Abstract
Nowadays, the use of minimally invasive plate osteosynthesis (MIPO) in the management of fracture of the distal tibia is common. The various advantages of the MIPO technique, namely, preserving blood supply and better bone healing, have been described extensively in the literature. However, this technique is not without complication. Among all the complications, infection is one of the commonest. In the last 3 years, we have performed 48 cases of MIPO in treating distal tibia fractures. Our study was to evaluate the clinical outcome of these cases, with special attention to the infection rate and our experience in managing these infection cases. Our results showed that the average time until the patient started to bear full weight was 9.4 weeks. The average time for bony union was 18.7 weeks. There were 7 cases of late infection among these 48 cases. The rate was 15%. The presence of late infection had no obvious effect on the time to bony union. Twenty-five patients (52%) had the implants removed and the most common reason was skin impingement by the implant. The clinical presentation and management of these late infections are discussed. In conclusion, MIPO fixation of distal tibia fractures using a metaphyseal locking plate is safe and efficient. However, complications such as late wound infection and impingement are relatively common. The overall clinical outcome is still good despite the presence of these complications.
Résumé
L’utilisation d’une plaque par technique mini invasive (MIPO) dans le traitement des fractures distales du tibia est relativement fréquente. L’avantage de cette technique est de préserver la vascularisation et d’avoir une meilleure consolidation de l’os. Cependant cette technique n’est pas sans complications. Parmi ces complications l’infection est l’une des plus communes et des plus habituelles. Dans les trois dernières années, nous avons réalisé 48 cas de traitement de fractures distales du tibia selon la technique du MIPO. Notre étude nous a permis d’évaluer le devenir de tous ces cas avec une mention spéciale pour le taux d’infection. Le résultat montre que la moyenne de reprise d’appui a été de 9.4 semaines, le temps moyen de consolidation de 18.7 semaines. Il existe 7 cas d’infections tardives, soit un taux de 15%. La présence d’infection tardive n’a pas influé sur le temps de consolidation. 25 patients (52%) ont bénéficié d’une ablation des implants et la demande la plus fréquente d’ablation des implants est secondaire à une gêne au niveau sous-cutané. En conclusion, la fixation des fractures distales du tibia selon la technique MIPO, utilisant une plaque verrouillée est une technique sûre et efficace. Cependant, les complications d’infection tardive et d’une gêne sous cutané du fait du matériel sont relativement habituelles. Néanmoins, on peut considérer que le devenir clinique de ces patients reste bon malgré l’existence des complications.
Introduction
Distal tibia shaft fractures are commonly caused by bending and rotational forces. Open fractures are also commonly seen because of the relatively thin soft tissue coverage. This will in turn result in a higher rate of infection. In addition, this relatively short distal fragment makes rigid fixation technically difficult and complications are not uncommon. Therefore, distal tibia fracture is one of the most problematic fractures seen today.
In the past, open reduction and internal fixation using traditional metal plates for low energy trauma were quite successful [14]. However, if complications occur, prolonged hospital stay and increased number of subsequent operations are inevitable. Some will even lead to disastrous complications like gangrene and finally result in amputation [12]. The ring fixator once offered promising results but pin tract infection and later malunion are common in this group of patients [7].
Internal fixation with a tibial nail is another option for the distal tibia fracture if the fracture is not within 7 cm of the ankle joint [4]. The use of nail had a higher incidence of malunion [4, 17] and a second operation to promote union was quite common in the nail group. It has been reported that up to 19% of patients require additional procedures to promote union [9].
In recent years, the concept of biological osteosynthesis has gained a reputation in fracture treatment. Use of the minimally invasive plate osteosynthesis (MIPO) technique for the treatment of distal tibia fractures has been successfully employed by various groups [2, 5, 6, 8, 10, 13, 15, 16]. Moreover, the introduction of plate design like PC-fix (point contact fixation), LC-DCP (low contact dynamic compression plate) [2, 6] and LCP (locking compression plate) [15] minimises the trauma to the injured zone, preserves the circulation around the fracture site and also provides better fixation in the osteoporotic bone.
