Abstract
We have attempted to determine the spatial orientation of the base of the superior articular process in relation to the centre of the pedicle and then measure the transverse and sagittal screw angles using this ideal pedicle screw entry point – the base of the superior articular process at the junction of the lateral one-third and medial two-thirds. The proposed advantages of this technique are the easily identifiable entry point, the well-defined transverse and sagittal screw angles and a very low incidence of medial and inferior pedicle violation.
Résumé
Nous avons essayé de déterminer quelle devait être l’orientation pour l’implantation de vis pédiculaires au centre du pédicule en se basant par rapport aux articulaires. Le point d’entrée idéal se situe à la base de l’articulaire supérieure à la jonction du tiers moyen et du tiers latéral. Ce point est facile à identifier et parfaitement bien défini. Il réduit le nombre d’erreurs d’implantation en dehors du pédicule.
Introduction
The use of pedicle screws has become popular during the past decade, first in applications involving the lumbar spine and subsequently in thoracic spine surgery. Pedicle screws have various biomechanical advantages [2, 10, 12, 15, 17, 18], but screw malposition can be devastating when it occurs in the proximity of neurovascular [4] and visceral structures [6]. In addition, there is a long learning curve associated with pedicle screws [9]. To aid the surgeon, various insertion techniques, such as the free hand [8] and funnel technique [19] or the use of fluoroscopy [1, 5] to guide the pins into the pedicles [16] using computer-assisted systems [7], have been described. The margin for error for thoracic pedicle screws is very much lower than that for the lumbar counterparts and, hence, there are many studies describing the entry point and transverse and horizontal pedicle angles. Most of these studies, however, describe different entry points at different levels as well as different insertion techniques. In addition, the transverse process is involved, and the superior facet is used as a landmark. The situation changes in the case of a deformed spine as the transverse process may be abnormal in shape and size due to rotation and wedging. Conversely, the base of the superior facet is easy to identify and has a constant anatomical relationship to the pedicle. We therefore propose that the base of the superior articular process at the junction of the lateral one-third and medial two-thirds can be used as an ideal pedicle entry point. To evaluate this possibility, we have used a cadaveric model and attempted to determine the spatial orientation of this point with respect to the centre of the pedicle; we have also measured the transverse and sagittal screw angles using this entry point. The proposed advantages of this technique are an entry point which is easy to identify, well-defined transverse and sagittal screw angles and a very low incidence of medial and inferior pedicle violation.
Material and methods
The study was carried out using ten fresh cadavers (six male and four female). The mean age of spine donors was 50 years (range: 30–70 years). Prior to the experiment, radiological assessment was done on all cadavers to exclude spinal deformity of the specimens. Two fellowship-trained spinal surgeons dissected the spine. This two-part study was carried out bilaterally on 240 pedicles between the first and twelfth thoracic (T) vertebrae.
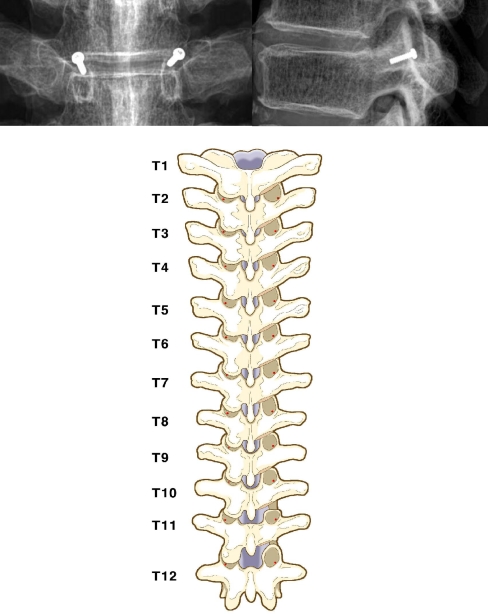
Part 1: study of the ideal pedicle entry point
