between the TESS and RNL index (p = 0.011). The self-assessment of physical disability (TESS) was markedly better (p < 0.001) than the objective evaluation of the functional outcome (MSTS score) (Fig. 1). Gender-specific differences were not found in the MSTS score, TESS and RNL index.
Fig. 1.
Box plot of overall MSTS score, TESS and RNL index
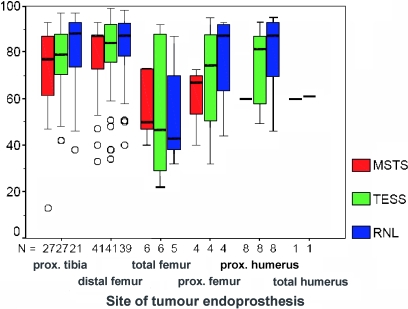
Tumour site
In the lower limb, the highest values of the MSTS score and TESS were obtained after insertion of a distal femur endoprosthesis, followed by proximal tibia and then by proximal and total femur replacement (Fig. 2). In order to evaluate the influence of tumour site on the functional outcome, the two most frequently implanted tumour endoprostheses (distal femur replacement, n = 41 and proximal tibia replacement, n = 27) were used. The two patient groups did not differ with regard to gender (p = 0.328) or age distribution (p = 0.384). There was no significant difference between the two patient groups (p = 0.206) with regard to the MSTS score, TESS and RNL index (Table 2). If only the proximal tibia replacement is considered, there is a significant difference when the three scores are compared (p = 0.004), whereas there was only a tendency to differences (p = 0.063) with distal femur replacement (Fig. 2). Patients with proximal humerus replacement (n = 8) showed an MSTS score of 60%, a median TESS of 81.5% and an RNL index of 87%. Because of the small number, a significance level was not calculated.
Fig. 2.
Box plot of MSTS score, TESS and RNL index related to the site of tumour endoprosthesis
Table 2.
MSTS score, TESS and RNL index related to the site of tumour endoprostheses
| MSTS score, TESS and RNL index related to the site of tumour endoprostheses | MSTS score, TESS and RNL index related to age | ||||
|---|---|---|---|---|---|
| Proximal tibia (n = 27)% | Distal femur (n = 41)% | 12–25 years (n = 32) | 20–40 years (n = 33) | 41–73 years (n = 22) | |
| MSTS score | 77 (13–93) | 87 (33–93) | 80% (13–90%) | 80% (47–93%) | 61.5% (33–87%) |
| TESS | 79(42–97) | 84 (34–99) | 88% (42–99%) | 81% (22–93%) | 57% (29–98%) |
| RNL index | 88 (38–97) | 87 (40–98) | 92% (46–97%) | 87% (38–95%) | 83% (32–98%) |
Patient age
To detect age-specific differences, three age classes were formed: group 1, 12–25 years (n = 32); group 2, 26–40 years (n = 33) and group 3, 41–73 years (n = 22). In group 1, the MSTS score differed significantly from the TESS (p < 0.001). In group 3, the MSTS score differed significantly from the RNL index (p = 0.011) and the TESS from the RNL index (p = 0.008). There were no significant differences between the scores of the patients in group 2. Significant differences were found in both the MSTS score (p = 0.006), TESS (p = 0.001) and RNL index (p = 0.047) when the youngest and oldest groups of patient were compared. The patients in group 2 and 3 showed significant differences in the MSTS score (p = 0.003) and TESS (p = 0.005), but not in the RNL index (Table 2).
There is also a tendency towards these results when the occupational activities in the three age-related patient groups are analysed. In group 1, 93.7% are still receiving education or are working full-time or part-time, 51.7% in group 2 and only 27.2% in group 3. The proportion of occupational disability and unfitness for work follows an opposite course: it is 0% in group 1 and 63.6% in group 3 (Table 3). There were no gender-specific differences in the MSTS score, the TESS and the RNL index.
Table 3.
