Abstract
From July 2004 to June 2005, 19 patients with 25 discs underwent anterior cervical discectomy and interbody fusion (ACDF) in which polyetheretherketone (PEEK) cages were filled with freeze-dried cancellous allograft bone. This kind of bone graft was made from femoral condyle that was harvested during total knee arthroplasty. Patient age at surgery was 52.9 (28–68) years. All patients were followed up at least 1 year. We measured the height of the disc and segmental sagittal angulation by pre-operative and post-operative radiographs. CT scan of the cervical spine at 1 year was used to evaluate fusion rates. Odom's criteria were used to assess the clinical outcome. All interbody disc spaces achieved successful union at 1-year follow-up. The use of a PEEK cage was found to increase the height of the disc immediately after surgery (5.0 mm pre-operatively, 7.3 mm immediately post-operatively). The final disc height was 6.2 mm, and the collapse of the disc height was 1.1 mm. The segmental lordosis also increased after surgery (2.0° pre-operatively, 6.6° immediately post-operatively), but the mean loss of lordosis correction was 3.3° at final follow-up. Seventy-four percent of patients (14/19) exhibited excellent/good clinical outcomes. Analysis of the results indicated the cancellous allograft bone-filled PEEK cage used in ACDF is a good choice for patients with cervical disc disease, and avoids the complications of harvesting iliac autograft.
Résumé
De juillet 2004 à juin 2005, 19 patients ont bénéficié de 25 discectomies cervicales suivies d’arthrodèses intercorporéales (ACDF) avec l’utilisation de cages de type PEEK utilisant des allogreffes cryoconservées. Le matériel osseux a été obtenu à partir de condyles fémoraux récupérés lors d’une prothèse totale du genou. Matériel et méthode : la moyenne d’âge lors de la chirurgie a été de 52.9 ans (28 à 68). Tous les patients ont été suivis au moins un an. Nous avons mesuré radiologiquement la hauteur du disque et les angulations sagittales pré et post-opératoires. Afin d’évaluer la bonne fusion nous avons utilisé un scanner cervical un an après l’intervention. Les critères d’Odomi ont été appréciés de façon à évaluer le résultat clinique. Les disques arthrodésés sont considérés comme consolidés après un an post-opératoire. L’utilisation de cages de type PEEK semble améliorer la conservation de la hauteur du disque immédiatement après l’intervention (5.0 mm pré op, 7.3 mm post-op). La hauteur finale du disque étant de 6.2 mm et le collapsus du disque de 1.1 mm. La lordose segmentaire augmente également après l’intervention chirurgicale (2° en pré op et 6.6° immédiatement en post-opératoire) la perte de lordose est de 3.3° au dernier suivi. 74% des patients (14/19) ont un excellent résultat clinique. L’analyse de ces résultats nous indique que l’utilisation d’allogreffes cryoconservées associées à une cage de type PEEK dans l’arthrodèse cervicale permet d’obtenir une bonne fusion en évitant les complications secondaires à la prise de greffes iliaque.
Introduction
Cervical spondylosis usually occurs in the disc, including disc herniation, osteophyte formation at endplates or uncovertebral joints. Anterior cervical discectomy with interbody fusion (ACDF) is the surgical procedure of choice for cervical discogenic diseases. Use of anterior iliac bone graft for anterior interbody fusion has been the gold standard for decades. Although highly successful fusion is achieved by autogenous iliac bone graft, various studies have documented iliac donor site complications [1, 5]. These complications include persistent donor site pain, infection, haematoma formation, iliac crest fracture, and meralgia parasthetica. To prevent these complications, cages have been studied and applied in humans as potential bone substitutes for autograft in interbody fusion. The criteria required for an ideal cage for cervical interbody fusion are the following: providing immediate stability, maintaining spinal alignment and foraminal height, achieving higher or at least equal fusion success rate, and obviating complications by using autograft. Titanium or carbon fibre cages were widely used for cervical interbody fusion, but subsidence, migration, and structure failure have occurred [11, 17]. Polyetheretherketone (PEEK) is a non-absorbable biopolymer that has been used in a variety of industries including medical devices. The PEEK cages are biocompatible, radiolucent, and have modulus of elasticity similar to the bone. There were a few sporadic reports in the literature that mentioned PEEK cages used in the cervical spine. Cancellous allograft has been successfully used in orthopaedic surgery for a long time. It is usually applied to fill bone defects caused by fracture, bone tumour, or in joint revision surgery. This study was the first clinical and radiographic report obtained in patients undergoing ACDF in which PEEK cages were filled with freeze-dried cancellous allograft bone.
