Abstract
The aim of this study was to assess the outcome of primary cementless total hip arthroplasty in rheumatoid arthritis patients and to compare the results with osteoarthritis patients. Sixty-four patients (77 hips) with rheumatoid arthritis and 120 patients (135 hips) with osteoarthritis had a conical-shaped Zweymueller threaded cup and a tapered, rectangular Zweymueller stem implanted and were assessed after an average of 12.5 years. The endpoints for survival analysis were failure of one or both components due to radiographic loosening or revision. Revision was defined as exchange of cup, stem or both. When the PE-insert or the ceramic ball head were exchanged leaving cup and stem in place, e.g. for PE-wear or dislocation, this was not considered a revision but a re-intervention. No differences were found in survival rates; however, in the rheumatoid arthritis group there was an increased rate of malposition of the cup, avulsions of the greater trochanter, and increased bone resorption in the trochanteric region. This study shows that despite altered biomechanical properties of rheumatoid bone, mechanical stability and osseous integration of cementless prosthesis are not compromised and, although a higher complication rate did occur, long-term survival is excellent.
Résumé
Le but de cette étude est d’évaluer le devenir des prothèses totales sans ciment chez les patients porteurs d’arthrite rhumatoïde et, comparer ces résultats avec ceux des patients opérés pour coxarthrose. 64 patients (77 hanches) avec arthrite rhumatoïde et 120 patients (135 hanches) opérés pour coxarthrose ont bénéficié d’une prothèse de type Zweymueller avec une cup vissée. Le suivi moyen a été de 12.5 ans. La courbe de survie a été évaluée sur l’échec des deux composants avec descellement radiographique ou révision. La révision a été définie comme le changement de cup, de pièces fémorales ou des deux éléments. Lorsqu’il s’agit simplement d’un changement d’insert ou de têtes céramiques, les éléments principaux étant laissés en place (changement pour usure ou luxation) ceux-ci ne sont pas considérés comme une révision mais comme une réintervention. Il n’y a pas de différences, en terme de survie, des deux populations, cependant le groupe arthrite rhumatoïde a un taux de mal position de la cup plus important de même que les lésions du grand trochanter avec notamment une ostéolyse de cette région trochantérienne. Cette étude montre que malgré la mauvaise qualité de l’os rhumatoïde, il n’y a pas de problème d’instabilité ni d’ostéo intégration dans ce type de prothèse sans ciment et, l’on ne peut pas considérer que le taux de complications soit rédhibitoire, la survie à long terme étant excellente.
Introduction
The supposed increased long term survival of cementless total hip arthroplasty (THA) could be especially beneficial to the relatively young rheumatoid arthritis (RA) patient population.
However, RA is associated with altered biological and mechanical bone properties [1, 3, 4, 20, 21, 23]. This raises several potential complications when cementless prostheses are being used in RA patients. First of all, fractures of either the acetabulum or the femur could occur, both at the time of surgery and in the postoperative phase. Second, there could be an elevated risk of early aseptic loosening as a result of either a reduced primary stability of the implant, or of an altered metabolism of the bone, both potentially compromising the process of osseointegration.
Third, bone loss produced by stress-shielding around cementless stems may contribute to increased pain, periprosthetic fractures and eventually to loss of fixation [15]. This process of bone resorption is known to be more prominent when preoperative osteopenia is present as in RA patients [18, 19, 22].
To assess these potential complications a study was performed to analyse clinical and radiographic results of a group of RA patients after primary cementless THA and to compare these to the results of a group of OA patients.
Patients and methods
Between 1986 and 1992, 259 consecutive primary cementless THAs were carried out on 223 patients. Sixty-four patients (77 hips) were classified as having RA, and 120 patients (135 hips) were classified as having OA. Patients with other diagnoses were not included.
