Abstract
Ceramic femoral heads have been used in an attempt at reducing polyethylene wear of total hip arthroplasties. Clinical results with zirconia femoral heads have been mixed. This study was undertaken to compare the polyethylene wear and incidence of periprosthetic osteolysis in total hip replacements performed using a 28-mm zirconia versus a 28-mm cobalt chromium femoral head. Thirty-five hips with a 28-mm cobalt chromium head and 68 hips with a 28-mm zirconia head were evaluated after a minimum follow-up of 2 years (average, 4.0 years; range, 2.0 to 9.1 years). A monoblock acetabular component was used in all patients. Polyethylene wear was measured in serial radiographs from 58 of the hips utilizing a computer-assisted vector wear technique. Periacetabular osteolysis developed in three patients (two with a zirconia head and one with a cobalt chromium head). The total wear and the annual wear rate were 0.48 mm and 0.11 mm/year for the cobalt chromium heads and 0.53 mm and 0.14 mm/year for the zirconia heads, respectively. We found no benefit with respect to the rate of polyethylene wear or incidence of osteolysis with the use of zirconia femoral heads.
Keywords: polyethylene wear, zirconia, cobalt chrome, femoral head
Introduction
Polyethylene wear and wear-related osteolysis continue to be important factors limiting the longevity of total hip Arthroplasties (THAs) [15, 22, 25]. A direct relationship between polyethylene wear and the prevalence of periprosthetic osteolysis and component loosening has been confirmed [7, 9, 22, 24].
In an attempt to reduce polyethylene wear, zirconia ceramic femoral heads have been used as an alternative bearing surface. The theoretical reduction in wear with the use of zirconia femoral heads is based on their high surface hardness, high compressive strength, high wettability, and superior surface polish [21]. Relatively low wear rates associated with the use of zirconia have been observed clinically in a small, mostly male population [15] and with 22-mm heads [26].
However, with zirconia ceramic, the potential exists for late phase transformation and aging, resulting in grain pullout, surface cracking, and increasing surface roughness [4, 8, 23, 28]. Zirconia ceramic has three phases of physical structure. The tetragonal phase has the greatest mechanical strength and is used for the manufacture of prosthetic femoral heads, but it is also the most unstable phase with possible surface transformation back into the more stable monoclinic phase [11, 12]. Phase transformation can result from cyclic contact loading at pressures that are commonly found in the hip [28], as well as from contact with water and body fluids [3, 27]. In one study of 52 retrieved zirconia heads, the monoclinic content within the bearing surface averaged 40% compared with 3% in nonimplanted heads [8]. The broader clinical relevance of this retrieval study can be brought into question due to a lack of correlation with clinical wear and osteolysis, the effect of third-body debris, and the inclusion of only failed components in the series.
Increased polyethylene wear rates in THAs with zirconia femoral heads have been observed clinically [13, 14, 16, 18]. Longevity of THAs with zirconia heads has been questioned by a report of a poor survival rate (63%) in a series of 78 THAs with a zirconia-on-polyethylene bearing at 5.8 years’ follow-up [2].
To date, few studies have been reported comparing the polyethylene wear rates of THAs with zirconia and cobalt chromium femoral heads using the same manufacturer for the polyethylene acetabular component and a common femoral head size. The purpose of this study was to measure any differences in polyethylene wear and prevalence of periprosthetic osteolysis in THAs performed with zirconia or cobalt chromium femoral heads.
Materials and methods
One hundred three total hip replacements in 91 patients 70 years old or younger who underwent THA between August 1998 and April 2005 by a single orthopedic surgeon (CNC) were retrospectively reviewed. To be included in this series, patients had to have at least 2 years of follow-up. A variety of cemented or uncemented femoral components were used, but all THAs were performed using the Trabecular Metal™ Monoblock Acetabular Cup System (Zimmer, Warsaw, IN, USA) and either a 28-mm cobalt chromium or zirconia femoral head.