Materials and methods
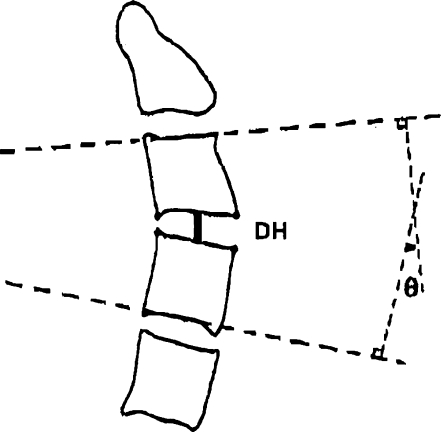
Between January 2005 and June 2005, 24 consecutive patients underwent ACDF using PEEK cages with allograft at our department. We prospectively followed these 24 patients, but only 19 patients were enrolled into this study because the other five patients received ACDF with anterior plating augmentation. This cohort compromised nine men and ten women with a mean age of 52.9 years. The clinical symptoms included cervical radiculopathy (13 patients) or myeloradiculopathy (6 patients) caused by nerve root or spinal cord compression. The surgery was performed when the patient had myelopathy or radiculopathy with progressive neurological deficit, or failure of conservative treatment (a minimum of 3 months). All the operations were done by the same doctor. A transverse skin incision was used. The anterior cervical disc was approached using the method described by Smith and Robinson [15]. A Caspar screw distractor was used to allow distraction of the disc space throughout the procedure. Cervical discectomy and removal of the posterior hypetrophic osteophytes were performed thereafter. The upper and lower endplates were prepared by removing the overlying cartilage and preserving the hardest subchondral bone. An optimal PEEK cage was selected following completion of discectomy and endplate preparation. The inner cavity of the PEEK cage was filled with cancellous allograft bone (Fig. 1). The PEEK cage with allograft was impacted into disc space for fusion after adequate distraction with the use of Caspar distractor. After surgery, all patients were protected by wearing a Miami brace for 3 months. Neck exercises were initiated 6 weeks after surgery and a normal activity level was progressively resumed. Plain AP and lateral cervical spine radiographs were taken before and after surgery and at 3, 6 and 12 months post-operatively. Radiographs with the neck in lateral flexion and extension were obtained at 12 months to evaluate fusion results. One independent orthopaedic surgeon assessed the status of interbody height, segmental sagittal alignment (Cobb’s angle), and final fusion results. The distance between the midpoint of the upper end plate and lower end plate was measured as interboby height. Cobb’s angle was measured using a protractor and defined as the angle between the cranial and caudal end plates of upper and lower vertebrae in the motion segment subjected to surgery (Fig. 2). We used radiographs obtained at 1-year follow-up to define union. Union of the cage was defined as no radiolucent line between the cage and endplate and no translation or angular change seen on lateral flexion and extension radiographs.
Fig. 1.
Photograph of a PEEK cage filled with cancellous allograft bone. This kind of allograft was harvested from femoral condyle during total knee arthroplasty
Fig. 2.
This diagram shows how disc height and segmental angle were determined. DH = disc height; theta = segmental angle
We used Odom criteria to evaluate clinical outcomes of the patients at 1-year follow-up [12]. By comparing the pre-operative and post-operative neurological status and subjective complaints, an independent observer who did not attend the surgery interviewed these patients and recorded the clinical results. Successful treatment was defined as the patient achieving improvement of symptoms, including excellent or good outcomes. Failed treatment was defined as persisting or worsened pre-operative symptoms. Duration of admission, operation time, and blood loss were also recorded.
Results
In this series, the mean operation time was 177.1 min (range, 67 to 251 min), estimated blood loss was below 50 ml in all 19 patients, and the mean hospital stay was 3.8 days (range, 2 to 7 days). All patients were followed up at least 1 year (range, 12 to 18 months). C5–6 was the major disc for surgery in this series. The demographic data of patients are shown in Table 1.
Table 1.