The implant
The Zweymueller cup is a conically shaped threaded cup made of grit blasted titanium (Zimmer, formerly Sulzermedica, Wintherthur, Switzerland). The insert is made of ultra-high molecular weight polyethylene. A 32 mm Biolox alumina ceramic ball head (Ceramtec, Plochingen, Germany) was used initially, and changed for a 28 mm Biolox alumina ceramic ball head (Ceramtec, Plochingen, Germany) from 1990 onwards. The Zweymuller stem is a tapered, rectangular shaped grit-blasted titanium alloy stem. A first generation cementless Zweymueller (Hochgezogen) stem was used from 1986 to 1987 followed by the second generation SL-Zweymueller (step-less) stem (Sulzermedica, Wintherthur, Switzerland) from 1988 onwards.
Surgical technique
Operations were performed with the patients lying supine using either an anterolateral or a straight lateral approach.
Follow-up evaluation
All patients were seen 3 and 6 months postoperatively and thereafter annually or biannually. Clinical results were assessed using the Harris Hip Score (HHS) [14]. Patients were asked to classify their pain level into one of three categories: no pain, mild to moderate pain, marked pain.
Radiographic analysis
Standard radiographs in two directions of the hip were obtained pre- and post-operatively. Assessment of radiolucencies at the acetabular side was performed according to DeLee and Charnley [7] and on the femoral side according to Gruen et al. [13]. Wear of the insert, bone resorption, cortical hypertrophy, and osteolytic lesions were assessed according to criteria described by Johnston et al. [16]. Inclination of the cup was determined by measuring the angle between the inter-teardrop line and a line through the opening plane of the cup. Malposition of the cup was defined as either perforation through the acetabular floor, a position more than 1 cm too cranial to the anatomical acetabulum, or an inclination of more than 55 degrees or less than 40 degrees. Malposition of the stem was defined as more than 2 degrees of varus or valgus alignment or a position more than 1 cm too cranial to the tip of the greater trochanter. Change in component position (migration, tilting, and subsidence) was determined by comparison between consecutive radiographs. Implant stability was defined according to the criteria described by Engh et al. [11].
Statistical analysis
The two diagnostic groups were compared either by using Fisher’s exact test or the chi-square test for 2 × 2 tables whenever the outcome was a dichotomous variable; the student t-test in case of continuous outcome variables; or a survival approach using Kaplan-Meier estimates and Cox proportional hazards models in the case of a dichotomous outcome as a function of “time since operation”. In all cases p values of <0.05 were considered statistically significant.
The probability of implant survival was estimated by Kaplan-Meier survival analysis in both diagnostic groups for the THA as a whole and for stem and cup separately. The survival analyses were each done twice; once for failure of the implant due to any cause, and once for failure due to aseptic loosening in which case a failure due to any other cause than aseptic loosening was treated as a censoring event in the Kaplan-Meier or Cox model.
Since aseptic loosening and non-aseptic loosening are actually “competing risks” and together define the event “overall failure”, the Kaplan-Meier estimates are themselves incorrect for the purpose of estimating the true probabilities in the population. Although the relative risks comparing the two diagnostic groups are estimated correctly for aseptic loosening and non-aseptic loosening respectively, the survival curves themselves should be calculated by a competing risk method, for which the package NCSS 2000 was used. In such a competing risk context, the sum of the survival curves for aseptic and non-aseptic loosening add up exactly to the overall survival curve (“due to any cause”). The relation between the diagnostic group and the risk of failure is estimated in the Cox framework. The test used to compare diagnostic groups is the log-rank test.
The endpoints for the survival analysis were failure due to radiographic loosening, revision of a component for any reason and revision of a component for aseptic loosening. Revision was defined as exchange of cup, stem or both components. When the PE-insert was exchanged for wear—leaving cup and stem in pace—this was considered as failure of the insert and not as failure of the cup. Also, when the ball-head was exchanged for recurrent dislocation, this was not considered as failure of the prosthesis. Therefore these procedures were not considered as revisions but as a re-interventions.
