Abstract
Aim: The aim of the present study is the comparison of the results of the appliance of two methods of respiratory physiotherapy; the active cycle of breathing techniques in drainage positions and the conventional physiotherapy, regarding their effects on mucociliary clearance in patients with cystic fibrosis.
Material-methods: Thirty-five children teenagers and adults with cystic fibrosis, 8-20 years of age, with mean Schwachman score 78,49 took part in the research. All patients had regular physiotherapeutic control and applied systematically physiotherapy. The same children received two methods of respiratory physiotherapy in a 3-month random order, when they came at the outpatients' department of the hospital for their regular check-up.
Results: The comparison of the results of the two methods did not show statistical significant difference in sputum quantity, whereas statistical significant difference was noticed in sputum quality after the application of active cycle of breathing techniques.
Conclusions: The application of the active cycle of breathing techniques contributes effectively in the sputum expectoration from the peripheral bronchopulmonary segments and enhances the mucociliary clearance in children with cystic fibrosis.
Keywords: active cycle of breathing techniques, conventional physiotherapy, mucociliary clearance, cystic fibrosis
Mucociliary clearance is the most important defense mechanism of respiratory system, which is responsible mainly for the clearance of secretions from peripheral airways. It is located in the airways from larynx to terminal bronchioles, where ciliary epithelium combines with mucous layer1.
Efficient mucociliary clearance of lung secretions depends on the ideal relationship between ciliated epithelium, periciliary fluid and mucus (viscosity, hydration, ability of attachment e.t.c). A change in one element of this relationship results in a defective mucociliary clearance system2,3.
The optimal relationship between cilia, periciliary layer and mucus is determined by the efficient ions and water transport across the respiratory epithelium, that ensures the hydration and the depth of periciliary layer and the hydration and the viscosity of mucus layer4.
In cystic fibrosis, the characteristic result of the gene defect is the altered chloride ion transport that leads to decreased water transport across the respiratory epithelium5. This sub-optimal water transport is presumed to leave the periciliary and mucus layer in a dehydrated and viscous state, causing the insufficiency of mucociliary clearance. The implications of the defective mucociliary clearance lead to the accumulation of secretions and the airway obstruction with the direct effect of the infection and inflammation by opportunistic bacteria. The progressive airway damage, the respiratory failure and the premature death follow. So the severity of respiratory disease is determinant for the quality and the duration of patient's life6.
The aim of this study is the comparison of the results of the application of conventional physiotherapy and active cycle of breathing techniques in drainage positions, regarding their effect on the mechanism of mucociliary clearance, through the evaluation of sputum.
Patients – Methods
Thirty five (35) children and adults with diagnosed cystic fibrosis, aged 8 to 20 years, took part in the study. The patients came at the outpatients' department of Hippokratio hospital of Thessaloniki for their regular check-up every three months. Their condition was stable and nobody presented with exacerbation of the symptoms. All children received the same two methods of respiratory physiotherapy for approximately 3 months in random order.
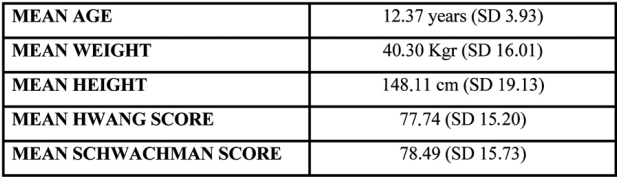
Our sample consisted of 14 boys (40%) and 21 girls (60%) with mean age 12.37 years old (st.a..=3.93). Table 1 summarises the basic characteristics of our sample.
Table 1. Means of the sample in chosen basic characteristics of the children.
1ST METHOD-Conventional physiotherapy combined with respiratory exercises.
The conventional physiotherapy consisted of: postural drainage, percussion, pressure-vibration, cough and active respiratory exercises (unilateral and bilateral, durated 10 min) The treatment was passive and the total duration for all bronchopulmonary segments of both lungs was 50 min. The total duration of each therapy session was 60 min.
2ND METHOD-Active cycle of breathing techniques (ACBT) combined with respiratory exercises.
