Abstract
Objective: Hearing loss can significantly impair patient's quality of life, affecting communicative behavior, emotional and social function. This study assesses the impact of hearing aids on the quality of life of patients in a rural area and its correlation with socio-economic factors.
Materials - methods: Thirty patients (18 male, 12 female), with bilateral sensorineural hearing loss of variable etiology, using hearing aid for at least five years, were enrolled in this study. Mean age of subjects was 74 years. This study used the Glasgow Benefit Inventory (GBI) to quantify the changes in quality of life. Patients were divided in above and below criterion group. The criterion used was the median of the air contaction threshold improvement. The binaural use and the type of hearing aids were recorded and correlated with the type of social security service of patients.
Results: Eighty per cent of patients reported significant benefit from the hearing aid use. The majority of patients (90%) used one hearing aid (mean GBI total score 35) and only 10% had binaural hearing aid (mean GBI total score 45). The majority of patients used analog hearing aid (56.5%) while 43.5% used digital hearing aid. Interestingly, it was found that patients did not attend appointments for hearing aids maintenance with a mean follow up of 2.5 years.
Conclusion: This study demonstrates a trend of better quality of life for patients with bilateral hearing loss and binaural hearing aid use. The type of hearing aid is related to the funding from their social security service. Therefore more patients are using analog hearing aids, as they are less expensive than the digital hearing aids.
Keywords: hearing aid, quality of life, socioeconomic aspects
Hearing loss is a common and potentially disabling problem in elderly individuals. Even though over than one-quarter of elderly individuals complain of hearing problems, only one-third of them have significant hearing impairment on audiological testing1. Hearing loss may impair physical and social function, and is associated with cognitive deficits, mood disturbances and behavioral disorders1,2. Hearing aids improve the quality of life; however the benefit from their use is strongly related to the patients social and economic status3. Differences in cost among analog and digital devices and the various funding among social security services are significant factors that affect the choice of hearing aid type. This study assesses the effectiveness of hearing aid intervention assessing the quality of life of patients in relation to the hearing aid type and social security services in a rural area of Northern Greece.
Materials and Methods
In this study 30 consecutive patients were enrolled with bilateral sensorineural hearing loss of variable etiology, who had been using hearing aids. Inculsion criteria were moderate hearing loss (air conduction threshold between 40-70 db4) and use of hearing aids for at least five years (mean time of use 7.4 years). There were 18 male and 12 female patients. Mean age of patients was 74 years (male 73 years old, female 76 years old, range 57-79 years).
This study uses the Glasgow Benefit Inventory (GBI) to quantify the changes in quality of life. The GBI is a generic quality of life questionnaire designed for measuring outcomes after otorhinolaryngological procedures4. It has been validated over a wide range of procedures and is patient oriented5. It measures quality of life in three domains, social, general, and physical. Specifically out of the 18 questions included in GBI, 12 are related to general improvement of quality of life, 3 to social improvement, and 3 to physical improvement. Each of the questions has five possible responses; a response of 5 denotes the most favorable outcome, while a response of 1, the poorest result. A response of 3 denotes no change. The scores are averaged and plotted as a graph with a final range of GBI score from -100 to +100.
GBI uses a criterion to be a measure of technical success based on pure-tone thresholds. The change in average air conduction threshold calculated over 0.5, 1, 2 and 4 kHz. Pre-intervention data derived from the last audiometric measurement before the use of the hearing aids. As post-intervention audiogram was considered the most recently performed. A four-frequency average air conduction threshold was measured pre- and post-intervention for every patient. The differences between the above average numbers were recorded. The median of these differences was considered as the criterion to divide patients in two groups, above and below criterion respectively.
The binaural and monaural use and the type of hearing aids (digital / analog) were recorded and mean total GBI scores were compared for the above parameters.
The type of social security service was also recorded dividing patients in three groups as follows: Patients with funding from the Social Insurance Institute (SII), patients with funding from the Organism of Agricultural Security Services (OASS), and patients with funding from other type of social security service.
Analyses were conducted in SPSS 12.0 (SPSS, Inc., Chicago, IL). Differences between groups with respect to GBI scores were tested using Mann-Whitney U test. All reported p-values are two-tailed with a significance level of 0.05.
Results
All patients reported benefit from the use of hearing aids (positive GBI score). Using as a criterion the median of air conduction threshold improvements we divided patients in two groups above and below criterion respectively. The vast majority of patients (80%) were included to the above criterion group (mean GBI score 38.5 ± 2) and only 20% of them to the below criterion group (mean GBI score 22 ± 4). This difference between GBI means for the two groups was statistically significant (p<0.001). No intersexual differences were found between GBI scores (males: mean GBI score 35.9 ± 3 / females: mean GBI score 36.2 ± 4).
The vast majority of patients used one hearing aid (27 patients, 90%) and only 3 patients had binaural use of hearing aids. Patients with one hearing aid had a mean GBI total score 35 ± 3, and patients with two hearing aids had a mean GBI total score 45 ± 10. Due to small number of patients with binaural hearing aid use, a statistical analysis can not be performed regarding quality of life outcome. However this difference shows a trend especially if we consider that all patients with two hearing aids had the same type of social security service (SII).