All data were stored in a database developed for data management of prosthetic surgery (Project Manager, version 7.0; Department of Medical Statistics, LUMC, Leiden, the Netherlands). This program was linked to SPSS version 10.1 (SPSS, Chicago, Illinois) for statistical analysis and to NCSS 2000 for the analysis of competing risks.
Results
The RA group was significantly younger than the OA group. The average age at operation in the RA group was 59.1 years (SD 11.5, range 27.1–78.4 years), and for the OA group the average was 65.9 years (SD 7.4, range 40.9–82.5 years). Gender distribution was the same in both groups (RA group: 22 male out of 77; OA group: 26 male out of 135). Sixty-three cases (29 RA, 34 OA) died before 10 years of follow-up was obtained. Two patients lived abroad (2 hips: 1 RA, 1 OA) and were eventually lost to follow-up at 51 and 95 months postoperative, respectively. Up to that time these patients had no complaints of hip pain. The mean follow-up time was 150 months (range 120–210 months).
The HHS improved significantly after surgery in both groups and this gain was maintained over the years; preoperative HHS, RA group: 28.7 (SD 15.6; range 15–74), OA group: 40.5 (SD 13.8, range 18–74).
Intraoperative complications
Acetabulum
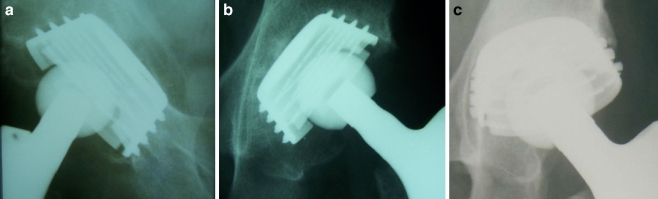
Perforation of the cup through the acetabular floor (Fig. 1a) and malposition of the cup more than 1 cm too cranial to the anatomical acetabulum (Fig. 1b) occurred more frequently in the RA group than in the OA group; 4 out of 77 versus 1 out of 135 (p < 0.05), and 5 out of 77 versus 0 out of 135 (p<0.05), respectively. None of these cups developed aseptic loosening.
Fig. 1.
a Protrusion of the cup through the acetabular floor perforating the internal lamina of the pelvis. b A too cranial position of the cup in relation to the anatomical acetabulum. c Tilting of the cup with radiolucent lines in all three zones 2 1/2 years after implantation
The incidence of malposition of more than 55 degrees or less than 40 degrees inclination was not different between the groups.
Femur
Avulsion of the tip of the greater trochanter occurred significantly more in the RA group than in the OA group; 10 out of 77 versus 4 out of 125 (p < 0.05). No relation was found to the survival of the implant or to other complications.
Incomplete shaft fractures were seen once in the RA group and twice in the OA group. These fractures were all secured by tension band wires and healed without complications.
Revisions
Acetabular component
In the RA group six cups needed revision, four due to aseptic loosening. Two of these occurred in an early phase, one of which was revised 31 months after the operation (Fig. 1c), while the other patient was also scheduled for revision but died due to co-morbidity from cardiovascular disease before the operation was carried out and is not mentioned in Table 1. For the survival analysis this case was classified as aseptic loosening. The two other cups developed signs of aseptic loosening in a later phase. They were combined with polyethylene (PE) wear and the development of osteolytic lesions and were revised after 117 and 123 months, respectively. Traumatic fracture of the acetabulum with tilting of the cup required revision in two RA patients, 102 and 112 months postoperatively. In the RA group, no cups were revised for infection or recurrent dislocations and none of the revised cups were in malposition.
Table 1.