All these methods and their own merits and weaknesses with regards to different fracture situations have been well described in the literature [1, 17]. Infection rate is one of the most common surgical complications. Although the rate of infection with nail seemed to be a bit higher than plating, which is 4.6% compared to 2.4%, respectively, the result may not reflect the real situation because of the variability of the initial soft tissue trauma [17].
In the last 3 years, we have treated nearly 50 cases of distal tibia fractures using MIPO plating with the locking plate system. In this study, we would like to discuss the clinical outcome of these patients, with special attention to the rate of infection as well as its effect on the fracture healing. Is it true that the smaller wound has minimised the chance of wound complication? And furthermore, is it true that the use of metaphyseal locking plate is more comfortable than using the ordinary plate?
Materials and methods
This is a retrospective study of the clinical outcome using metaphyseal locking plate by the MIPO technique in fracture of the distal tibia. We reviewed 48 patients having acute distal tibia fractures from 1st March 2003 to 31st July 2006. The absolute indications for surgery were displaced fractures and unstable fractures. The relative indications include intolerance to conservative treatment, multiple fracture and patient’s preference. Paediatric fractures and pathological fractures, lower limbs with pre-existing neurological deficit, autoimmune disease or vascular disease were excluded from the study.
All these patients were treated using metaphyseal locking plate (Synthes, Bettlach) by the MIPO technique. They have had regular follow-up with X-rays in our out-patient clinic. The clinical outcome including movement, weight bearing status, X-ray appearance, and, most important of all, any complications were recorded.
Results
From March 2003 to August 2006, we performed 48 distal tibia fracture fixations using locking plate by the MIPO technique. There were 24 male and 24 female patients. The ages ranged from 21 to 87 years with an average of 51 years.
Fifteen patients were classified as high energy trauma. Nine of them were victims of road traffic accidents, four were victims who fell from height and the other two were hit by heavy metal. The other 33 patients sustained mainly twisting injuries on level ground or low energy direct trauma.
In these 48 fractures, five patients sustained multiple fractures. Nine patients (19%) had open fractures. Four of these patients were Gustilo type II or III. None required major soft tissue reconstruction or vascular repair. With regard to these four patients, two patients had an external fixator before definitive plating. The other two patients had MIPO fixation within 24 hours of injury. All open fractures were given second generation cephalosporin and aminoglycoside for 3 days for prophylaxis. The waiting time between the day of injury until definitive MIPO fixation varied from 0 to 17 days. The average was 4.4 days.
We classified the distal tibia fractures according to the Arbeitsgemeinschaft fur Osteosynthesefragen (AO) classification. In these 48 patients, 37 patients (77%) had their fractures around the distal tibia shaft. Nineteen patients (51%) had type A fractures, 13 patients (35%) had type B fractures and the remaining five (14%) were type C fractures. Eleven patients (23%) had fractures involving the metaphyseal area of the distal tibia: five were intra-articular and six were extra-articular fractures.
Bony union
All the study patients came back for follow-up for at least 6 months. The longest follow-up was 45 months with an average follow-up period of 18.7 months. The average time to radiological bony union was 18.7 weeks, which ranged from the shortest 12 weeks to the longest 44 weeks. Case 6 is excluded because bone graft was needed 12 weeks after first osteosynthesis to achieve bony union. We encountered five cases (10%) of delayed union (Table 1).
Table 1.