Vocational situation related to the age (n = 87)
| 12–25 years (n = 32) | 20–40 years (n = 33) | 41–73 years (n = 22) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Full-time employed | 7 | 21.9 | 13 | 39.4 | 5 | 22.7 |
| Part-time employed | 1 | 3.1 | 2 | 6.1 | 1 | 4.5 |
| Unemployed | 2 | 6.3 | 4 | 12.1 | 0 | 0 |
| Student/apprentice | 22 | 68.7 | 2 | 6.1 | 0 | 0 |
| Retiree | 0 | 0 | 0 | 0 | 2 | 9.1 |
| Disabled | 0 | 0 | 9 | 27.2 | 14 | 63.6 |
| Not applicable | 0 | 0 | 3 | 9.1 | 0 | 0 |
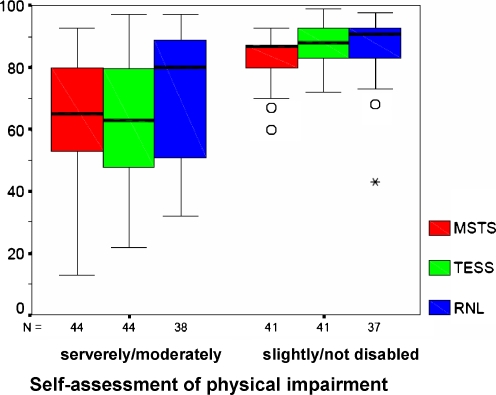
Self-assessment of disability
Of the 87 patients, 4.6% assessed themselves as not disabled, 42.5% as slightly disabled, 26.4% as moderately disabled and 24.1% as severely disabled. Two patients did not respond to this question (2.3%). A more detailed analysis was conducted in two groups. Group 1 includes the patients who feel themselves to be severely or moderately disabled and group 2 represent those patients who feel slightly or not at all disabled. Both patient groups differed significantly in the MSTS score, TESS and RNL index (p < 0.001). In group 1 (severely/moderately disabled) significant differences were found between the MSTS score and the RNL index (p = 0.044) on the one hand and between the TESS and RNL index (p = 0.003) on the other (Fig. 3). Within group 2 (slightly/not at all disabled) significant differences were also found between the MSTS score and TESS (p < 0.001) and between the MSTS score and RNL index (p = 0.039). When the occupational situation was taken into account, these results were corroborated. Of the patients, 46.5% who felt severely or moderately disabled were unfit for work, while only 7.5% of the patients in the other group (slightly/not at all disabled) were unfit for work (p < 0.001).
Fig. 3.
Box plot of MSTS score, TESS and RNL indexes related to the self-assessment of physical impairment
Discussion
The assessment of a treatment outcome can be made at the most varied levels (physical, mental, cosmetic, social, etc.). With the International Classification of Impairment, Disability and Handicap (ICIDH), the WHO has defined the complex concept of disability. The anatomical damage (impairment) is distinguished from functional impairment (disability) and social disadvantage (handicap) [23, 24]. Following this, it is apparent that the MSTS score reflects mainly impairment, the TESS disability and the RNL index handicap. While the MSTS score assesses the anatomical situation (impairment) in particular, the TESS evaluates the functional impairment (disability) and the RNL index the social component.
Hitherto, analysis of the functional outcome was performed mainly in the comparison of limb sparing surgery versus amputation and also in comparison with rotationplasty in patients with primary malignant bone tumours [9, 12, 25]. The type of surgery has no influence on quality of life and subjective well-being after lower extremity sarcomas [25]. Thus, the decision for either limb-sparing surgery or amputation cannot be based on quality of life and subjective well-being, but must be determined by oncological criteria [25]. An attempt to compare an objective (doctor’s) assessment with the patients’ self-assessment was made much more rarely. The TESS system was validated along with the MSTS and subsequently has been used to analyse these complex problems [2, 4].
In general, all of our patients with objective anatomical deficits were well integrated socially, and the functional impairment of the affected limb was also assessed as good. The age of the patients at the time of the disease depended on the tumour type and corresponded to the known distribution. Osteosarcomas and Ewing sarcomas occur predominantly in children and adolescents and are treated by combined modality therapy including high dose chemotherapy. Chondrosarcomas can be expected in the second half of life and mainly are treated by surgical resection without preoperative chemotherapy. The three scoring systems were analysed according to the criteria of gender, tumour site, age and self-assessment of disability. The tumour type was not taken into account as the different results in the scores could have been attributed to the age of predilection of the various primary bone tumours.