Revisions
| Case | Gender, age in years | Year of surgery | Months to revision | Reason for revision | Revision surgery | |
|---|---|---|---|---|---|---|
| RA group | 165 | Female, 41 | 1989 | 31 | Early aseptic loosening | Cup |
| 22 | Female, 27 | 1989 | 117 | Loosening with osteolytic cysts and PE wear | Cup | |
| 144 | Male, 48 | 1987 | 123 | Loosening with osteolytic cysts and PE wear | Cup and stem | |
| 23 | Female, 27 | 1989 | 112 | Traumatic acetabular fracture | Cup | |
| 255 | Female, 53 | 1988 | 102 | Traumatic acetabular fracture | Cup | |
| OA group | 161 | Female, 67 | 1991 | 28 | Malposition | Cup |
| 222 | Female, 68 | 1987 | 5 | Malposition | Cup | |
| 2 | Male, 49 | 1989 | 40 | Early aseptic loosening | Cup | |
| 101 | Female, 67 | 1987 | 76 | Loosening with osteolytic cysts and PE wear | Cup and stem | |
| 100 | Female, 67 | 1987 | 123 | Loosening with osteolytic cysts and PE wear | Cup and stem | |
| 56 | Female, 72 | 1987 | 59 | Infection | Removal cup (and previously revised stem, see below) | |
| 121 | Male, 63 | 1990 | 71 | Infection | Cup | |
| 202 | Female, 68 | 1992 | 30 | Recurrent Dislocation | Cup | |
| 128 | Female, 58 | 1990 | 21 | Malposition | Stem | |
| 56 | Female, 72 | 1987 | 44 | Loosening with osteolytic cysts and PE wear | Stem and PE insert | |
| 187 | Male, 55 | 1987 | 74 | Loosening with osteolytic cysts and PE wear | Stem and PE insert |
RA rheumatoid arthritis, OA osteoarthritis, PE polyethylene
In the OA group eight cups were revised, three due to aseptic loosening; one cup with early loosening was revised after 40 months, two cups were revised in a later phase after, respectively, 76 and 123 months for aseptic loosening in combination with PE wear and the development of osteolytic lesions. None of these cups were malpositioned. Two other cups were revised for malposition; protrusio position of the cup induced instability due to lack of sufficient off-set in one hip. In another hip the anterior acetabular wall was damaged during reaming leaving the cup unstable. Two revisions were performed due to infection, and one for recurrent dislocation.
Femoral component
In the RA group one stem was revised together with the cup 123 months after the index operation due to severe PE wear in combination with extensive osteolytic lesions in the proximal femur and acetabulum.
In the OA group five stems were revised, four of which were for extensive osteolytic lesions in the proximal femur in combination with severe PE wear. One stem was revised due to malposition; the stem was placed too high and the patient complained of leg length discrepancy and thigh pain.
In all stem revisions the component was well anchored, necessitating a longitudinal osteotomy at the lateral side of the proximal femur in order to remove the stem.
Re-interventions
No re-interventions had to be carried out in the RA group. In the OA group nine re-interventions were carried out. In four hips recurrent dislocations developed. All four were treated successfully by implanting a longer ceramic ball head. In three hips the insert was exchanged because of PE wear. In two hips removal of heterotopic ossifications was carried out for complaints of pain and stiffness.
Radiographic results
Acetabulum
Incidence and distribution of radiolucent lines were not significantly different between the two groups. Bone atrophy was seen more often in the RA group than in the OA group; 8 out of 43 versus 2 out of 92 (p < 0.01) (Fig. 2). Osteolytic lesions were not found. All cups in both groups were classified as stable.
Fig. 2.

AP radiograph of the left hip of a 78-year-old female patient with rheumatoid arthritis 11 years after implantation of the Zweymueller prosthesis. Typical radiographic result with bone atrophy in the acetabulum in zones I and II, thin radiolucent lines around the stem in zones I and VII, and bone atrophy in the proximal femur in zones I and VII
Femur
Incidence of radiolucent lines around the proximal part of the stem in the RA group was slightly lower than in the OA group; 12 out of 47 versus 40 out of 95 (p = 0.05). Bone atrophy was found in the majority of the femora in both groups, predominantly in zones I and VII (Fig. 2). In the RA group there were significantly more femora with bone atrophy in three or more zones; 18 out of 47 versus 13 out of 95 (p < 0.01). Osteolytic lesions were seen around two stems in each group.