No standardized criteria were employed for selecting metal or ceramic femoral heads, although younger patients were more likely to receive a zirconia head. A cobalt chromium femoral head was used in 35 hips (34%) and a zirconia ceramic head in 68 hips (66%). There were 58 women and 33 men. Patient height, weight, and body mass index (BMI) were similar between those receiving cobalt chromium or zirconia heads, but the group receiving zirconia heads had a younger average age (p = 0.001) and had more males (p = 0.04). The length of follow-up was longer (p = 0.005) for the cobalt chromium group, averaging 4.6 versus 3.6 years in the zirconia group (Table 1).
Table 1.
Patient demographics: overall refers to the entire data series, combining both cobalt chrome and zirconia
| Head type | N (hips) | Sex | Age (years) | Height (cm) | Weight (kg) | BMI | Average length of F/U (years) |
|---|---|---|---|---|---|---|---|
| Cobalt chrome | 35 | 9 Male | 62.1 | 166.5 | 84.2 | 30.3 | 4.6 |
| 26 Female | |||||||
| Zirconia | 68 | 29 Male | 53.2 | 169.0 | 82.9 | 28.9 | 3.6 |
| 39 Female | |||||||
| p value | 0.04 | 0.001 | 0.3 | 0.8 | 0.4 | 0.005 | |
| Overall | 103 | 38 Male | 56.3 | 168.1 | 83.3 | 29.4 | 4.0 |
| 65 Female | |||||||
The preoperative diagnosis was osteoarthritis in 82 hips, avascular necrosis in 10, posttraumatic arthritis in five, developmental dysplasia in three, and rheumatoid arthritis in three. The right side was affected in 57 hips and the left side in 46.
Surgery was performed through a posterolateral approach and with an enhanced soft tissue repair. The diameter of the femoral head was 28 mm in all cases. Patients received either a cemented femoral stem or a proximally hydroxyapatite-coated press fit stem.
Patients were asked to return for routine radiographic examination at 6 weeks, 3 months, 12 months, 24 months, and biannually thereafter. All standing radiographs were evaluated and measured for inclination, anteversion, and wear by a single observer (RMC) who was not involved in the surgeries. Osteolysis and fixation were evaluated in all films by one of the authors (AGDV) who did not participate in the surgeries.
We determined cup inclination from standing radiographs obtained at 6 weeks follow-up utilizing a horizontal reference line through the base of both teardrops using a digital protractor with a precision of 0.1° (X-Caliper® Digital Measuring System, Eisenlohr Technologies, Davis, CA, USA). Anteversion was calculated according to the method of Ackland et al. [1] from the standardized radiograph obtained 6 weeks after surgery. This initial radiograph was compared to that obtained at the last follow-up to determine radiographic fixation, total wear, annual wear rate, and the presence, extent, and location of osteolysis [6].
Radiographic osteolysis was defined as punched-out areas devoid of trabecular bone, usually with a sclerotic border. Osteolytic lesions of the acetabulum were located according to the zones of De Lee and Charnley [5] and those of the femur according to the zones of Gruen [10]. Calcar resorption was defined as rounding of the calcar with a convex shape and loss of calcar–collar contact. It was differentiated from calcar osteolysis, which was defined as a punched-out, expansive area with a concave shape [6].
The total penetration and annual wear rate were determined by comparing the standing anteroposterior radiograph obtained 6 weeks after surgery with all subsequent follow-up radiographs, utilizing the computer-assisted vector wear technique described by Martell and Berdia [20]. Radiographs were digitized using a digital X-ray scanner (Diagnostic Pro™ Plus; Vidar Systems, Herndon, VA, USA). To correctly define the circumference of the femoral head, only radiographs where a portion of the perimeter of the femoral head was visible both medial and lateral to the femoral neck were used in the wear analysis (Fig. 1). Due to the radioopacity of the tantalum monoblock cup, the perimeter of the femoral head could not be visualized within the socket in 45 hips. Consequently, wear measurements could not be performed on these 45 hips. Total and annual wear measurements were performed on the remaining 58 hips (56.3% of the study population), 22 hips articulating with a cobalt chromium femoral head and 36 with a zirconia head. Wear was measured on these 58 hips at the last follow-up and all intermediate follow-up visits for a total of 176 wear measurements.