Demographic data of patients
| Characteristic | Total (n = 19) |
|---|---|
| Sex | |
| M | 9 |
| F | 10 |
| Age | 52.9 (28~68) |
| Radiculopathy | 13 |
| Myelopathy | 2 |
| Radiculomyelopathy | 4 |
| Level | |
| C3–4 | 1 |
| C4–5 | 5 |
| C5–6 | 11 |
| C6–7 | 8 |
| OP time (min) | 177.1 (67~251) |
| Hospital stay (day) | 3.8 (2~7) |
| Blood loss (c.c.) | <50 |
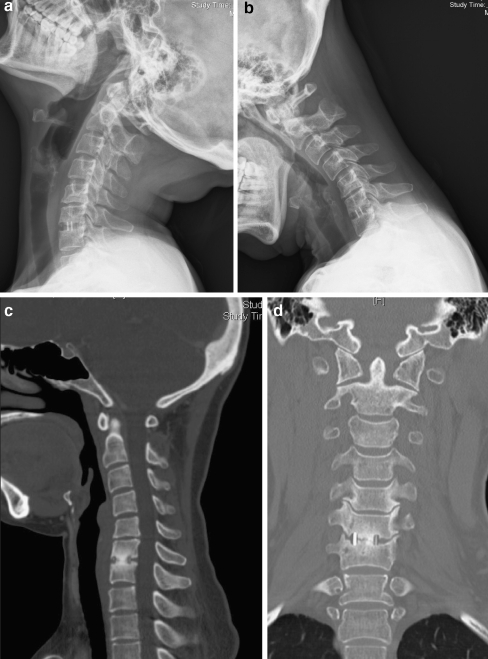
All 25 disc interspaces in 19 patients achieved solid union at final follow-up (Fig. 3). Clinical outcomes were rated as excellent or good in 14 patients (success rate: 74%). Two patients were graded as fair and three as poor clinical results. The mean pre-operative, immediately post-operative, and final interbody space heights were 5.0 mm (range, 2.6 to 7.0 mm), 7.3 mm (range, 5.0 to 8.7 mm), and 6.2 mm (range, 4.0 to 8.0 mm). The mean collapse of interbody space was 1.1 mm. The mean size of cages used in this series is 6.2 mm (5–7). Additionally, the mean segmental lordosis before surgery was 2.0° (range, −5.2° to 16.4°), corrected to 6.6° (range, −3.2° to 22.1°) immediately after surgery. The final mean segmental lordsis was 3.3° (range, −9.9° to 16.1°); the loss of correction was 3.3°. In these three patients with poor clinical results, the mean pre-operative interspace height was 4.8 mm. The mean immediately post-operative disc height was 6.4 mm, and the final disc height was 5.7 mm. The loss of disc height was 0.7 mm. The mean segmental lordosis was −1.6° before surgery, corrected to −0.9° immediately after surgery, and the final Cobbs angle was −4.4°. The mean loss of lordosis correction was 3.5°. The radiological data are shown in Table 2. There was no wound infection or further nervous tissue damage during the surgery.
Fig. 3.
Lateral flexion-extension cervical spine radiographs (a–b) and sagittal-coronal CT scans (c–d) obtained 12 months after C6–7 anterior cervical discectomy and fusion. Evidence of solid bridging bone on CT scans and no instability on flexion-extension radiographs were demonstrated
Table 2.
Radiographic data of surgery
| Parameter | Total (n = 19) | Success result (excellent + good) (n = 14) | Poor result (n = 3) |
|---|---|---|---|
| Disc height (mm) | |||
| Pre-operative | 5.0 | 4.9 | 4.8 |
| Post-operative | 7.3 | 7.5 | 6.4 |
| Final | 6.2 | 6.6 | 5.7 |
| Cage size (mm) | 6.2 | 6.5 | 5.8 |
| Segmental angle (lordosis degree) | |||
| Pre-operative | 2.0 | 1.3 | −1.6 |
| Post-operative | 6.6 | 7.0 | −0.9 |
| Final | 3.3 | 3.4 | −4.4 |
Discussion
The anterior cervical discectomy with interbody fusion is an effective method for treating patients with cervical disc diseases. Although tricortical autograft harvested from iliac crest as interbody fusion material can provide satisfactory clinical results and fusion rates, the complication rates of the donor site are around 20% [3]. Spinal surgeons have assessed numerous fusion materials in order to avoid harvesting iliac bone graft. Although frozen, irradiated allograft does not provide cells that form new bone, their organic matrix may have the ability to induce local bone formation. Banked fibula allograft was thought to be an excellent option, but the union rate is not as high as iliac autograft [19]. Cortical allograft was reported to have higher incidence of graft subsidence and graft collapse. Furthermore, the structure cortical allograft is seldom performed in our country because they mainly originate from voluntary donors and cannot be obtained commercially, thus limiting their availability.