Survival analysis
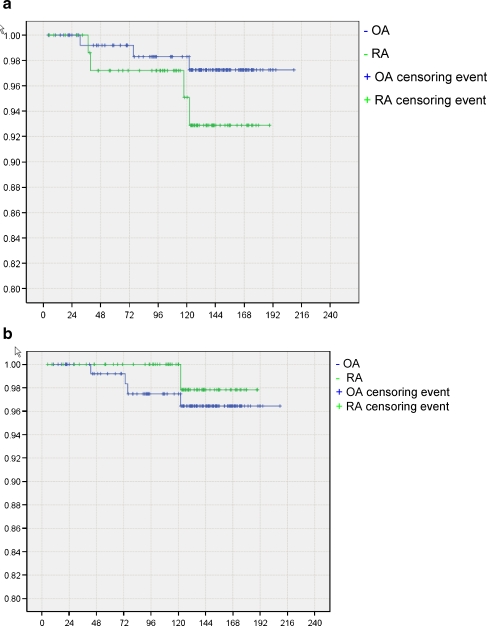
The failure rate for the acetabular component due to aseptic loosening after an average follow-up of 125 months (range 6–210) was 5.2% in the RA group and 2.2% in the OA group. The ten-year survival of the cup in the RA group with failure due to aseptic loosening as the endpoint was 0.95 [95% CI 0.90–1.0] while in the OA group it was 0.98 [95% confidence interval (CI) 0.96–1.00] (Fig. 3a).
Fig. 3.
Kaplan-Meier survival analysis of the cup (a) and stem (b) with failure due to aseptic loosening as endpoint. Failure due to any cause other than aseptic loosening was regarded as a censoring event. X-axis: months since operation. Y-axis: proportion of components unrevised. For confidence intervals at ten years see text
The failure rate due to aseptic loosening for the stem after an average follow-up of 125 months (6–210) was 1.3% in the RA group and 3.7% in the OA group. The ten year survival of the stem in the RA group with failure due to aseptic loosening as the endpoint was 1.0 while in the OA group it was 0.97 [95% CI 0.97–0.99] (Fig. 3b).
None of the survival analyses showed significant differences between the two groups.
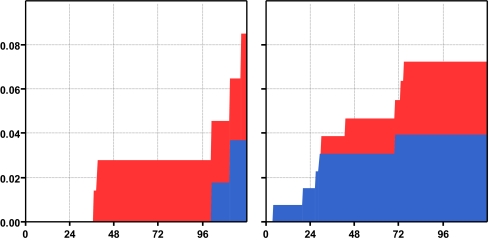
The cumulative probability of failure of one or both components split for aseptic loosening and other causes of component failure such as peri-prosthetic fracture, infection, malposition and recurrent dislocation are presented in Fig. 4.
Fig. 4.
Cumulative incidence of failure of one or both components of THA in a competing risk setting, by diagnostic group (left panel RA group; right panel OA group). X-axis: time in months since operation. Y-axis: probability of failure. Red area: probability of failure due to aseptic loosening (both early loosening and late loosening with osteolytic lesions and PE wear). Blue area: probability of failure due to other causes such as peri-prosthetic fracture, infection, malposition and recurrent dislocation
Discussion
Several studies show increased loosening of cemented THA in patients with RA [5, 17], but publications on cementless Zweymueller THA in RA patients are scarce. Publications on this prosthesis in OA patients report good results [6, 10, 12, 24, 25].
