Hilar cholangiocarcinomas involving either the right and/or left hepatic duct (Bismuth-Corlette type IIIa/IIIb or IV) are generally proposed to require resection of the respective hemiliver or extended hemiliver to achieve clear margins.1,2 When the hepatic artery is occupied by the tumour,3 hemihepatectomy concurrent with resection of the common hepatic artery or the artery bifurcations can achieve the largest benefit with respect to resectability and oncologic radicality. Nonetheless, the functional failure of the hepatic remnant, bile leakage, liver necrosis and abscess restrict its application. In our study, we report that 2 patients with hilar cholangiocarcinoma accompanied by hepatic artery infiltration underwent left hemihepatectomy, hepatic artery resection and biliary reconstruction and that both recovered smoothly.
Case 1
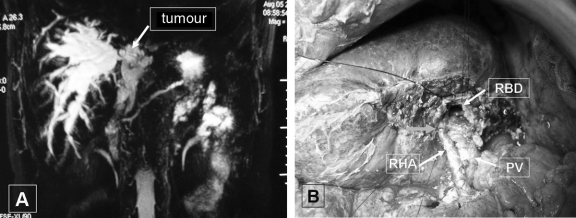
A 65-year-old man was admitted to our hospital on August 4, 2004, because of yellow skin and sclera existing for 10 days. Laboratory results were as follows: total bilirubin (TB) 359 μmol/L, direct bilirubin (DB) 271 μmol/L, alanine transferase (ALT) 164 U/L, aspartate aminotransferase (AST) 84 U/L, alkaline phosphatase (ALP) 523 U/L and carbohydrate antigen 19-9 (CA19-9) 695.2 U/L. Ultrasonography showed a solid echo pattern (D = 1.8 cm) in the hilum, and magnetic resonance cholangiopancreatography (MRCP) indicated changiocarcinoma (Bismuth-Corlette type IIIb) (Fig. 1A). Intraoperative exploration revealed the tumour located in the hilum involving the left liver, while the bilateral bile duct was totally obstructed. Invasion of the right hepatic artery was found during the left hemihepatectomy and extrahepatic biliary tract resection. The the invaded hepatic artery was resected, and end-to-end artery anastomosis was performed (Fig. 1B) after the right triangular and coronary ligaments were disconnected to diminish the tension at both ends of the arteries. Doppler ultrasound indicated that hepatic artery patency was not achieved after reconstruction of the artery. Pathological examination demonstrated papillary adenocarcinoma with negative margins. Postoperatively, aminotransferase levels were found to be moderately elevated (ALT/AST: 281/ 300 U/L), but they quickly reverted to normal within 7 days. However, the patient developed liver necrosis and abscess 3 months later, recovering after a course of sensitive antibiotics.
FIG. 1. MRCP image (A) and intraoperative picture (B) of Case 1. MRCP showed the hilar tumour (arrow) that extended to the atrophied left liver and the dilated right bile duct. MRCP = magnetic resonance cholangiopancreatography; PV = portal vein; RBD = right bile duct; RHA = right hepatic artery.
Case 2
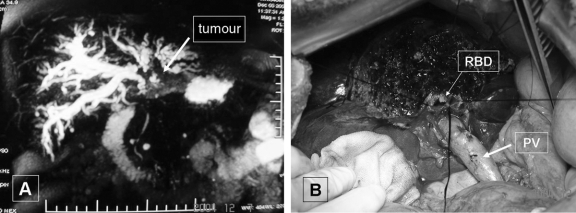
A 38-year-old man was hospitalized to our department with yellow skin that had persisted for 10 days. The levels of TB/DB (308/277 μmol/L), ALT (180 U/L) and γ-glutamyltransferase (γ-GT; 236 U/L) suggested obstructive jaundice. CA19-9 was elevated significantly (1226 U/L). Computed tomography and MRCP showed a hilar obstruction compressing intrahepatic bile duct dilatation, as well as left liver atrophy (Fig. 2A). The patient was diagnosed with hilar cholangiocarcinoma (Bismuth-Corlette type IIIb) and underwent surgery 3 days after admission. Laparotomy revealed that the tumour was located in the bifurcation of the bile duct and extended to the atrophic left liver, with invasion of the hepatic artery. We carried out left liver and partial segment V resection, lymphadenectomy and dearterialization of the remnant liver by resection of the invaded artery. We subsequently performed proximal bilioenteric anastomosis, using a jejunum Y-loop and the posterior and anterior bile duct (Fig. 2B). Pathology reported papillary adenocarcinoma with nerve invasion and lymph nodes metastasis. Postoperatively, the patient had elevated ALT and AST (1362 U/L, 650 U/L) that declined to normal after 10 days.