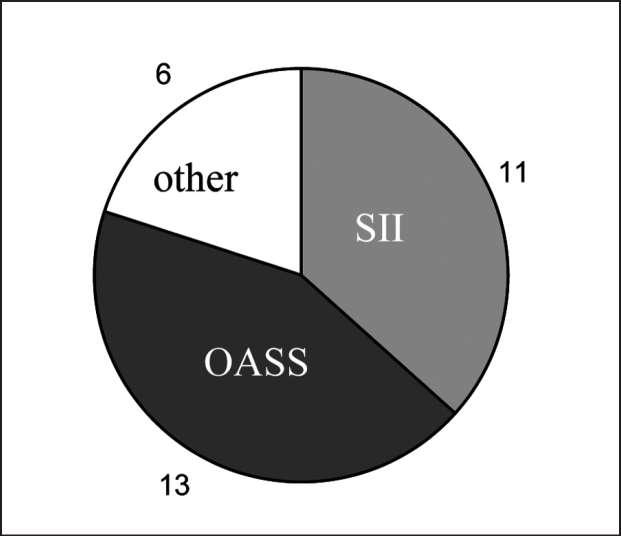
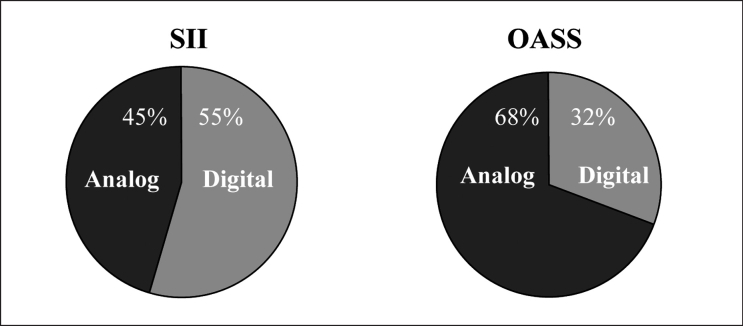
The distribution of patients regarding their type of social security service is shown in figure 1. The number of patients having social security service SII and OASS was similar (11 vs 13 patients respectively) allowing subgroup comparison. In total seventeen patients (56.5%) used analog hearing aids and thirteen patients (43.5%) of used digital hearing aids. The distribution of patients according to their type of social insurance (SII or OASS) and the type of hearing aid is shown in figure 2, where it is obvious that patients with SII security service use digital hearing aids in a greater percentage compared with OASS patients (55% vs 32%).
Figure 1. Distribution of patients according to their type of social security service.
Figure 2. Comparison of digital/analog hearing aid use between SII and OASS social security services.
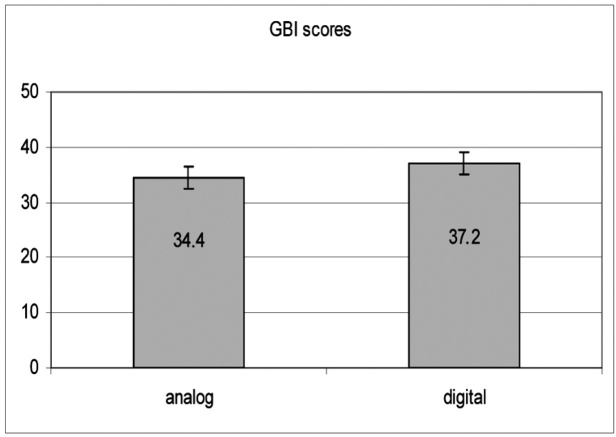
Comparison of mean GBI scores between digital and analog hearind aid users showed a trend towards significance for the use of digital hearing aids (analog 34.4± 3, digital 37.2± 2, p=0.061), (Figure 3).
Figure 3. Comparison of GBI scores between patients using analog and digital hearing aids.
Interestingly, all patients did not attend their regular appointment for hearing aid maintenance every year. The mean period of time between service appointments was 2,5 years. There was no difference between patients with different social security services regarding the hearing aid maintenance appointments.
Discussion
Hearing loss is the most frequently recorded communication handicap in the world and restricts several aspects in the quality of life of patients2. It impairs communication, emotional and social function and can isolate affected people from their family and friends. Hearing impairment has been shown to interfere with patients' ability to live independently and safely having a negative impact on communicative behavior2. Furthermore, it can cause or aggravate depression, anxiety, and feelings of inadequacy, contributing to functional impairment 2.
Elderly individuals who experience hearing impairement seek for expert opinion when they realise that their hearing has deteriorated to an extend that limits their social activity. Another significant factor is the social pressure from family members who are negatively impacted by the individual's hearing loss. Hearing loss usually occurs gradually. By the time the need for hearing aids is recognized, the quality of life may have been significantly impaired.
The average first-time hearing aid wearer is close to 65 years of age1,2 as seen also in our study. Social isolation and inability to follow conversations are much more common among hearing-impaired adults aged 50 years and over, than among non-hearing impaired people in the same age group1.