Fig. 1.
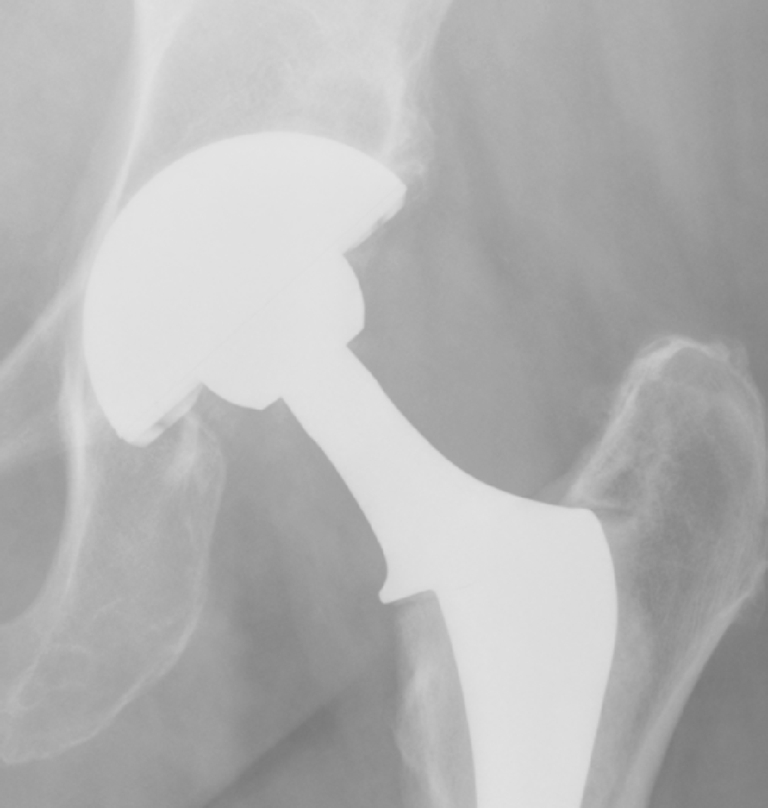
A radiograph of a THA in which wear could be measured since a portion of the circumference of the femoral head was visible both medial and lateral to the femoral neck
The intraobserver consistency of the wear measurements was calculated as the average 95% confidence interval (CI) of five wear measurements performed on different days for three different patients for a total of 15 measurements [9]. The 95%CI for the wear measurements was 0.031 mm/year (range, 0.020–0.046 mm/year).
Correlations between normally distributed variables (age, height, weight, BMI, inclination, anteversion, and wear rate) were examined using Pearson’s correlation coefficient, r. All other correlations were done using Spearman’s rank correlation, rho. A correlation of greater than 0.4 is considered at least a moderate correlation. Comparisons between two groups on normally distributed data, such as age and wear rate, were done using t tests. For more than two groups, a one-way analysis of variance (ANOVA) was used. Comparisons between two or more groups of ordinal variables, such as gender and head type, or among non-Gaussian distributed data were done using a Kruskal–Wallis test.
Results
All cups achieved radiographic fixation at the last follow-up. Among the 103 hips with complete radiographic follow-up, all were well-fixed and had bone ingrown. The average inclination of the cup was 45.2° (SD, 7.3°; range, 20.8–62.1°). Anteversion averaged 14° (SD, 6.5°; range, 0–41°). Five of the 103 hips (4.9%) in the study cohort underwent reoperation with only one hip (1.0%) requiring revision of the acetabular monoblock component. Reoperation occurred in two cases for periprosthetic fracture of the femoral component, one for leg length discrepancy, one for recurrent dislocation, and one for instability of the acetabular cup. There were no revisions for infection.