Cases of delay union
| Case | Age | M/F | Co-morbidities | Injury | Open/close | AO | Previous OT | Days to OT | Full wt bearing(wk) | Bony union (wk) | FU/mth | Remarks | Implant problem | Localised infection (time) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 6 | 46 | F | CA colon | RTA | OpenII | 42-C3 | Ext fix + debri. D0, D5, D9 | 2 | 12 after bone grafting | 52 wks after bone graft | 31 | Delayed union needing bone graft 3 months later | Impingement | No |
| 8 | 47 | M | RTA | Open IIIB | 42-B2 | nil | 1 | 28 | 44 | 27 | Debridement + skin graft D10; delay union | Broken screws | Yes (acute) | |
| 12 | 43 | F | S/F | Close | 42-C1 | nil | 1 | 8 | 28 | 23 | Impingement | No | ||
| 18 | 72 | F | DM, HT | S/F | Close | 42-A1 | nil | 1 | 8 | 28 | 18 | Nil | No | |
| 36 | 31 | F | GCT left knee curretage and cement 7/03 | S/F | Close; # cement bone | 42-A1 | nil | 16 | 8 | 44 | 11 | Delay union but no loosening of implant | Impingement | No |
GCT giant cell tumour, RTA road traffic accident, S/F slipped and fell
Three of these cases did not have infections. Only one patient (case 8) had acute infection after fixation which was treated by debridement and later split thickness skin grafting. He also had two broken screws in the distal fragment but the patient was not symptomatic and thus refused further surgery. The average time to bony union in the non-infected group was 18.4 weeks while the average time of the infected group was 19.4 weeks. The time to full weight bearing walking ranged from 5 to 28 weeks. The average was 9.2 weeks after operation excluding case 6.
Infection
As seen in Table 2, there were eight cases (17%) of post-operative infection, one patient had acute infection and seven were late infections. Patient 8 had acute infection. He had an open III B fracture left tibia. The infection was managed by debridement and antibiotics. He had split thickness skin grafting on day 10 and the infection settled. There were seven cases presented with late infection. All of them were superficial infection in the medial shin area. Six were closed injury. Only one had type I open injury. The onset of infection ranged from 2 to 12 months. Four of them presented as cellulitis (Fig. 1). They were treated by a course of antibiotics for 1 week. The other three late infection cases presented as subcutaneous abscess or discharging sinus. They needed incision and drainage with removal of implant after fracture healing. All delayed infections subsequently progressed to uneventful bony union. The rehabilitation was not greatly affected by late infection.
Table 2.
Cases of infection
| Case | Age | M/F | Co-morbidities | Injury | Open/close | AO | Days to OT | Full weight bearing(wk) | Bony union (wk) | FU/ mth | Implant problem | Onset of infection/ mth | Organism | Remarks | R/O(mth) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4 | 55 | F | S/F | Close | 42A1 | 7 | 8 | 20 | 36 | Nil | 6 | No culture | Treated with oral antibiotics | 14 | |
| 8 | 47 | M | RTA (Crush) | Open IIIB | 42-B2 | 1 | 28 | 44 | 27 | Broken screws | Acute | Aeromonas hydrophila | Acute wound infection, Debridement + skin graft on D10 | No | |
| 10 | 30 | M | Chronic drinker | Fell from height | Close | 43-C2 | 11 | 8 | 12 | 24 | Nil | 6 | MSSA | Infected implant with subcutaneous abscess, treated with incision and drainage | 6 |
| 13 | 43 | M | RTA (high energy) | Close | 42-B1 | 3 | 8 | 20 | 22 | Nil | 12 | No culture | Treated with oral antibiotics | 14 | |
| 20 | 51 | M | HT, old TB, varicosities | S/F | Close | 42-B1 | 3 | 8 | 16 | 18 | Nil | 2 | MSSA | Delay subcutaneous abscess treated with incision and drainage. | 16 |
| 44 | 87 | F | Right DHS 98; Left AMA 06 | S/F | Close | 42-A2 | 5 | 12 | 16 | 6 | Impingement | 4 | MRSA | Delay deep wound infection requiring immediate removal | 4 |
| 47 | 43 | M | RTA (high energy) | Open I | 42-B2 | 0 | 8 | 15 | 6 | Nil | 2 | No culture | Treated with oral antibiotics | No |
DHS dynamic hip screw, AMA Austin Moore arthroplasty, RTA road traffic accident, S/F slipped and fell, MSSA methicillin sensitive Staphylococcus aureus, MRSA methicillin resistant Staphylococcus aureus, R/O removal
Fig. 1.