We found two studies on the Zweymueller cup in RA patients. Dominkus et al. [8] found 4% loosening rate in 82 THAs in 61 RA patients after 7 years (range 2–10) while Arnold et al. [2] report on a multi-centre study with several cementless designs after 6.9 years including 591 patients diagnosed with inflammatory joint disease. They concluded that all cementless prostheses could be used safely in RA patients.
On the Zweymueller stem in RA patients we found only one study. Effenberger et al. [9] reported only one stem revision for a traumatic femoral fracture in 60 THAs after 49 months (range 12–131).
In our material several complications occurred more frequently in the RA group: perforation of the cup through the acetabular floor and malposition of the cup in a too cranial position. Together with the two traumatic fractures of the acetabulum with tilting of the cup in the RA group and the increased rate of avulsions of the tip of the greater trochanter, these findings suggest a tendency for a higher rate of fractures in RA patients caused by the altered mechanical properties of the rheumatoid bone. Also, an increased rate of bone atrophy in the acetabulum and the proximal femur was found in the RA group compared to the OA group.
Thus far, this increased bone atrophy in the RA group did not lead to an increase in clinically related consequences, such as pain, aseptic loosening, and peri-prosthetic fractures in comparison with the OA group.
In summary, this study shows that the mechanical stability and the process of osseous integration on the cementless Zweymueller hip prosthesis does not seem to be compromised in RA patients as early aseptic loosening and long term survival were similar in the two diagnostic groups. However, the increased complication rates in RA patients (malposition of the cup, avulsions of the tip of the greater trochanter, and bone atrophy) confirm the concerns based on the altered biomechanical properties of the softer rheumatoid bone with this type of implant. In contrast to the very satisfactory results with the femoral component, accurate positioning of the threaded acetabular component appears to be a problem in RA patients.
References
- 1.Åkesson K, Önsten I, Obrant KJ. Periarticular bone in rheumatoid arthritis versus arthrosis. Acta Orthop Scand. 1994;65:135–138. doi: 10.3109/17453679408995420. [DOI] [PubMed] [Google Scholar]
- 2.Arnold P, Schüle B, Schroeder-Boersch H, Jani L. Überblick und Ergebnisse der ARO-Multicenterstudie. Orthopäde. 1998;27:324–332. doi: 10.1007/pl00003503. [DOI] [PubMed] [Google Scholar]
- 3.Bogoch E, Gschwend N, Bogoch B, Rahn B, Perren S. Juxtaarticular bone loss in experimental inflammatory arthritis. J Orthop Res. 1988;6:648–656. doi: 10.1002/jor.1100060505. [DOI] [PubMed] [Google Scholar]
- 4.Bogoch ER, Moran EL. Bone abnormalities in the surgical treatment of patients with rheumatoid arthritis. Clin Orthop. 1999;366:8–21. doi: 10.1097/00003086-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Creighton MG, Callaghan JJ, Olejniczak JP, Johnston RC. Total hip arthroplasty with cement in patients who have rheumatoid arthritis. J Bone Joint Surg (Am) 1998;80:1439–1446. doi: 10.2106/00004623-199810000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Delaunay C, Kapandji AI. Survival analysis of cementless grit-blasted titanium total hip arthroplasties. J Bone Jt Surg (Br) 2001;83:408–413. doi: 10.1302/0301-620X.83B3.11164. [DOI] [PubMed] [Google Scholar]
- 7.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop. 1976;121:20–32. [PubMed] [Google Scholar]