FIG. 2. Magnetic resonance cholangiopancreatography image (A) and intraoperative picture (B) of Case 2. The tumour was located in the hilus and involved the left liver. PV = portal vein; RBD = right bile duct.
Discussion
According to recent literature reviews, the overall inhospital mortality rates for hilar cholangiocarcinoma decreased from 20% in 1988–1993 to 10.3% in 1998–2003, with liver failure still the most common postoperative cause of death.1 We doubted whether hemihepatectomy with hepatic artery resection would result in liver failure, and we therefore proposed such a surgical strategy, albeit with limited experience. Miyazaki and colleagues4 reported that a patient who received left hemihepatectomy and right hepatic artery resection survived liver failure, whereas another died after right hemihepatectomy and left hepatic artery resection. We believed that, in regard to hilar cholangiocarcinoma (Bismuth-Corlette type IIIb), left hemihepatectomy concurrent with hepatic artery resection was feasible for our 2 patients.
It is reported that the absence of a hepatic artery blood supply could cause hepatic necrosis and abscess.4,5 However, Majno and colleagues5 pointed out that after artery resection the remnant liver may function adequately with the blood supply from the normal portal flow and collateral vessels, which are considered to be another important system supplying blood and oxygen to the liver. Our first patient had hepatic necrosis 3 months postsurgery. We analyzed its probable cause, which might have been the disruption of the ligaments in the right liver. Our second patient, in whom the collateral arteries in the ligaments were preserved, came through the postoperative period with no events. Anastomotic leakage is another common complication after hemihepatectomy and hepatic artery resection with bile duct reconstruction.4,5 The blood supply to the extrahepatic bile duct comes mainly from the hepatic artery, and the blood supply to the intrahepatic bile duct comes from the collateral arteries, the portal vein and hepatic artery. In our experience, the incidence of bile leakage may decrease if jejunocholedocal anastomosis is rebuilt in a close-to-parenchyma fashion without residual extrahepatic bile duct.
Acknowledgments
Supported by the National Basic Research Program of China (973 Program), grant no 2003CB515501.
Contributors: Drs. Wang and Tang contributed equally to the article. Drs. Wang, Tang and Zheng designed the study. Drs. Wang, Tang, Yao and Liang acquired the data, which Drs. Wang, Tang, Yao, Liang, Jin and Jiang analyzed. Drs. Wang and Tang wrote the article, which Drs. Yao, Liang, Jin, Jiang and Zheng reviewed. All authors approved the article for publication.
Competing interests: None declared.
Accepted for publication Sept. 22, 2007
Correspondence to: Dr. S.-S. Zheng, Department of Hepatobiliary and Pancreatic Surgery, The First Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou 310003, China; fax 86-571-87236628; zhengshs@cae.cn, drtxf@163.com
References
- 1.Dinant S, Gerhards MF, Rauws EAJ, et al. Improved outcome of resection of hilar cholangiocarcinoma (Klatskin tumor). Ann Surg Oncol 2006;13:872-80. [DOI] [PubMed]
- 2.Chamberlain RS, Blumgart LH. Hilar cholangiocarcinoma: a review and commentary. Ann Surg Oncol 2000;7:55-66. [DOI] [PubMed]
- 3.Sakamoto Y, Sano T, Shimada K, et al. Clinical significance of reconstruction of the right hepatic artery for biliary malignancy. Langenbecks Arch Surg 2006;391: 203-8. [DOI] [PubMed]
- 4.Miyazaki M, Ito H, Nakagawa K, et al. Unilateral hepatic artery reconstruction is unnecessary in biliary tract carcinomas involving lobar hepatic artery implications of interlobar hepatic artery and its preservation. Hepatogastroenterology 2000;47:1526-30. [PubMed]
- 5.Majno PE, Pretre R, Mentha G, et al. Operative injury to the hepatic artery. Arch Surg 1996;131:211-5. [DOI] [PubMed]