Abstract
Background: Diabetes mellitus is associated with a variety of musculoskeletal disorders. The prevalence of connective tissue disorders in these patients has increased in the recent years affecting significantly their quality of life.
Methods - Results: We conducted a pilot study including 208 sequentially selected patients with type 2 diabetes mellitus regularly followed-up at the Diabetes Center of the Hippokration University Hospital. Among the diabetic patients who were screened according to the Short Musculoskeletal Function Assessment Questionnaire for musculoskeletal symptoms and findings, 82.6% were found to exhibit musculoskeletal abnormalities, mainly of the degenerative, noninflammatory type.
Conclusions: Musculoskeletal disorders are a common finding among patients with type 2 diabetes. Obesity and accumulation of abnormally glycosylated byproducts have been proposed as potential pathogenetic mediators of these connective tissue abnormalities. Of particular interest is, however, the common association of osteoarthritis, involving even non-weight bearing joints in patients with type 2 diabetes, indicating a common pathophysiologic mechanism connecting these two clinical conditions.
Keywords: musculoskeletal disorders, diabetes mellitus, prevalence
Diabetes mellitus (DM) affects connective tissues in many ways and causes different alterations in periarticular and skeletal systems1,2. Several musculoskeletal disorders have been described in these patients which can be divided into three categories: a. disorders which represent intrinsic complications of diabetes, such as limited joint mobility or diabetic cheiroarthropathy, stiff hand syndrome, and diabetic muscular infarction, b. disorders with an increased incidence among diabetics, such as Dupuytrens disease, shoulder capsulitis, neuropathic arthropathy, osteopenia (in type 1 DM), flexor tenosynovitis, septic arthritis, acute proximal neuropathy, proximal motor neuropathy, pyomyositis and the diffuse idiopathic skeletal hyperostosis (DISH) syndrome, the diagnosis of which depends on the radiographic recognition of a minimum of two bridges connecting three consecutive vertebrae in diabetics usually complaining of backache, and finally c. disorders for which a possible association with diabetes has been proposed but not proven yet, such as osteoarthritis and the carpal tunnel syndrome1.
The aim of our study was to investigate the prevalence of musculoskeletal disorders in patients with type 2 diabetes mellitus followed up at the Diabetes Center of the 2nd Propedeutic Department of Internal Medicine of the Hippokration University Hospital with the aid of the Short Musculoskeletal Function Assessment Questionnaire, and to compare the results with results previously published from studies performed in other populations.
Two hundred and eight (208) sequentially selected type 2 diabetics, regularly followed up at the Diabetes Center of the Hippokration University Hospital in Thessaloniki, Greece, and residents both of the rural as well as the urban areas of the prefecture of Thessaloniki, were included in the study. Eighty nine patients were men and 119 women. The mean age of the patients was 66.3 years ranging from 36 to 87 years and the mean duration of the primary disease was 10.1 years. Diabetes was moderately controlled with a mean glycosylated HbA1C value of 7.6% prior to inclusion in the study.
All patients were evaluated at the Rheumatology Outpatient Clinic of the 2nd Propedeutic Department of Internal Medicine of the Hippokration General Hospital. Evaluation was performed according to the Short Musculoskeletal Function Assessment Questionnaire (SMFA). This questionnaire was developed by Swiontkowski et al 19993 based on the Musculoskeletal Function Assessment questionnaire, which due to its length (101 questions) is mainly used for research purposes4. It was designed to study differences in the functional status of patients with a broad range of musculoskeletal disorders. It consists of two parts; the first part is a dysfunction index addressing the issue of how much dysfunction these patients are encountered with in their daily activities, with an emphasis on the function and mobility of the arm and hand, and how much their dysfunction affects their emotional status; the second part is a bother index designed to address the issue of to what extent these patients are bothered by their dysfunction in their recreation and leisure, sleep and rest, work and family. The Short Musculoskeletal Function Assessment Questionnaire represents a valid, reliable and responsive instrument for clinical assessments and is recommended by the American Academy of Orthopaedic Surgeons5. Upon completion of the questionnaire and clinical examination of the patients' laboratory tests, imaging analysis and histopathological analysis of tissue samples were requested and evaluated in the cases considered appropriate.