There are numerous types of cages developed for ACDF including titanium, carbon fibre, and PEEK cages. Metallic cages used in ACDF can provide mechanical support, maintain initial disc height, and sagittal lordosis. Clinical results are satisfactory and donor site complications can be prevented [7, 13]. But cage subsidence or migration was also observed resulting in disc height collapse and kyphotic deformity [11]. In addition to a high fusion rate, successful treatment depends on maintenance of interspace height and segmental angle [9]. Furthermore, metallic cages are radio-opaque, which prevents the observation of trabecular bone formation, and radiographic determination of fusion has been debated.
The PEEK cage demonstrated absence of cytotoxicity and mutagenicity in an in vitro study [10]. With biocompatible, non-absorbable, and corrosion-resistant abilities, the PEEK cage is thought a safe biomaterial spacer for spine surgery [16]. The modulus of elasticity of PEEK is similar to bone [18]. This distinguishing feature is thought to be able to prevent cage subsidence induced by metallic cages. In an in vitro biomechanical study, the stiffness of the PEEK cage was statistically higher than that of the normal motion segment in flexion. Volume-related stiffness of the PEEK cage was higher than that of iliac bone in all directions. These results show that polyetheretherketone could be manufactured as the optimal interbody spacer containing adequate volume for bone refilling and providing immediate mechanical stability in ACDF [6]. In addition to the fact that the PEEK cage is radiolucent and does not produce artefacts on radiographs or CT scans, it is easy to evaluate fusion status on X-ray films.
To achieve successful fusion, the fusion material embedded in the cage is another key point. Boakye et al. reported results obtained in 24 patients with cervical disc disease who had undergone ACDF involving the placement of PEEK cages filled with recombinant human bone morphogenetic protein (rhBMP-2) and anterior plating [2]. A 100% fusion rate was achieved with evidence of solid bridging bone and no instability on dynamic X-ray films. But the cost of this bone substitute is high and not covered by the national health insurance in our country. Furthermore, adverse effects of rhBMP-2 used in anterior cervical spine fusion have been reported [14]. Cho et al. compared the results of 40 patients who underwent ACDF with PEEK spacers filled with autogenous iliac cancellous bone graft and a comparable group who underwent ACDF with autogenous tricortical iliac crest graft [4]. The fusion rate in the PEEK group was 100%, whereas that in the autogenous tricortical iliac crest graft group was 93%. The complication rate was lower in the PEEK cage group. Although clinical results were satisfactory, it was still necessary to create iliac wound even though the wound was small in the PEEK cage group.
Cancellous allograft bone had been used in posterior spine surgery and achieved good fusion results [8]. In our institute, femoral condyle harvested during total knee arthroplasty was processed as freeze-dried cancellous allograft. The fusion material filled in the PEEK spacer in the current study was this kind of allograft. In our series, all 19 patients with 25 discs achieved solid union after at least 1 year of follow-up. No cage subsidence or migration occurred and no complications associated with bone graft. The average disc height at the final follow-up was 6.2 mm, which was equal to the average size of cages used in this series (6.2 mm). The clinical outcomes were rated as excellent/good in 14 patients (74%). Three patients were rated as having poor results, though these three patients achieved solid union at the final follow-up. Analysis of radiographic data of these three patients showed that the immediate post-operation segmental lordosis was −0.9° and regressed to −4.4°. It was not possible to create the condition of local lordosis, which might have been due to the choice of the smaller size cage, resulting in poor clinical results.
Conclusions
The combination of PEEK cage and cancellous allograft bone for ACDF can lead to a high union rate and satisfactory clinical results without graft donor site complications. The sources of this kind of allograft are abundant. Solid fusion alone cannot promise successful clinical results. Creating and maintaining local cervical lordosis is necessary to achieve satisfactory results.