We observed no significant difference in total wear (p = 0.5), annual wear rate (p = 0.07), or prevalence of osteolysis (p = 0.99) between cobalt chromium and zirconia femoral heads (Tables 2 and 3). An ANOVA with wear as the dependent variable, time since surgery as a covariate, and head type as an independent factor was also not significant (p = 0.1), indicating that head type did not influence wear in this series.
Table 2.
Total wear and annual wear rate for cobalt chrome and zirconia femoral heads
| Head type | N | Total wear (mm) | SD | Range (mm) | 95% Confidence interval | p value |
|---|---|---|---|---|---|---|
| Cobalt chrome | 22 | 0.48 | 0.30 | 0.19–1.19 | 0.35–0.62 | 0.5 |
| Zirconia | 36 | 0.53 | 0.30 | 0.11–1.54 | 0.43–0.62 |
Table 3.
Total wear and annual wear rate for cobalt chrome and zirconia femoral heads
| Head type | N | Annual wear (mm/year) | SD | Range (mm) | 95% Confidence interval | p value |
|---|---|---|---|---|---|---|
| Cobalt chrome | 22 | 0.11 | 0.06 | 0.04–0.27 | 0.09–0.14 | 0.07 |
| Zirconia | 36 | 0.14 | 0.06 | 0.20–0.32 | 0.12–0.16 |
Osteolysis was present in three hips (2.9%) at the last follow-up. Osteolysis developed in one patient with a cobalt chromium femoral head (2.9%) located in the proximal femur in zones 1 and 7. Two patients with a zirconia femoral head (2.9%) developed osteolysis in the acetabulum, one in zone 1 and one in zone 2. The three patients who developed osteolysis had a similar average age (p = 0.2), height (p = 0.9), weight (p = 0.2), and BMI (p = 0.3) as those patients who did not develop osteolysis. Total wear (p = 0.7) and annual wear rate (p = 0.1) did not differ significantly in patients with radiographic evidence of osteolysis compared with patients who had no evidence of osteolysis.
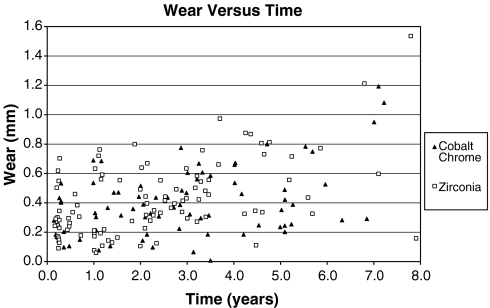
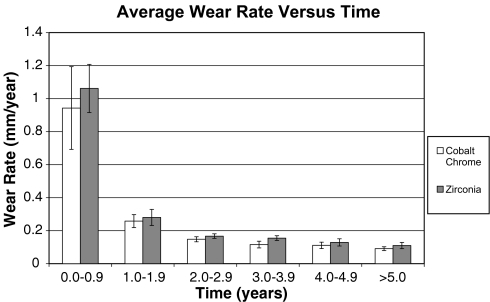
When all 176 postoperative radiographs were analyzed, a significant correlation between wear and time since surgery (r = 0.47, p = 0.001) and a significant decrease in wear rate over time (r = −0.55, p = 0.001) were found (Fig. 2). When the groups were analyzed separately, cobalt chromium heads demonstrated an increase in wear over time (r = 0.64, p = 0.001) and a decrease in wear rate over time (r = −0.63, p = 0.002). These trends were also observable with zirconia heads, which demonstrated an increase in wear over time (r = 0.64, p = 0.001) and a decrease in wear rate over time (r = −0.58, p = 0.001) (Fig. 3).
Fig. 2.
A scattergram plot of total wear as a function of time since surgery for cobalt chromium and zirconia femoral heads showing similar wear over time
Fig. 3.