The active cycle of breathing techniques (ACBT) was performed in drainage positions and contained: diaphragmatic breathing (5 - 10 times), thoracic breathing (4 times deep breathing + 5 sec hold of breath), percussion, pressure-vibration, forced expiration technique or huffing, cough and active respiratory exercises (unilateral and bilateral, durated 10 min). The treatment was active applied by the patients themselves under our control. The duration of the application of ACBT in all positions was 45 min. The total duration of therapy session was 55min.
After the breathing exercises in both methods, followed relaxation with discussion and consultation (15 min) on physiotherapeutic issues, like the childrens posture in sitting and in upright position and the importance of its contribution in normal breathing.
The examination of sputum was done 15 min after the therapy sessions. Sputum was collected in a spittoon during the treatment. Their color was examined. The white and yellow sputum was determined as «light colored» and the green and gray sputum as «dark colored». Then their quantity was determined, by suction of sputum with syringe, as «few»< 1ml, «moderate» > 2 ml and «many» > 3 ml.
The analysis of the results was made by the use of x2- test in the same group. In particular the comparison of the results in mucus measurements-existence, quantity, quality- from the two methods was done.
Results
The results of the comparison of the two methods showed that the groups had the same record regarding the existence of sputum.
The 2nd method is superior to 1st method, as regards as the quantity of mucus, since a great percent of children expectorated larger quantity of "many" sputum after the application of the 2nd method. However this difference is not statistically significant. (Table 2).
Table 2. Comparison of the quantity of the mucus production after the application of the 1st and the 2nd method.
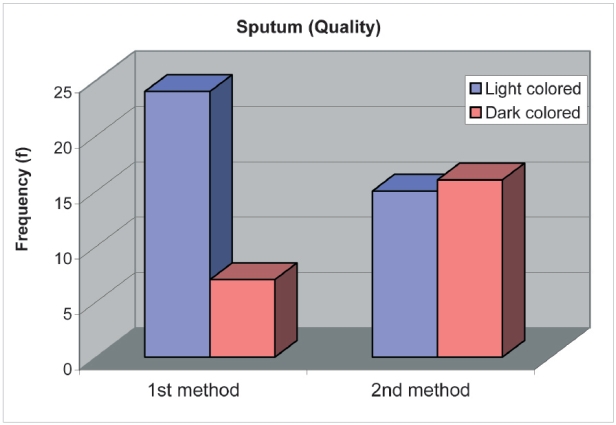
The superiority of the 2nd method is confirmed also by the quality of mucus. The significant difference (x2=5.599, p<.05) of 2nd method comes from the fact that its application caused the expectoration of more dark colored sputum. (Table 3).
Table 3. Comparison of the quality of the mucus production after the application of the 1st and the 2nd method.
Discussion
Expectoration of mucus is the main problem in cystic fibrosis, because the accumulation of copious and viscous secretions leads to the insufficiency of the mechanism of mucociliary clearance, resulting in the progressive lung damage.
Conventional physiotherapy is performed for decades in the treatment of cystic fibrosis and its effectiveness in the removal of mucus has been supported by several studies7.8,9. However, this method presents many disadvantages, since it requires assistance from another person in order to apply percussion and pressure-vibration and there is direct dependence of the patient on the physiotherapist or another person.
These two factors lead to the denial of patients regarding this method, causing the pause of treatment with all bad consequences of lung damage.
Active Cycle of Breathing Techniques (ACBT) is an active and relatively new method, that presents many advantages such as independent application, control of treatment by the patient himself, encouragement of physical activities, psychological support and increase of confidence, that contribute to better compliance of patients in daily treatment with its benefits. Also the ACBT is flexidle and adapted to suit the needs of the individual10,11.
In our study, the results show that active cycle of breathing techniques is superior to conventional physiotherapy in mucus quantity and quality, with significant difference in mucus quality (p<0.05).
The superiority of active cycle of breathing techniques is due to the fact that it combines the drainage positions with the active participation of the patient in thoracic expansion and forced expiratory technique or huffing.
The exercises of thoracic expansion - hold of breath, result in air been transported behind the obstructed areas with better secretion removal.
The forced expiratory technique or huffing12 cause a great compression, which aims to bring the secretions upwards and to activate the cough reflex11.