Presentation as cellulitis
Implant removal
Twenty-five patients (52%) complained of implant impingement or discomfort around the medial tibial shin region. Twenty-three patients (48%) had their implants removed. Fourteen patients’ (61%) implant removal was for impingement while six patients had the implant removed for infection. Otherwise, another three patients’ plates were removed for personal reasons. The time of removal ranged from 4 to 34 months post-op. Two patients had breakage of locking screws in the distal fragment but all progressed to bony union.
Discussion
Over the past ten years, the concept of bridging plate osteosynthesis has been developed for multifragmentary shaft fractures. The technique minimises the soft tissue trauma to the injured zone which theoretically preserves a better blood supply around the fracture area [3]. Since the damage to the soft tissues and the blood supply is less extensive, more rapid fracture healing can be achieved.
In our series, the use of metaphyseal locking plate was an attempt to minimise the discomfort associated with the bulky implants such as the conventional DCP [8, 13, 16] or the LC-DCP [2, 6, 10]. Although there was no direct comment on the comfort of a bulky plate over the medial tibial cortex in these papers, the use of a low profile metaphyseal LCP around the medial tibial region will definitely provide better cosmesis and theoretically less chance of impingement. However, we still had 25 patients (52%) experiencing implant impingement. They usually complained of discomfort over the proximal end. However, the symptoms were mild and only 14 of them had the implants removed. The other nine patients who had their implants removed were for other reasons.
The relatively smaller distal fragment often poses a problem of adequate fixation during operation. The use of the ordinary DCP and the LC-DCP limits the number of screws in the distal fragment. The use of metaphyseal LCP provides a better fixation for the distal fragment. This is because of the special configuration of the 3.5 mm locking screw holes in the distal end of the plate (Fig. 2). Moreover, the bending of the plate with the locking screw system can generate multi-directional locking screws inside the cancellous metaphyseal region, thus providing a much better pull-out strength and better angular stability around the small distal fragment in comparison to the classical fixation technique.
Fig. 2.
Special configuration of locking screw holes
In our studies, the average time to union was 18.7 weeks. This is comparable with other reports of percutaneous tibia plating [2, 6, 11]. Five patients had delayed union. Case 6 had an open Type II tibial fracture with ipsilateral lower limb multiple fractures. Multiple debridements were performed. Case 8 was also an open Type IIIB fracture with debridement performed. Moreover, he developed acute wound infection which required debridement as well. Case 18 was an elderly lady with DM and HT. Although she had no open wound, her fracture was a simple AO A1 fracture but the reduction was less than satisfactory. Therefore, according to strain theory, this kind of simple fracture could not heal satisfactorily in this situation. Case 36 had a concurrent giant cell tumour in the distal femur. It had been treated by curettage and cementation. However, during the injury, there was also a fracture through the thin cortical bone in the cemented area. Therefore, together with the tibial fixation, a modular total knee replacement was also performed. It was postulated that a weaker and painful limb would make the whole rehabilitation process slower. We could not identify any obvious cause for poor bone healing in case 12.
Infection is one of the complications that we would like to discuss in detail. In our study, we had one acute infection (2%) and seven late infections (14.5%). Our definition of late infection is that infection happens after at least 1 month of complete wound healing without any sign of infection. In the literature, the rate of infection of plating ranges from 0%–6% [2, 5, 6, 8, 10, 11, 13, 16, 17]. The range varies because the degree of soft tissue injury is different in these studies, some include open fractures requiring soft tissue reconstruction [6] and some include only closed injuries [8, 10, 11, 13]. The rate of infection, especially late infection, seemed to be exceptionally high in our series. When we analysed these cases, all of them presented with complete healing of the wound before infection developed. Four of them (cases 4, 13, 38 and 47) presented with cellulitis and the other three (cases 10, 27 and 44) presented with small subcutaneous abscess formation and persistent drainage. The cellulitis was successfully treated with a course of antibiotics. The abscess needed drainage and a full course of antibiotics. Only one patient (case 44) had persistent infection despite antibiotics and daily dressing (Fig. 3). She was an 87-year-old woman with multiple osteoporotic fractures which were fixed and became only an exercise walker before she had the tibia fracture. The medial shin area was thin and the skin condition was sub-optimal. Since her X-ray showed bony union when the infection occurred, the implant was removed 4 months after the operation. She was given a protective brace for 1 month. The infection subsided after removal of the implant with a course of antibiotics.