The average wear rate plotted as a function of time of follow-up for each postoperative year for cobalt chromium and zirconia femoral heads. The decreasing height of the bars over time suggests that the wear rate was not constant but decreased over time. The bars represent the standard error
Polyethylene wear was not associated with sex, age, height, weight, or BMI. Poor correlations existed between the annual wear rate and age (p = 0.9), height (p = 0.8), weight (p = 0.4), BMI (p = 0.5), inclination of the cup (p = 0.2), and anteversion of the cup (p = 0.2) (Tables 4 and 5).
Table 4.
Relationship between annual wear rate and patient variables
| Sex | Total wear (mm±SD) | Annual wear rate (mm/year±SD) |
|---|---|---|
| Males | 0.56 ± 0.28 | 0.14 ± 0.06 |
| Females | 0.47 ± 0.31 | 0.12 ± 0.05 |
| p value | 0.15 | 0.1 |
Table 5.
Relationship between annual wear rate and patient variables
| Variable | Correlation with annual wear rate (r) | p value |
|---|---|---|
| Age | 0.05 | 0.9 |
| Height | 0.15 | 0.9 |
| Weight | 0.14 | 0.9 |
| BMI | 0.07 | 0.9 |
| Inclination | 0.13 | 0.9 |
| Anteversion | 0.05 | 0.9 |
Discussion
This study was initiated to evaluate the difference in wear and prevalence of osteolysis in THAs performed using cobalt chromium and zirconia femoral heads. This study failed to detect any difference in osteolysis, total wear, or annual wear rate between cobalt chromium and zirconia femoral heads articulating with an identical acetabular component (Zimmer Monoblock Cup).
The study has several strengths. We report on a single surgeon series in which the THAs were implanted with identical surgical technique. All patients received the same acetabular cup and a 28-mm prosthetic femoral head. The population for this study was limited to those patients who were 70 years old or younger at the time of operation. It has been well-documented that younger patients are more active after THA, leading to increased wear and osteolysis. A study of 1,081 primary THAs found that no patients who were older than 70 years at the time of operation developed osteolysis or had revision surgery in the first 10 years after their operation, while 22% of patients younger than 50 years developed pelvic osteolysis over the same time period [19]. We thus limited our study population to those patients 70 years of age and younger to report on the rates of wear and osteolysis in a more active patient cohort.
This study represents an early report of wear and osteolysis and has some weaknesses. Follow-up was short and the sample size was slightly underpowered. A power analysis showed approximately 60 patients would be needed in each group to detect a 20% difference in wear [17]. Additionally, the vector wear technique may not be sensitive enough to accurately measure small amounts of wear in the early follow-up period. A longer follow-up period, resulting in greater amounts of total wear, would help improve the accuracy of the measurements with this technique. Moreover, since zirconia and cobalt chromium femoral heads have a different radiographic appearance, it is impossible to blind the observer measuring wear, resulting in a potential for bias. Nevertheless, we believe that the differences in wear measured in this study are quite small and of no clinical importance.
The cohorts in this study were not randomized and, on average, patients in the zirconia group were younger, male, and had shorter follow-ups than patients in the cobalt chromium group, although they had comparable height, weight, and BMI. Since both age and male gender have been associated previously with increased wear rates [6], it is conceivable that the zirconia group was predisposed to greater wear.
We observed no difference in wear characteristics or rate of osteolysis in these THAs regardless of whether a cobalt chromium or zirconia ceramic femoral head was used, confirming the results of a previous randomized trial [17]. We found the total wear and the annual wear rate with a cobalt chromium head to be 0.48 mm and 0.11 mm/year and with the zirconia head to be 0.53 mm and 0.14 mm/year, respectively. A decrease in wear rate occurred over time, suggesting that the true wear rate was not linear. Such a phenomenon has been described previously [13]. One possible explanation is that the high initial rate of femoral head penetration may be due to creep of the polyethylene or bedding in of the femoral head and may not represent true polyethylene wear. A decrease in polyethylene wear over time with zirconia femoral heads has been observed for the first four postoperative years followed by a subsequent increase in the wear rate from the fifth to 12th postoperative years [13]. In our series, the zirconia group demonstrated a decrease in wear rate over time with an average follow-up of 3.5 years. A longer follow-up period may be necessary to observe a possible increase in polyethylene wear rate from phase transformation of zirconia femoral heads. We agree with previous authors [14, 16, 17]. In view of the potential for deleterious phase change of zirconia femoral heads and the similar early wear observed when cobalt chromium and zirconia heads are compared, the use of zirconia femoral heads in THAs seems unwarranted.