No gender-specific differences were found in the three scores. This result can most probably be explained by the equal social status.
When the two large patient groups with distal femur replacement and proximal tibia replacement were compared, no difference was found in the TESS or RNL index. In the MSTS score a tendency in favour of patients with distal femur replacement was identified. Gait was better in patients with distal femur replacement than after proximal tibia replacement. This result can be attributed to the anatomical situation. In the case of proximal tibia replacement it is necessary to reconstruct the extensor apparatus. In most cases a uni- or bilateral gastrocnemius flap on the ipsilateral side is used. The anteriorised gastrocnemius flap is sutured to the patellar ligament. Apart from the increased operative complexity, postoperative rehabilitation is prolonged. Active and passive flexion in the affected knee is permitted only after the fourth postoperative week. This result is confirmed when the TESS is considered. Patients with a proximal tibia replacement felt functionally impaired in daily life more often. Similar results on comparing the MSTS score in patients with distal femur replacement and proximal tibia replacement were obtained by Ritschl et al. [16], Wittig et al. [21], Kawai et al. [11], Gerrand et al. [8] and Rompen et al. [17]. Only Fabroni et al. [6] reported that patients with a proximal tibia replacement have a better functional outcome compared to distal femur replacement. This can probably be explained by the small number of cases. Malo et al. [13] showed that the MSTS score was 80.4% and the TESS was 81.4% in 56 patients with a distal femur replacement. This corresponds to our results in 41 patients (MSTS score 87%, TESS 84%).
The lowest MSTS score was observed in patients with proximal and total femur replacement due to the poorer muscle status on the one hand and reconstruction of two corresponding joints in the case of total femur replacement on the other hand. The functional outcome can hardly be influenced positively even by using a connecting tube in proximal and total femur replacement. McGoveran et al. [14] reported an MSTS score of 58.3%, and Ilyas et al. [10] of 63.3% following proximal femur replacement nicely matching our results with 67%.
The low MSTS score after proximal humerus replacement results from the markedly impaired function of the shoulder joint. Reconstruction of shoulder joint function is not possible because of the resection of the rotator cuff muscles and division of the subscapularis, deltoid, pectoralis major muscles, etc., in order to leave a layer of muscle covering the tumour. In addition, in endoprosthetic reconstruction of the proximal humerus, arm shortening of 1–2 cm is accepted in order to allow tension-free closure of the soft tissue and reduce the risk of dislocation of the endoprosthesis. These endoprostheses have predominantly a spacer function when function in the elbow and wrist is preserved. Our results are similar to those of Shin et al. [19] and Fabroni et al. [6]. In contrast, Wittig et al. [21] obtained an MSTS score of 80–90% in 15 patients with a proximal humerus replacement. In our patients, the categories “function”, “emotional acceptance” and “ability to raise” in particular were assessed more poorly, leading to an MSTS score of 60% only. This difference is attributable less to different functional outcomes than rather to differences in interpretation by the investigator.
The age grouping was oriented to the occupational situation. Patients in the 12–25 years age group assessed themselves better in the TESS and RNL index than they were assessed in the MSTS score. This result can be attributed to the fact that the young patients demonstrate better adaptation to a changed physical situation and have learned to live with their disability. The patients in the >40 years age group were assessed worse in the MSTS score on the one hand and they also assessed themselves more poorly in the TESS than in the RNL index. This observation indicates that the patients have deficits at the level of both impairment and disability, which play hardly any part in the consideration of social integration. The RNL index differs clearly in comparison with the youngest age group, but not in comparison with the 26–40 years age group. The worse MSTS score of the patients in the >40 years age group is complex. The causes could be attributed to concomitant degenerative disease requiring treatment, lower motivation and less intensive rehabilitation. These patients required analgesia and walking aids more often and reported more rapid fatigue and tiredness.