Results
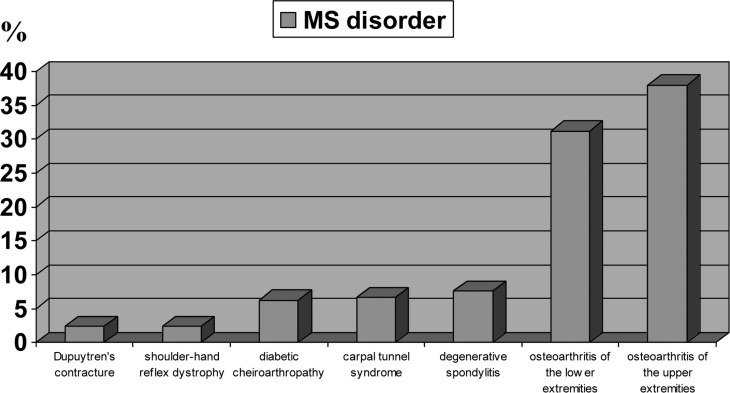
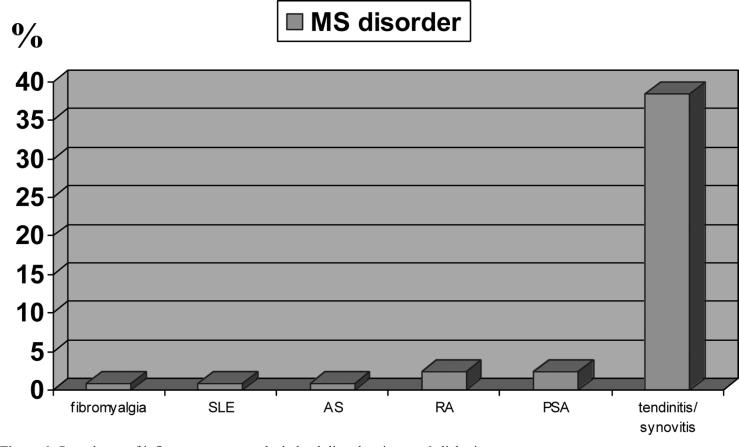
Eighty two point six percent (82.6%) of the type 2 diabetics evaluated in this study were found to have specific musculoskeletal disorders, while only 17.3% of the patients were symptom-free. Degenerative, non-inflammatory abnormalities (osteoarthritis, degenerative spondylitis, carpal tunnel syndrome, diabetic cheiroarthropathy, etc.) exhibited a significant overall higher prevalence rate among these disorders than inflammatory disorders (Figure 1 vs Figure 2). The most frequently encountered musculoskeletal disorders in these patients were osteoarthritis and enthesopathy (mainly flexor tenosynovitis). Interestingly, joints affected by osteoarthritis were not only weight-bearing joints of the lower extremities, but equally frequently joints of the upper extremities (31.2% vs 38%). The incidence rate of inflammatory rheumatological disorders, such as rheumatoid arthritis, did not differ significantly among diabetics (2.4%) and the background population (up to 5%)6
Figure 1. Prevalence of various non-inflammatory musculoskeletal disorders in type 2 diabetics.
Figure 2. Prevalence of inflammatory musculoskeletal disorders in type 2 diabetics SLE: systemic lupus erythematosus, AS: ankylosing spondylitis, RA: rheumatoid arthritis, PsA: psoriatic arthritis.
Discussion
Musculoskeletal disorders are common in type 1 and 2 diabetic subjects, and examination of periarticular regions of the hands, the joints, shoulders and feet, as well as the skeleton, should be included in the evaluation of patients with DM. Most musculoskeletal complications seem to be associated with the duration of DM and appear in diabetic patients of younger age than their counterparts in the general population6. Musculoskeletal disorders in these patients are probably related to the long-term glycaemic control of the diabetes. However, no direct association could be proven with the metabolic control of the disease.
The pathophysiology of these disorders in diabetic patients is not obvious. It could be associated with connective tissue disorders, such as the formation of abnormally glycosylated end products or the impaired degradation of byproducts, it could be indirectly related to the vasculopathy and neuropathy commonly complicating the primary disease, or finally, it could be attributed to a combination of factors. Studies comparing the incidence of specific musculoskeletal disorders between type 1 and type 2 diabetic patients did not show significant differences between the two groups, despite the substantial difference in the mean age of the patients in the two groups.
Musculoskeletal disorders were more common in patients with type 1 than type 2 diabetes. However, the type of diabetes was not associated with hand and shoulder syndromes after adjusting for the duration of the disease7. The prevalence rates for these disorders among diabetic patients vary between the different published studies with our rates of non-inflammatory disorders reaching slightly lower levels7–11. We believe that this difference can be attributed to the more accurate recognition of inflammatory rheumatological conditions, underestimated in analogous studies, as well as to intrinsic characteristics of the Greek population.