Acknowledgments
The authors thank Hilary Gamble for her help in preparing this manuscript.
References
- 1.Ackland MK, Bourne WB, Uhthoff HK (1986) Anteversion of the acetabular cup: measurement of angle after total hip replacement. J Bone Jt Surg Br 68:409–413 [DOI] [PubMed]
- 2.Allain J, Le Mouel S, Goutallier D, Voisin MC (1999) Poor eight-year survival of cemented zirconia-polyethylene total hip replacements. J Bone Jt Surg Br 81:835–842, doi:10.1302/0301-620X.81B5.9454 [DOI] [PubMed]
- 3.Chevalier J, Cales B, Drouin JM (1999) Low-temperature aging of Y-TZP ceramics. J Am Ceram Soc 82:2150–2204
- 4.Chowdhury S, Vohra YK, Lemons JE, Ueno M, Ikeda J (2007) Accelerating aging of zirconia femoral head implants: change of surface structure and mechanical properties. J Biomed Mater Res B Appl Biomater 81:486–492 [DOI] [PubMed]
- 5.DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 121:20–32 [PubMed]
- 6.Della Valle AG, Doty S, Gradl G, Labissiere A, Nestor BJ (2004) Wear of a highly cross-linked polyethylene liner associated with metallic deposition on a ceramic femoral head. J Arthroplasty 19:532–536, doi:10.1016/j.arth.2003.12.065 [DOI] [PubMed]
- 7.Dumbleton JH, Manley MT, Edidin AA (2002) A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty 17:649–661, doi:10.1054/arth.2002.33664 [DOI] [PubMed]
- 8.Fernandez-Fairen M, Sala P, Gil FJ (2006) Failures of yttria-stabilised tetragonal zirconia: 52 retrieved ceramic femoral heads of total hip prostheses. Biomed Mater Eng 16:415–422 [PubMed]
- 9.Gonzalez Della Valle A, Su E, Zoppi A, Sculco TP, Salvati EA (2004) Wear and periprosthetic osteolysis in a match-paired study of modular and nonmodular uncemented acetabular cups. J Arthroplasty 19:972–977, doi:10.1016/j.arth.2004.06.001 [DOI] [PubMed]
- 10.Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 141:17–27 [PubMed]
- 11.Hamadouche M, Sedel L (2000) Ceramics in orthopaedics. J Bone Jt Surg Br 82:1095–1099, doi:10.1302/0301-620X.82B8.11744 [DOI] [PubMed]
- 12.Haraguchi K, Sugano N, Nishii T, Miki H, Oka K, Yoshikawa H (2001) Phase transformation of a zirconia ceramic head after total hip arthroplasty. J Bone Jt Surg Br 83:996–1000, doi:10.1302/0301-620X.83B7.12122 [DOI] [PubMed]
- 13.Hernigou P, Bahrami T (2003) Zirconia and alumina ceramics in comparison with stainless-steel heads: polyethylene wear after a minimum ten-year follow-up. J Bone Jt Surg Br 85:504–509, doi:10.1302/0301-620X.85B4.13397 [DOI] [PubMed]
- 14.Inoue A, Asaumi K, Endo H, Fujiwara K, Mitani S, Ozaki T (2006) Assessment of head wear more than ten years after total hip arthroplasty: 22-mm zirconia vs. metal heads. Acta Med Okayama 60:311–318 [DOI] [PubMed]
- 15.Kim YH (2005) Comparison of polyethylene wear associated with cobalt-chromium and zirconia heads after total hip replacement: a prospective, randomized study. J Bone Jt Surg Am 87:1769–1776, doi:10.2106/JBJS.D.02572 [DOI] [PubMed]