- 8.Dominkus M, Wanivenhaus AH, Morscher M, Powell G, Krismer M, Wölfl G. Different cup migration in rheumatoid arthritis and arthrosis. Acta Orthop Scand. 1998;69:455–462. doi: 10.3109/17453679808997778. [DOI] [PubMed] [Google Scholar]
- 9.Effenberger H, Ramsauer T, Böhm G, Hilzensauer G, Dorn U, Lintner F (2002) Successful hip arthroplasty using cementless titanium implants in rheumatoid arthritis. Arch Orthop Trauma Surg 122:80–87 [DOI] [PubMed]
- 10.Effenberger H, Ramsauer T, Dorn U, Imhof M. Factors influencing the revision rate of Zweymuller acetabular cup. Int Orthop. 2004;28(3):155–158. doi: 10.1007/s00264-004-0546-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Engh CA, Glassman AH, Suthers KE. The case for porous-coated hip implants. Clin Orthop. 1990;261:63–81. [PubMed] [Google Scholar]
- 12.Garcia-Cimbrelo E, Cruz-Pardos A, Madero R, Ortega-Andreu M. Total hip arthroplasty with use of the cementless Zweymüller Alloclassic system. J Bone Jt Surg (Am) 2003;85:296–303. doi: 10.2106/00004623-200302000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Gruen TA, McNeice GM, Astutz HC. Modes of failure of cemented stem-type femoral components. Clin Orthop. 1979;141:17–27. [PubMed] [Google Scholar]
- 14.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. J Bone Jt Surg (Am) 1969;5:737–755. [PubMed] [Google Scholar]
- 15.Huiskes R. The various stress patterns of press-fit, ingrown, and cemented femoral stems. Clin Orthop. 1990;261:27–38. [PubMed] [Google Scholar]
- 16.Johnston RC, Fitzgerald RH, Harris WH, Poss R, Müller ME, Sledge CB. Clinical and radiographic evaluation of total hip replacement. J Bone Jt Surg (Am) 1990;72:161–168. [PubMed] [Google Scholar]
- 17.Lugt JC, Onstenk R, Nelissen RG. Primary Stanmore total hip arthroplasty with increased cup loosening in rheumatoid patients. Int Orthop. 2003;27(5):291–293. doi: 10.1007/s00264-003-0473-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maloney WJ, Sychertz C, Bragdon C, McGovern T, Jasty M, Engh CA, Harris WH. Skeletal response to well fixed femoral components inserted with and without cement. Clin Orthop. 1996;333:15–26. [PubMed] [Google Scholar]
- 19.Nakamura K. Measurement of periprosthetic bone mineral density after cementless hip arthroplasty by dual energy X-ray absorptiometry. J Orthop Sci. 1996;1:113–122. doi: 10.1007/BF02348802. [DOI] [Google Scholar]
- 20.Oettmeier R, Babisch J. Osteologic standardization of human coxarthrosis using histomorphometry and its relevance for hip alloarthroplasty. Pathol Res Pract. 1992;188:620–624. doi: 10.1016/S0344-0338(11)80068-3. [DOI] [PubMed] [Google Scholar]
- 21.Önsten I, Åkesson K, Obrant KJ. Periarticular bone mineral content in rheumatoid arthritis and arthrosis of the hip. Acta Orthop Scand. 1993;64:530–532. doi: 10.3109/17453679308993685. [DOI] [PubMed] [Google Scholar]
- 22.Sychterz CJ, Engh CA. The influence of clinical factors on periprosthetic bone remodeling. Clin Orthop. 1996;322:285–292. [PubMed] [Google Scholar]
- 23.Trancik T, Mils W, Vinson N. The effect of indomethacin, aspirin, and ibuprofen on bone ingrowth into a porous-coated implant. Clin Orthop. 1989;249:113–121. [PubMed] [Google Scholar]
- 24.Vervest TM, Anderson PG, Hout F, Wapstra FH, Louwerse RT, Koetsier JW. Ten to twelve-year results with the Zweymüller cementless total hip prosthesis. J Arthroplasty. 2005;20:362–368. doi: 10.1016/j.arth.2004.11.017. [DOI] [PubMed] [Google Scholar]
- 25.Weissinger M, Helmreich C. Langfristige resultate mit dem zementfreien Alloclassic-Schaft nach Zweymüller. Z Orthop. 2001;139:200–205. doi: 10.1055/s-2001-16321. [DOI] [PubMed] [Google Scholar]