Of particular interest is the possible pathogenetic association of osteoarthritis and diabetes mellitus. In our pilot study including a relatively small yet indicative number of patients the prevalence of osteoarthritis in type 2 diabetic patients was found to be significantly higher than the estimated prevalence in the general Greek population12.
In a large study on osteoarthritis including 1026 patients, the mean fasting glucose concentration was higher in subjects with osteoarthritis (OA) than in subjects without OA, but DM was present in only 5.5% of the subjects13. Such an increased propensity for the development of OA, especially in type 2 diabetic subjects, could be due to the obesity rather than to DM. The fact that OA even of non-weight-bearing joints, i.e. of the hand, is significantly more frequent in diabetics compared to non-diabetics however, argues in favour of a common pathogenetic mechanism connecting the two disorders. Overall, an association between DM and OA seems to exist and additional studies including a larger number of patients, and directly comparing osteoarthritic findings in diabetics and non-diabetics will be needed to verify and explore the pathophysiology of the connection of the two disorders.
References
- 1.Arkkila PE, Gautier JF. Musculoskeletal disorders in diabetes mellitus: an update. Best Pract Res Clin Rheumatol. 2003;17:945–970. doi: 10.1016/j.berh.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Cagliero E. Rheumatic manifestations of diabetes mellitus. Curr Rheumatol Rep. 2003;5:189–194. doi: 10.1007/s11926-003-0065-x. [DOI] [PubMed] [Google Scholar]
- 3.Swiontkowski MF, Engelberg R, Martin DP, Agel J. Short musculoskeletal function assessment questionnaire: validity, reliability and responsiveness. J Bone Joint Surg Am. 1999;81:1245–1260. doi: 10.2106/00004623-199909000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Engelberg R, Martin DP, Agel J, Swiontkowski MF. Musculoskeletal function assessment: reference values for patient and nonpatient samples. J Orth Res. 1999;17:101–109. doi: 10.1002/jor.1100170116. [DOI] [PubMed] [Google Scholar]
- 5.Ponzer S, Skoog A, Bergstrom G. The short musculoskeletal function assessment questionnaire (SMFA): cross-cultural adaptation, validity, reliability and responsiveness of the Swedish SMFA (SMFA-Swe) Acta Orthop Scand. 2003;74:756–763. doi: 10.1080/00016470310018324. [DOI] [PubMed] [Google Scholar]
- 6.Brown MA. Antibody treatments of inflammatory arthritis. Curr Med Chem. 2005;12:2943–2946. doi: 10.2174/092986705774462842. [DOI] [PubMed] [Google Scholar]
- 7.Cagliero E, Apruzzese W, Perlmutter GS, Nathan DM. Musculoskeletal disorders of the hand and shoulder in patients with diabetes mellitus. Am J Med. 2002;112:487–490. doi: 10.1016/s0002-9343(02)01045-8. [DOI] [PubMed] [Google Scholar]
- 8.Starkman HS, Gleason RE, Rand LI, Miller DE, Soeldner JS. Limited joint mobility (LJM) of the hand in patients with diabetes mellitus: relation to chronic complications. Ann Rheum Dis. 1986;45:130–135. doi: 10.1136/ard.45.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pal B, Anderson J, Dick WC, Griffiths ID. Limitation of joint mobility and shoulder capsulitis in insulin- and non-insulin-dependent diabetes mellitus. Br J Rheumatol. 1986;25:147–151. doi: 10.1093/rheumatology/25.2.147. [DOI] [PubMed] [Google Scholar]
- 10.Sukenik S, Weitzman S, Buskila D, Eyal A, Gross J, Horowitz J. Limited joint mobility and other rheumatological manifestations in diabetic patients. Diabetes Metabolism. 1987;13:187–192. [PubMed] [Google Scholar]
- 11.Fitzcharles MA, Duby S, Waddell RW, Banks E, Karsh J. Limitation of joint mobility (cheiroarthropathy) in adult noninsulin-dependent diabetic patients. Ann Rheum Dis. 1984;43:251–254. doi: 10.1136/ard.43.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andrianakos AA, Kontelis LK, Karamitsos DG, et al. Prevalence of symptomatic knee, hand, and hip osteoarthritis in Greece. The ESORDIG study. J Rheumatol. 2006;33:2507–2513. [PubMed] [Google Scholar]
- 13.Cimmino MA, Cutolo M. Plasma glucose concentration in symptomatic osteoarthritis: a clinical and epidemiological survey. Clin Exp Rheumatol. 1990;8:251–257. [PubMed] [Google Scholar]