The impact of hearing impairment on the quality of life can be minimized with the help of hearing aids. The rapid improvement when hearing aids are introduced is well documented6. What is not clearly documented is their long-term effectiveness as many factors may influence their positive impact on patients across their lifespan. Our results showed benefit for all patients from the use of hearing aids. However the scores from the quality of life questionnaires were lower than results recorded in other similar studies7.
Patients with symmetric hearing loss need binaural (ie, both ears) hearing aids1. It has been demonstrated in clinical and laboratory studies that binaural hearing aid wearers may benefit from the ability of the central auditory system to integrate binaural information and enjoy benefits such as binaural loudness summation, masking level difference, localization, and elimination of head-shadow8. Globally about 80% of patients with bilateral severe hearing loss wear hearing aids binaurally9. This fact is not in agreement with our results although we assess patients with moderate hearing loss, and probably affects negatively the quality of life results. If patients with bilateral hearing loss wear only one hearing aid, they cannot identify where a sound is coming from, and in noisy environments, they cannot hear speech clearly. More amplification is usually required with a monaural unit than with binaural units10. Based on these limitations we can speculate that the considerably low quality of life results in our study group are partially due to monaural use of hearing aids. Although the sample of binaural users in our study is small, all of them had the same type of social security and this shows a trend indicating the role of funding differences between social security services for hearing aids.
Hearing aids cost ranges from cheap devices to very expensive devices. Factors that affect the cost are size, circuitry options, circuitry sophistication and add-on options. Analog hearing aids are the most common and least expensive type (range 200-500 euros). Digital hearing aids (digital signal processing units) are the most technologically advanced. They are usually more expensive (range 600-3000 euros) than analog units (2-5 times more expensive). Thus, patients who need basic amplification at the lowest possible price may prefer the analog hearing aids. Our hospital serves an area mainly agricultural. These people usually do not have occupational need of hearing and their social security service does not provide funding for hearing aid expenses. This can explain to a certain point the extended use of analog hearing aids among them.
There is a need for regular follow - up appointments to make sure that the hearing aid is functioning and that the patient is benefiting from its use.The fitting of an aid is not an one-off event. It is therefore essential that there should be a good line of continuing communication between the dispenser and the hearing aid user. In our study all patients had a prolonged period of time between regular follow-up appointments for hearing aid maintenance. This fact may affect negatively the overall impression of the benefit from the hearing aid use. However the cost of hearing aid maintenance has to be met by the patient and this is probably the reason why patients usually do not attend these appointments.
Hearing aid fitting is a cost-effective intervention. In the decade to come, a concerted effort needs to be made by hearing care professionals and the hearing industry to work together to fundamentally change the state's health policy and social security strategy in treating hearing loss.
References
- 1.Wilson PS, Fleming M, Donaldson I. Prevalence of hearing loss among people aged 65 years and over: screening and hearing aid provision. Brit J Gen Practice. 1993;43:406–409. [PMC free article] [PubMed] [Google Scholar]
- 2.Cox RM, Alexander GC, Gray GA. Who wants a hearing aid? Personality profiles of hearing aid seekers. Ear Hear. 2005;26:12–26. doi: 10.1097/00003446-200502000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Vuorialho A, Karinen P, Sorri M. Counselling of hearing aid users is highly cost-effective. Eur Arch Otorhinolaryngol. 2006;263:988–995. doi: 10.1007/s00405-006-0104-0. [DOI] [PubMed] [Google Scholar]
- 4.Robinson K, Gatehouse S, Browning GG. Measuring patient benefit from otorhinolaryngological surgery and therapy. Ann Otol Rhinol Laryngol. 1996;105:415–422. doi: 10.1177/000348949610500601. [DOI] [PubMed] [Google Scholar]
- 5.Arunachalam P, Kilby D, Meikle D, Davison t, Johnson I. Boneanchored hearing aid quality of life assessed by Glasgow Benefit Inventory. Laryngoscope. 2001;111:1260–1263. doi: 10.1097/00005537-200107000-00022. [DOI] [PubMed] [Google Scholar]
- 6.Kochkin S. On the issue of value: Hearing aid benefit, price, satisfaction, and brand repurchase rates. The Hearing Review. 2003;10:12–25. [Google Scholar]
- 7.Mulrow C, Aguilar C, Endicott J, et al. Quality of life changes and hearing impairment: results of a randomized trial. Ann Intern Med. 1990;113:188–194. doi: 10.7326/0003-4819-113-3-188. [DOI] [PubMed] [Google Scholar]
- 8.Briskey RJ, Cole P. Consumer evaluation of binaural hearing aids. Hear Jour. 1983;36:29–31. [Google Scholar]
- 9.Brooks DN, Bulmer D. Survey of binaural hearing aid users. Ear and Hear. 1982:220–224. doi: 10.1097/00003446-198109000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Chung SM, Stephens SDG. Factors influencing binaural hearing aid use. Brit J Aud. 1986;20:129–140. doi: 10.3109/03005368609079006. [DOI] [PubMed] [Google Scholar]