Fig. 3.
Persistent infection in case 44
Regarding the organisms, all infected cases except one (case 44) were community acquired infection. Case 8 had Aeromonas hydrophila cultured from the wound. This organism usually comes from fresh water and can cause gastroenteritis. Cases 10 and 20 had methicillin sensitive Staphylococcus aureus (MSSA) infection. There was no positive bacteriological culture from the cellulitis cases. They were simply treated by a course of penicillin group antibiotics, usually ampicillin and cloxacillin in our cases. Case 44 was the elderly lady with severe infection 4 months after the surgery. The swab culture showed methicillin resistant Staphylococcus aureus (MRSA) infection. This was the only case in which removal of the implant was needed to control the infection. Since she was living in an institution after discharge from the hospital, the MRSA infection may be acquired from the institution after minor trauma.
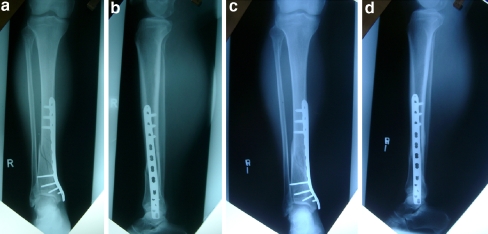
Although the rate of superficial infection seemed to be relatively high in our series, it seemed that bone healing was not affected by the presence of infection. The time to bony union in the normal and infected groups was 18.4 and 19.4 weeks, respectively. It seemed that the presence of low grade infection would have a minor adverse effect, if any, on bone healing. Moreover, the infection seemed to be well under control and there was no case of deep chronic infection causing osteomyelitis. The resistance of severe infection and good bony union rate may be due to the preservation of bony vascularity with the use of the MIPO technique (Fig. 4).
Fig. 4.
a,b X-ray of case 10 immediate post-op. He developed subcutaneous abscess 2 months post-op. c,d Bone progressed to uneventful healing after 6 months
In view of these infections, we could group these cases into two main groups. One is the cellulitis group and the other is the abscess formation group. For the cellulitis group, we suggest treating these cases with 1 week of penicillin group antibiotics. In our centre, we use ampicillin and cloxacillin orally. In our experience, all patients respond well. However, for the abscess formation group, a more aggressive treatment may be needed. We suggest that once abscess is formed, surgical incision and drainage are needed together with intravenous antibiotics for the acute phase. The wound is then managed by daily dressing until it granulates. Removal of the implant in both groups in an acute situation is rarely required. The decision is based on the clinical response of the initial management and the stage of bone healing. Since the bone healing is not affected much by the presence of late infection, most of the fractures are stable enough for removal of the implant without further protection at around 18 weeks.
Conclusion
The use of metaphyseal locking plate by minimally invasive percutaneous osteosynthesis is a safe and effective technique for the distal tibia fractures. This technique can help patients to resume their function early. The observed incidence of implant impingement and minor wound complications was quite common but these could be simply resolved by implant removal with antibiotics. The overall rehabilitation and function of the patient was not affected at all. Nevertheless, this technique has revolutionised treatment of distal tibial fractures even in difficult osteoporotic bone.