Drainage positions are applied in the 1st and 2nd method. It is stated in the literature that postural drainage is an effective type of treatment for patients with cystic fybrosis12,13. The active participation of the patient is present only in the second method. We consider that the better results are due to the active participation of the patients, which is absent from the first method. It is also stated in the literature that the combination of drainage positions with an active technique like the ACBT has better results in lung function and sputum expectoration11 and this is also confirmed by our study.
According to the results of the present study we recommend the instruction of active cycle of breathing techniques in children with cystic fibrosis, because better mucociliary clearance is achieved, resulting in better pulmonary function, reduction of complications and delay of disease process. The application in drainage position helps all bronchopulmonary segments to be cleared2.
Figure 1. Application of pressure and vibration from the physiotherapist.
Figure 2. Application of pressure and vibration from the child.
References
- 1.Oski AF, DeAngelis DC, Feigin DR, McMilian AJ, Warshaw BJ. Principles and practice of pediatrics. 2nd. Philadelphia: Lippincott; 1994. [Google Scholar]
- 2.Nelson EW, Behrman ER, Vaughan CV. Textbook of Pediatrics. 13th ed. Philadelphia: Saunders; 1987. [Google Scholar]
- 3.Pryor JC. Key Issues in cardiorespiratory physiotherapy. Oxford: Butterworth-Heimann; 1992. Mucociliary clearance; pp. 105–130. [Google Scholar]
- 4.Frizzell RA. Role of absorptive and secretory processes in hydration of the airway surface. Am Rev Respir Dis. 1988;138:S3–6. doi: 10.1164/ajrccm/138.6_Pt_2.S3. [DOI] [PubMed] [Google Scholar]
- 5.Cuthbert AW. Cystic fibrosis 4. Abnormalities of airways epithelial function and the implications of the discovery of the cystic fibrosis gene. Thorax. 1991;46:124–130. doi: 10.1136/thx.46.2.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boucher RC, Van ScottMR, Willumsen N, Stutts MJ. Epithelial injury. Mechanisms and cell biology of airway epithelial injury. Am Rev Respir Dis. 1988;138:S41–44. doi: 10.1164/ajrccm/138.6_Pt_2.S41. [DOI] [PubMed] [Google Scholar]
- 7.Fauroux B, Boule M, Lofaso F, et al. Chest physiotherapy in cystic fibrosis: improved tolerance with nasal pressure support ventilation. Pediatrics. 1999;103:E32. doi: 10.1542/peds.103.3.e32. [DOI] [PubMed] [Google Scholar]
- 8.Feldman J, Traver GA, Taussing LM. Maximal expiratory flows after postural drainage. Am Rev Respir Dis. 1979;119:239–245. doi: 10.1164/arrd.1979.119.2.239. [DOI] [PubMed] [Google Scholar]
- 9.Oermann CM, Swank PR, Sockrider MM. Validation of an instrument measuring patient satisfaction with chest physiotherapy techniques in cystic fibrosis. Houston. 2000;118:92–97. doi: 10.1378/chest.118.1.92. [DOI] [PubMed] [Google Scholar]
- 10.Cecins NM, Jenkins SC, Pengelley J, Ryan G. The active cycle of breathing techniques- to tip or not to tip? Respir Med. 1999;93:660–665. doi: 10.1016/s0954-6111(99)90107-5. [DOI] [PubMed] [Google Scholar]
- 11.Orlik T. Evaluation of the efficiency of selected thoracic physiotherapy methods used in the treatment of patients with cystic fibrosis. Med Wieku Rozwoj. 2000;4:233–246. [PubMed] [Google Scholar]
- 12.Kirrilloff LH, Owens GR, Rogers RM. Does chest physical therapy work? Chest. 1985;88:436–444. doi: 10.1378/chest.88.3.436. [DOI] [PubMed] [Google Scholar]
- 13.Lannefors L, Wollmer P. Mucus clearance with three chest physiotherapy regimes in cystic fibrosis: a comparison between postural drainage, PEP and physical exercise. Eur Respir J. 1992;5:748–753. [PubMed] [Google Scholar]