A posterior midline incision was made and subperiosteal dissection carried out. Periarticular soft tissue was cleared to expose the facet joint and tips of the transverse process. With a 2-mm osteotome, approximately 5 mm of inferior articular process, which overhangs the base of the superior articular process, was removed so as to expose the base of the superior articular process situated to the right of the medial to lateral border. A vernier caliper with an accuracy of 0.1 mm was used to correctly identify the junction of the lateral one-third and medial two-thirds of the base of the superior articular process. The orientation of the transverse process was not considered throughout the procedure. However, at the end of the procedure the authors observed that this point was always slightly superior to the superior border of the transverse process. A 2-mm circular metal marker was placed over the proposed entry point (Fig. 1). In order that the X-ray beam be parallel to the end plates the radiographs were taken in three parts by centering the beam over the upper, middle and lower thoracic spine, respectively. The pedicle shadow can be easily identified by this method. The superior and lateral distance of the ideal pedicle entry point (IPEP) from the centre of the pedicle was then calculated using Rapidia ver. 2.7 software (INFINITT, Seoul, Korea). The accuracy of the software was 0.1 mm. Using the lateral radiograph, we attempted to find out the ideal sagittal angle for placement of the screw. The points considered were the centre of the metal marker and the junction of the upper one-third and lower two-thirds in the middle of the corresponding body. Two lines were then drawn, one along these two points and the other along the superior border of the body. The angle was then measured using the same software. The accuracy was 1°. To determine the horizontal angle a computed tomography (CT) scan was then performed with 2-mm-thick cuts. The points that were considered were the midpoint of this metal marker and the midpoint of the isthmus. One line was drawn along these points and the other line was drawn to bisect the vertebrae. The angles were measured using the same software with an accuracy of 1°. The whole procedure was carried out on one side by one spine surgeon and on the other side by the other surgeon. The two observations were blinded, and we were able to determine the interobserver reliability in identifying the IPEP.
Fig. 1.
Plain roentgenography shows the superolateral entry point in the anteroposterior view (left), and the superior location of the entry point in the lateral view (right). Posterior view (bottom) of the thoracic spine shows the pedicle screw entry points (red points) following the one-third and two-thirds rule
Part 2: study of pedicle screw violation
Using this IPEP, pedicle screws were inserted on the right side by one spine surgeon and on the other side by the other surgeon. An entry point was made using an awl. The thoracic gearshift (2-mm blunt-ended probe) was introduced. The angle at which the screws were inserted was indicated by the average pedicle angle in the horizontal and sagittal plane, which had been worked out as previously described. A goniometer was used to calculate the exact angle. The probe was then inserted into the body to a depth of around 30–40 mm for the lower thoracic spine and 20–25 mm for the proximal thoracic region. A sudden advancement of the pedicle finder usually indicates entrance into the soft tissues and, consequently, pedicle or body violation. A flexible ball-tipped pedicle sounding or palpating device was then inserted to palpate the floor and four walls. Special attention was paid to the first 10–25 mm of the hole. If a breach was discovered, then the pedicle finder was redirected. The pedicle was then undertapped with a tap that was 0.5 mm less in diameter. The pedicle tract was once again palpated to ensure that no wall had been breached. Pedicle screws (5 mm) were then inserted throughout the whole thoracic spine. We used 5-mm screws because we wanted our data of pedicle violation to be comparable to those of other series. The length of the screws was 35 mm in the lower thoracic spine, 30 mm in the middle and 25 mm in the upper thoracic spine. Radiographs (as previously described) and CT scans were done at the end of the procedure. The amount of medial or lateral cortical breach was classified as <2 mm, 2–4 mm or >4 mm.