References
- 1.Bedi A, Le TT, Karunakar MA. Surgical treatment of nonarticular distal tibia fractures. J Am Acad Orthop Surg. 2006;14(7):406–416. doi: 10.5435/00124635-200607000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Borg T, Larsson S, Lindsjo U. Percutaneous plating of distal tibial fractures. Preliminary results in 21 patients. Injury. 2004;35(6):608–614. doi: 10.1016/j.injury.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Borrelli J, Jr, Prickett W, Song E, Becker D, Ricci W. Extraosseous blood supply of the tibia and the effects of different plating techniques: a human cadaveric study. J Orthop Trauma. 2002;16(10):691–695. doi: 10.1097/00005131-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Hahn D, Bradbury N, Hartley R, Radford PJ. Intramedullary nail breakage in distal fractures of the tibia. Injury. 1996;27(5):323–327. doi: 10.1016/0020-1383(95)00228-6. [DOI] [PubMed] [Google Scholar]
- 5.Helfet DL, Shonnard PY, Levine D, Borrelli J., Jr Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997;28(Suppl 1):A42–A48. doi: 10.1016/S0020-1383(97)90114-5. [DOI] [PubMed] [Google Scholar]
- 6.Krackhardt T, Dilger J, Flesch I, Hontzsch D, Eingartner C, Weise K. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg. 2005;125(2):87–94. doi: 10.1007/s00402-004-0778-y. [DOI] [PubMed] [Google Scholar]
- 7.Leung F, Kwok HY, Pun TS, Chow SP. Limited open reduction and Ilizarov external fixation in the treatment of distal tibial fractures. Injury. 2004;35(3):278–283. doi: 10.1016/S0020-1383(03)00172-4. [DOI] [PubMed] [Google Scholar]
- 8.Maffulli N, Toms AD, McMurtie A, Oliva F. Percutaneous plating of distal tibial fractures. Int Orthop. 2004;28(3):159–162. doi: 10.1007/s00264-004-0541-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nork SE, Schwartz AK, Agel J, Holt SK, Schrick JL, Winquist RA. Intramedullary nailing of distal metaphyseal tibial fractures. J Bone Joint Surg Am. 2005;87(6):1213–1221. doi: 10.2106/JBJS.C.01135. [DOI] [PubMed] [Google Scholar]
- 10.Oh CW, Kyung HS, Park IH, Kim PT, Ihn JC. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res. 2003;408:286–291. doi: 10.1097/00003086-200303000-00038. [DOI] [PubMed] [Google Scholar]
- 11.Pai V, Coulter G, Pai V (2006) Minimally invasive plate fixation of the tibia. Int Ortho [Epub 8 September 2006] [DOI] [PMC free article] [PubMed]
- 12.Pugh KJ, Wolinsky PR, McAndrew MP, Johnson KD. Tibial pilon fractures: a comparison of treatment methods. J Trauma. 1999;47(5):937–941. doi: 10.1097/00005373-199911000-00022. [DOI] [PubMed] [Google Scholar]
- 13.Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury. 2004;35(6):615–620. doi: 10.1016/j.injury.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 14.Ruedi TP, Allgower M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res. 1979;138:105–110. [PubMed] [Google Scholar]
- 15.Ryf C, Gotsch U, Perren T, Rillmann P. New surgical treatment procedures in fractures of the distal tibia (LCP, MIPO) Ther Umsch. 2003;60(12):768–775. doi: 10.1024/0040-5930.60.12.768. [DOI] [PubMed] [Google Scholar]
- 16.Toms AD, McMurtie A, Maffulli N. Percutaneous plating of the distal tibia. J Foot Ankle Surg. 2004;43(3):199–203. doi: 10.1053/j.jfas.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 17.Zelle BA, Bhandari M, Espiritu M, Koval KJ, Zlowodzki M. Evidence-based orthopaedic trauma working group. Treatment of distal tibia fractures without articular involvement: a systematic review of 1125 fractures. J Orthop Trauma. 2006;20(1):76–79. doi: 10.1097/01.bot.0000202997.45274.a1. [DOI] [PubMed] [Google Scholar]