The patients’ self-assessment (TESS, RNL index) yielded better results through all subgroups than the assessment by a physician’s clinical examination (MSTS score). These differences can be interpreted on the one hand as different perception by patient and physician. On the other hand, the better results of the self-assessment can be attributable to acceptance and coming to terms with the postoperative situation. The patients who assessed themselves as moderately or severely disabled showed markedly better results in the RNL index than in the MSTS score or TESS. The time of evaluation of the TESS and RNL index was not included in this analysis, since this problem affects the entire group of patients. This indicates that these patients can integrate well into normal life despite functional impairments. The patients who felt themselves to be slightly or not at all disabled achieved better results in the RNL index and in the TESS than in the MSTS score. This can be attributed to the fact that it is easier in both the TESS and in the RNL index to obtain more points in the upper region of the scale compared to the MSTS score. The categories “function” and “emotional acceptance” of the MSTS score can lead to a subtraction of points without the patient having to demonstrate severe functional disadvantages. These observations were also confirmed by Davis et al. [2].
By using the combined MSTS score, TESS and RNL index, we could demonstrate that despite functional anatomical impairments after endoprosthetic management of bone tumours of the limbs, physical disability is perceived to only a small degree by the patients. Parallel recording of the MSTS score, the TESS and the RNL index allows much better evaluation of the quality of life after limb-sparing surgery taking into account tumour site and patient age. Without the use of a self-rating scale of the patient, ‘objective’ measurements by the physician tend to overestimate anatomical impairment. Combining different tools for outcome assessment provides an improved understanding of the often complex post therapeutic situation of our patients.
References
- 1.Cox DR, Snell EJ. Applied statistics: Principles and examples. London: Chapman and Hall; 1981. [Google Scholar]
- 2.Davis AM, Bell RS, Badley EM, Yoshida K, Williams JI. Evaluating functional outcome in patients with lower extremity sarcoma. Clin Orthop. 1999;358:90–100. [PubMed] [Google Scholar]
- 3.Davis AM, Devlin M, Griffin AM, Wunder JS, Bell RS. Functional outcome in amputation versus limb sparing of patients with lower extremity sarcoma: a matched case-control study. Arch Phys Med Rehabil. 1999;80(6):615–618. doi: 10.1016/S0003-9993(99)90161-2. [DOI] [PubMed] [Google Scholar]
- 4.Davis AM, Wright JG, Williams JI, Bombardier C, Griffin A, Bell RS. Development of a measure of physical function for patients with bone and soft tissue sarcoma. Qual Life Res. 1996;5(5):508–516. doi: 10.1007/BF00540024. [DOI] [PubMed] [Google Scholar]
- 5.Enneking WF, Dunham W, Gebhardt MC, Malawer M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop. 1993;286:241–246. [PubMed] [Google Scholar]
- 6.Fabroni RH, Castagno A, Aguilera AL, Steverlynck AM, Zeballos J. Long term results of limb salvage with the Fabroni custom made endoprosthesis. Clin Orthop. 1999;358:41–52. [PubMed] [Google Scholar]
- 7.Feinstein AR. Clinimetric perspectives. J Chronic Dis. 1987;40(6):635–640. doi: 10.1016/0021-9681(87)90027-0. [DOI] [PubMed] [Google Scholar]