- 16.Kim YH, Kim JS, Cho SH (2001) A comparison of polyethylene wear in hips with cobalt-chrome or zirconia heads: a prospective, randomised study. J Bone Jt Surg Br 83:742–750, doi:10.1302/0301-620X.83B5.10941 [DOI] [PubMed]
- 17.Kraay MJ, Thomas RD, Rimnac CM, Fitzgerald SJ, Goldberg VM (2006) Zirconia versus Co-Cr femoral heads in total hip arthroplasty: early assessment of wear. Clin Orthop Relat Res 453:86–90, doi:10.1097/01.blo.0000246544.95316.1f [DOI] [PubMed]
- 18.Liang B, Kawanabe K, Ise K, Iida H, Nakamura T (2007) Polyethylene wear against alumina and zirconia heads in cemented total hip arthroplasty. J Arthroplasty 22:251–257, doi:10.1016/j.arth.2006.03.004 [DOI] [PubMed]
- 19.Maloney WJ, Galante JO, Anderson M et al (1999) Fixation, polyethylene wear, and pelvic osteolysis in primary total hip replacement. Clin Orthop Relat Res 369:157–164, doi:10.1097/00003086-199912000-00016 [DOI] [PubMed]
- 20.Martell JM, Berdia S (1997) Determination of polyethylene wear in total hip replacements with use of digital radiographs. J Bone Jt Surg Am 79:1635–1641 [DOI] [PubMed]
- 21.Masonis JL, Bourne RB, Ries MD, McCalden RW, Salehi A, Kelman DC (2004) Zirconia femoral head fractures: a clinical and retrieval analysis. J Arthroplasty 19:898–905, doi:10.1016/j.arth.2004.02.045 [DOI] [PubMed]
- 22.Orishimo KF, Claus AM, Sychterz CJ, Engh CA (2003) Relationship between polyethylene wear and osteolysis in hips with a second-generation porous-coated cementless cup after seven years of follow-up. J Bone Jt Surg Am 85:1095–1099 [DOI] [PubMed]
- 23.Santos EM, Vohra S, Catledge SA, McClenny MD, Lemons J, Moore KD (2004) Examination of surface and material properties of explanted zirconia femoral heads. J Arthroplasty 19(Suppl 2):30–34, doi:10.1016/j.arth.2004.06.017 [DOI] [PubMed]
- 24.Sochart DH (1999) Relationship of acetabular wear to osteolysis and loosening in total hip arthroplasty. Clin Orthop Relat Res 363:135–150, doi:10.1097/00003086-199906000-00018 [DOI] [PubMed]
- 25.Wroblewski BM, Fleming PA, Siney PD (1999) Charnley low-frictional torque arthroplasty of the hip: 20-to-30 year results. J Bone Jt Surg Br 81:427–430, doi:10.1302/0301-620X.81B3.9521 [DOI] [PubMed]
- 26.Wroblewski M, Siney PD, Nagai H, Fleming PA (2004) Wear of ultra-high-molecular-weight polyethylene cup articulating with 22.225 mm zirconia diameter head in cemented total hip arthroplasty. J Orthop Sci 9:253–255, doi:10.1007/s00776-004-0777-4 [DOI] [PubMed]
- 27.Yoshimura M, Noma T, Kawabata K, Somiya S (1987) Role of H2O on the degradation process of Y-TZP. J Mater Sci Lett 6:465–467, doi:10.1007/BF01756800 [DOI]
- 28.Zhou J, Mah J, Shrotriya P, Mercer C, Soboyejo WO (2007) Contact damage in an yttria stabilized zirconia: implications. J Mater Sci Mater Med 18:71–78, doi:10.1007/s10856-006-0664-y [DOI] [PubMed]