References
- 1.Arrington ED, Smith WJ, Chambers HG, Bucknell AL, Davino NA. Complications of iliac crest bone graft harvesting. Clin Orthop. 1996;329:300–309. doi: 10.1097/00003086-199608000-00037. [DOI] [PubMed] [Google Scholar]
- 2.Boakye M, Mummaneni PV, Garrett M, Rodts G, Haid R. Anterior cervical discectomy and fusion involving a polyetheretherketone spacer and bone morphogenetic protein. J Neurosurg Spine. 2005;2(5):521–525. doi: 10.3171/spi.2005.2.5.0521. [DOI] [PubMed] [Google Scholar]
- 3.Castro FP, Jr, Holt RT, Majd M, Whitecloud TS., 3rd A cost analysis of two anterior cervical fusion procedures. J Spinal Disord. 2000;13(6):511–514. doi: 10.1097/00002517-200012000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Cho DY, Liau WR, Lee WY, Liu JT, Chiu CL, Sheu PC. Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery. 2002;51(6):1343–1349. doi: 10.1097/00006123-200212000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Goulet JA, Senunas LE, DeSilva GL, Greenfield ML. Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop. 1997;339:76–81. doi: 10.1097/00003086-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Gu YT, Jia LS, Chen TY. Biomechanical study of a hat type cervical intervertebral fusion cage. Int Orthop. 2007;31(1):101–105. doi: 10.1007/s00264-006-0141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hwang SL, Hwang YF, Lieu AS, Lin CL, Kuo TH, Su YF, Howng SL, Lee KS. Outcome analyses of interbody titanium cage fusion used in the anterior discectomy for cervical degenerative disc disease. J Spinal Disord Tech. 2005;18(4):326–331. doi: 10.1097/01.bsd.0000164198.30725.2d. [DOI] [PubMed] [Google Scholar]
- 8.Jones KC, Andrish J, Kuivila T, Gurd A. Radiographic outcomes using freeze-dried cancellous allograft bone for posterior spinal fusion in pediatric idiopathic scoliosis. J Pediatr Orthop. 2002;22(3):285–289. doi: 10.1097/00004694-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Kao FC, Niu CC, Chen LH, Lai PL, Chen WJ. Maintenance of interbody space in one- and two-level anterior cervical interbody fusion: comparison of the effectiveness of autograft, allograft, and cage. Clin Orthop. 2005;430:108–116. doi: 10.1097/01.blo.0000142626.90278.9e. [DOI] [PubMed] [Google Scholar]
- 10.Katzer A, Marquardt H, Westendorf J, Wening JV, Foerster G. Polyetheretherketone-cytotoxicity and mutagenicity in vitro. Biomaterials. 2002;23(8):1749–1759. doi: 10.1016/S0142-9612(01)00300-3. [DOI] [PubMed] [Google Scholar]
- 11.Niu CC, Chen LH, Lai PL, Fu TS, Chen WJ. Trapezoidal titanium cage in anterior cervical interbody fusion: a clinical experience. Chang Gung Med J. 2005;28(4):212–221. [PubMed] [Google Scholar]
- 12.Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc. 1958;166(1):23–28. doi: 10.1001/jama.1958.02990010025006. [DOI] [PubMed] [Google Scholar]
- 13.Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A. Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine. 2006;4(6):447–453. doi: 10.3171/spi.2006.4.6.447. [DOI] [PubMed] [Google Scholar]
- 14.Shields LB, Raque GH, Glassman SD, Campbell M, Vitaz T, Harpring J, Shields CB. Adverse effects associated with high-dose recombinant human bone morphogenetic protein-2 use in anterior cervical spine fusion. Spine. 2006;31(5):542–547. doi: 10.1097/01.brs.0000201424.27509.72. [DOI] [PubMed] [Google Scholar]
- 15.Smith GW, Robinson RA. The treatment of certain cervical spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg [Am] 1958;40:607–624. [PubMed] [Google Scholar]
- 16.Toth JM, Wang M, Estes BT, Scifert JL, Seim HB, 3rd, Turner AS. Polyetheretherketone as a biomaterial for spinal applications. Biomaterials. 2006;27(3):324–334. doi: 10.1016/j.biomaterials.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 17.Haven I, Loon PJ, Bartels RH, Susante JL. Anterior cervical interbody fusion with radiolucent carbon fiber cages: clinical and radiological results. Acta Orthop Belg. 2005;71(5):604–609. [PubMed] [Google Scholar]
- 18.Wenz LM, Merritt K, Brown SA, Moet A, Steffee AD. In vitro biocompatibility of polyetheretherketone and polysulfone composites. J Biomed Mater Res. 1990;24(2):207–215. doi: 10.1002/jbm.820240207. [DOI] [PubMed] [Google Scholar]
- 19.Young WF, Rosenwasser RH. An early comparative analysis of the use of fibular allograft versus autologous iliac crest graft for interbody fusion after anterior cervical discectomy. Spine. 1993;18(9):1123–1124. doi: 10.1097/00007632-199307000-00002. [DOI] [PubMed] [Google Scholar]