- 8.Gerrand CH, Currie D, Grigoris P, Reid R, Hamblen DL. Prostetic reconstruction of the femur for primary bone sarcoma. Int Orthop. 1999;23(5):286–290. doi: 10.1007/s002640050373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hillmann A, Hoffmann C, Gosheger G, Krakau H, Winkelmann W. Malignant tumor of the distal part of the femur or the proximal part of the tibia: endoprosthetic replacement of rotationplasty. Functional outcome and quality-of-life measurements. J Bone Joint Surg (Am) 1999;81(4):462–468. doi: 10.2106/00004623-199904000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Ilyas I, Pant R, Kurar A, Moreau P, Younge D. Modular mega prosthesis for proximal femoral tumors. Int Orthop. 2002;26(3):170–173. doi: 10.1007/s00264-002-0335-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawai A, Muschler GF, Lane JM, Otis JC, Healey JH. Prosthetic knee replacement after resection of a malignant tumor of the distal part of the femur. Medium to long-term results. J Bone Joint Surg (Am) 1998;80(5):636–647. doi: 10.2106/00004623-199805000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Lindner NJ, Ramm O, Hillmann A, Roedl R, Gosheger G, Brinkschmidt C, Juergens H, Winkelmann W. Limb salvage and outcome of osteosarcoma: The University of Muenster experience. Clin Orthop. 1999;358:83–89. doi: 10.1097/00003086-199901000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Malo M, Davis AM, Wunder J, Masri BA, Bell RS, Isler MH, Turcotte RE. Functional evaluation in distal femoral endoprosthetic replacement for bone sarcoma. Clin Orthop. 2001;389:173–180. doi: 10.1097/00003086-200108000-00024. [DOI] [PubMed] [Google Scholar]
- 14.McGoveran BM, Davis AM, Gross AE, Bell RS. Evaluation of the allograft-prosthesis composite technique for proximal femoral reconstruction after resection of a primary bone tumor. Can J Surg. 1999;42(1):37–45. [PMC free article] [PubMed] [Google Scholar]
- 15.Natarajan MV, Annamalai K, Williams S, Selvaraj R, Rajagopal TS. Limb salvage in distal tibial osteosarcoma using a custom mega prosthesis. Int Orthop. 2000;24(5):282–284. doi: 10.1007/s002640000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ritschl P, Capanna R, Helwig U, Campanacci M, Kotz R. KMFTR (Kotz Modular Femur Tibia Reconstruction System) modular tumor endoprosthesis system for the lower extremity. Z Orthop. 1992;130(4):290–293. doi: 10.1055/s-2008-1039620. [DOI] [PubMed] [Google Scholar]
- 17.Rompen JC, Ham JS, Halbertsma JP, Horn JR. Gait and function in patients with a femoral endoprosthesis after tumor resection: 18 patients evaluated 12 years after surgery. Acta Orthop Scand. 2002;73(4):439–446. doi: 10.1080/00016470216319. [DOI] [PubMed] [Google Scholar]
- 18.Rougraff BT, Simon MA, Kneisl JS, Greenberg DB, Mankin HJ. Limb salvage compared with amputation for osteosarcoma of the distal end of the femur. A long-term oncological, functional, and quality-of-life study. J Bone Joint Surg (Am) 1994;76(5):649–656. doi: 10.2106/00004623-199405000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Shin KH, Park HJ, Yoo JH, Hahn SB. Reconstructive surgery in primary malignant and aggressive benign bone tumor of the proximal Humerus. Yonsei Med J. 2000;41(3):304–311. doi: 10.3349/ymj.2000.41.3.304. [DOI] [PubMed] [Google Scholar]
- 20.Tunn PU, Schmidt-Peter P, Pomraenke D, Hohenberger P. Osteosarcoma in children - long-term functional analysis. Clin Orthop. 2004;421:212–217. doi: 10.1097/01.blo.0000126301.34087.b4. [DOI] [PubMed] [Google Scholar]
- 21.Wittig JC, Bickels J, Kellar-Graney KL, Kim FH, Malawer MM. Osteosarcoma of the proximal humerus: long-term results with limb-sparing surgery. Clin Orthop. 2002;397:156–176. doi: 10.1097/00003086-200204000-00021. [DOI] [PubMed] [Google Scholar]
- 22.Wood-Dauphinee S, Williams JI. Reintegration to Normal Living as a proxy to quality of life. J Chronic Dis. 1987;40(6):491–502. doi: 10.1016/0021-9681(87)90005-1. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organisation (1980) International classification of impairments, disabilities, and handicaps. Geneva
- 24.World Health Organisation (2002) Towards a common language for functioning, disability and health: The international classification of Functioning, Disability and Health (ICF) Geneva
- 25.Zahlten-Hinguranage A, Bernd L, Ewerbeck V, Sabo D. Equal quality of life after limb-sparing or ablative surgery for lower extremity sarcomas. Br J Cancer. 2004;91(6):1012–1014. doi: 10.1038/sj.bjc.6602104. [DOI] [PMC free article] [PubMed] [Google Scholar]