Results
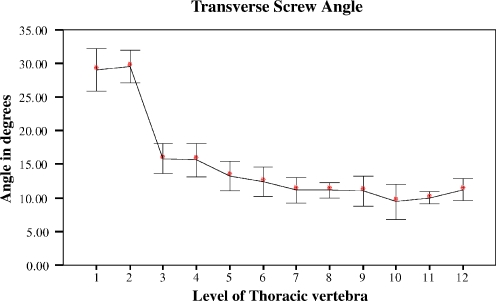
The superior distance of the IPEP from the centre of the pedicle showed a peculiar trend: it was 7.84 ± 0.94 mm at T1, decreasing rapidly to 5.62 ± 0.87 mm at T2, remaining fairly constant (4.68 mm–6.67 mm) between T2 and T9 and then increasing again to reach a maximum of 8.31 ± 0.94 mm at T10 before decreasing slightly to 7.18 ± 0.33 mm at T11 and 7.14 ± 0.24 mm at T12 (Fig. 2). The lateral distance of IPEP from the centre of the pedicle was at its maximum at T1 (5.41 ± 0.25 mm), decreasing to 3.66 ± 0.40 mm at T2 and to 1.72 ± 0.34 mm at T3, then remaining fairly constant up to T12 (range: 0.82 mm–1.81 mm) (Fig. 3). The maximum transverse screw angle was at T1 and T2 – 29 ± 1.87° and 29.50 ± 2.50°, declining first rapidly to 15.80 ± 2.25° at T3 then gradually to 9.40 ± 2.88° at T10 before increasing to11.20 ± 1.60° at T12 (Fig. 4). The maximum sagittal screw angle, 25.44 ± 0.62°, was at T1, declining rapidly to 21.20 ± 1.24° at T2, then remaining fairly constant at 19.93 ± 0.77° at T6 before declining again, first rapidly to 15.83 ± 2.83° at T7 and then more gradually to 5.19 ± 0.77° at T12 (Fig. 5). A medial violation of less than 2 mm occurred in four cases and lateral violation in ten (four less than 2 mm, four between 2 and 4 mm, two more than 4 mm). Superior wall violation occurred in four cases, but no inferior violation occurred (Table 1). Interobserver reliability was analysed using the statistical package SAS V 9.13 (SAS, Cary, N.C.). The results were expressed as a mean standard deviation. The reliability of locating the proposed ideal pedicle entry point was measured using the correlation coefficient, and the results revealed a high correlation at each level of the thoracic spine (Table 2).
Fig. 2.
Superior location of entry point from the centre of the pedicle according to level
Fig. 3.
Lateral location of the entry point from centre of the pedicle according to level
Fig. 4.
Transverse screw angle in relation to the centre of the pedicle according to level
Fig. 5.
Sagittal screw angle to the centre of the pedicle according to level
Table 1.
Incidence of pedicle violation
| Location | Number of screws | |
|---|---|---|
| Medial wall violation | <2 mm | 4(1.66%) |
| 2–4 mm | 0 | |
| >4 mm | 0 | |
| Lateral wall violation | <2 mm | 4(1.66%) |
| 2–4 mm | 4(1.66%) | |
| >4 mm | 2(0.83%) | |
| Superior wall violation | <2 mm | 4(1.66%) |
| 2–4 mm | 0 | |
| >4 mm | 0 | |
| Inferior wall violation | <2 mm | 0 |
| 2–4 mm | 0 | |
| >4 mm | 0 | |
Table 2.
Interobserver reliability
| Level (thoracic spine) | Superior | Lower |
|---|---|---|
| 1 | 0.91 | 0.91 |
| 2 | 0.92 | 0.81 |
| 3 | 0.94 | 0.85 |
| 4 | 0.85 | 0.84 |
| 5 | 0.80 | 0.19 |
| 6 | 0.84 | 0.86 |
| 7 | 0.83 | 0.91 |
| 8 | 0.90 | 0.89 |
| 9 | 0.90 | 0.85 |
| 10 | 0.94 | 0.87 |
| 11 | 0.89 | 0.85 |
| 12 | 0.95 | 0.95 |
Discussion
Although the application of pedicle screw instrumentation in the thoracic spine has been gaining acceptance and is a confirmed technique under certain conditions [17], thoracic pedicle screw fixation is a difficult procedure to master and can cause serious complications due to screw misplacement. Several techniques have been proposed to decrease the incidence of screw malposition and enhance safety. One of these, the free hand technique, relies on an accurate entry point, correct screw trajectories in the transverse and sagittal plane and palpation of all walls of the pedicles during each step of insertion. Rampersaud et al. [14] has shown that the maximal permissible translational error at the midthoracic and thoracolumbar junction is less than 1 mm and that the permissible rotation error is less than 5°. Morphometric studies have shown that the transverse diameter of the pedicle is less than 5 mm in some normal and scoliotic spines at the midthoracic level [13, 20]. It is therefore imperative that there be a constant entry point that is easy to identify and that the transverse and sagittal angles be calculated from this entry point. Our entry point is situated at the base of the superior facet at the junction of the lateral one-third and medial two-thirds. It is very easy to identify at all levels, as shown by the very high interobserver correlation. The superior distance of the IPEP from the centre of the pedicle was greater at the upper thoracic spine (T1) and lower thoracic spine T10–T12 and fairly constant between T2 and T9. This means that the point lies close to the centre of the pedicle in the middle thoracic spine and farther away towards the transition vertebrae. However, in terms of sagittal screw angles, these were at a maximum at the upper thoracic spine (T1 and T2) and showed a decreasing trend in the direction of T12. The reason for this is that the sagittal pedicle angle itself decreases as we proceed from T1 to T12, as shown in morphometric studies [20]. In terms of the lateral distance of IPEP, which is situated lateral throughout the thoracic vertebrae, the maximum distance was at T1 and T2 and the distance was fairly constant between T3 and T12. The transverse screw angle was at a maximum at T1 and T2, declining rapidly at T3 and then gradually until T10 before increasing again at T11 and T12. It is important to note that even at the lower thoracic level, the ideal direction of the screw is directed medially – even though the pedicle is neutral to slightly divergent as the entry point is situated lateral to the midpoint of the pedicle. A comparison of the transverse and sagittal screw angles with the transverse and sagittal pedicle angles that have been described in previous morphometric studies [20] reveals that the former are slightly larger, primarily because our entry point is situated superolateral to the midpoint of the pedicle. These angles should be used during the insertion of pedicle screws when using our entry point.
When pedicle violation using this technique is considered, 1.6% of the screws showed superior violation while no screws showed inferior violation; 1.6% screws showed a lateral or medial violation of <2 mm each, while 1.6% showed a lateral violation of 2–4 mm and 0.8% showed a lateral violation of >4 mm. There were no medial violations >2 mm. Most of the violations were at the midthoracic level. In a cadaveric study that used the junction of the superior border of the transverse process and lateral one-third of the base of the transverse process as the entry point, Cinnoti et al. [3] showed that the incidence of medial screw violation was 2% and that of the lateral cortex 10%. These researchers also mentioned that the bottom of the superior facet was located proximal to the centre of the pedicle at T4 but that it moved caudally from T4 to T12 where it was situated 2 mm below the centre of the pedicle. The reason for the difference between the two studies could be that Cinnoti et al. projected the pedicle onto the posterior surface of the lamina, while we have used radiographs to determine the centre of the pedicle. Vaccaro et al. [18] reported the entry point for T11 and T12 to be the junction of the middle of the transverse process and the middle of the superior facet, and that for T4–T9 to be the vertebrae junction of the superior border of transverse process and the middle of the superior facet. These researchers also reported that 41% of the pedicle screws were outside the boundaries of the pedicle. Cinnoti et al. [3] reported that choosing the entry point along the centre of the superior facet will increase the incidence of medial wall violation. Hence, a line along the midpoint of the superior facet should not be considered. The possible disadvantage of a superior entry point is that the screw has to be directed more caudally; as a result, it is not parallel to the end plate, thereby leading to a slightly lower pull-out strength. Nevertheless, the screw still has a much higher pull-out strength than hooks [11]. In addition, seating the rod to the screw will be difficult as they will be at an angle to each other. This can be overcome by using polyaxial screws in patients with normal anatomy and even in those with some spinal deformity having a greater flexibility. However, we expect this to occur only in the upper thoracic region where the angles were found to be greater.
We can therefore conclude that the ideal pedicle entry point described herein should be considered by surgeons during thoracic pedicle screw instrumentation. The base of the superior articular process at the junction of the lateral one-third and medial two-thirds will always remain constant and therefore act as a “polar star” in guiding the screw towards the entry of the pedicle.
Most surgeons should bear in mind that the results of our study may not be applicable to all patients worldwide in terms of ethnicity. Also, if the surgeon is not fully experienced in the method reported here, it will be necessary to combine it with another technique.
Contributor Information
Kook Jin Chung, Email: chungkjmd@dreamwiz.com.
Seung Woo Suh, Email: spine@korea.ac.kr.
References
- 1.Assaker R, Reyns N, Vinchon M, Demondion X, Louis E. Transpedicular screw placement: image-guided versus lateral-view fluoroscopy: in vitro simulation. Spine. 2001;26:2160–2164. doi: 10.1097/00007632-200110010-00024. [DOI] [PubMed] [Google Scholar]
- 2.Berlemann U, Cripton PA, Rincon L, et al. Pull-out strength of pedicle hooks with screw fixation screws: influence of screw length and angulation. Eur Spine J. 1996;5:71–73. doi: 10.1007/BF00307831. [DOI] [PubMed] [Google Scholar]
- 3.Cinotti G, Gumina S, Ripani M, Postacchini F. Pedicle instrumentation in the thoracic spine. A morphometric and cadaveric study for placement of screws. Spine. 1999;24:114–119. doi: 10.1097/00007632-199901150-00003. [DOI] [PubMed] [Google Scholar]
- 4.Ebraheim NA, Jabaly G, Xu R, et al. Anatomic relations of the thoracic pedicle to the adjacent neural structures. Spine. 1997;22:1160–1164. doi: 10.1097/00007632-199705150-00018. [DOI] [PubMed] [Google Scholar]
- 5.Hart RA, Hansen BL, Shea M, Hsu F, Anderson GJ. Pedicle screw placement in the thoracic spine: a comparison of image-guided and manual techniques in cadavers. Spine. 2005;30:E326–E331. doi: 10.1097/01.brs.0000166621.98354.1d. [DOI] [PubMed] [Google Scholar]
- 6.Heini P, Scholl E, Wyler D, et al. Fatal cardiac tamponade associated with posterior spinal instrumentation: a case report. Spine. 1998;23:2226–2230. doi: 10.1097/00007632-199810150-00017. [DOI] [PubMed] [Google Scholar]
- 7.Kim KD, Johnson JP, Bloch O, Masciopinto JE. Computer assisted thoracic pedicle screw placement. Spine. 2001;26:360–364. doi: 10.1097/00007632-200102150-00011. [DOI] [PubMed] [Google Scholar]
- 8.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: Is it safe? Spine. 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 9.Kim YJ, Lenke LG, Cheh G, Riew KD (2004) Defining the learning curve of free hand pedicle screw placement for adolescent idiopathic scoliosis surgery: sixty-seven consecutive cases. Poster presentation. Int Meet Adv Spine Technol, Bermuda
- 10.Krag MH, Weaver DL, Beynnon BD, Haugh LD. Morphometry of the thoracic and lumbar spine related to transpedicular screw placement for surgical spinal fixation. Spine. 1998;13:27–32. doi: 10.1097/00007632-198801000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Lehman RA, Jr, Kuklo TR. Use of the anatomic trajectory for thoracic pedicle screw salvage after failure/violation using the straight-forward technique: a biomechanical analysis. Spine. 2003;28:2072–2077. doi: 10.1097/01.BRS.0000084628.37133.BA. [DOI] [PubMed] [Google Scholar]
- 12.Liljenqvist U, Hackenberg L, Link T, Halm H. Pullout strength of pedicle screws versus pedicle and laminar hooks in the thoracic spine. Acta Orthop Belg. 2001;67:157–163. [PubMed] [Google Scholar]
- 13.Parent S, Labelle H, Skalli W, Guise J. Thoracic pedicle morphometry in vertebrae from scoliotic spines. Spine. 2004;29:239–248. doi: 10.1097/01.BRS.0000109995.64028.FE. [DOI] [PubMed] [Google Scholar]
- 14.Rampersaud YR, Simon DA, Foley KT. Accuracy requirements for image guided spinal pedicle screw placement. Spine. 2001;26:352–359. doi: 10.1097/00007632-200102150-00010. [DOI] [PubMed] [Google Scholar]
- 15.Skinner R, Maybee J, Transfeldt, et al. Experimental pullout testing and comparison of variables in transpedicular screw fixation: a biomechanical study. Spine. 1990;15:195–201. doi: 10.1097/00007632-199003000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine. 2001;26:2049–2057. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 17.Vaccaro AR, Rizzolo SJ, Balderstone R. Placement of pedicle screws in the thoracic spine. Part I: Morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77:1193–1199. doi: 10.2106/00004623-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Vaccaro AR, Rizzolo SJ, Balderston RA, et al. Placement of pedicle screws in the thoracic spine. Part II: An anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200–1206. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Yingsakmonkol W, Karaikovic E, Gains RW. The accuracy of pedicle screw placement in the thoracic spine using the funnel technique. J Spinal Disord. 2002;6:445–449. doi: 10.1097/00024720-200212000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Zindrick MR, Wiltse LL, Doornik A, Widell EH, Knight GW, Patwardhan AG, Thomas JC, Rothman SL, Fields BT. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine. 1987;12:160–166. doi: 10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]