This paper describes a case of fatal rectus sheath hematoma (RSH) following administration of enoxaparin subcutaneously into the abdominal wall in an elderly patient taking warfarin. Physicians are increasingly using such low-molecular-weight heparins (LMWHs) to initiate anticoagulation for many clinical conditions, such as atrial fibrillation, unstable angina pectoris, non–Q-wave myocardial infarction, deep-vein thrombosis, and pulmonary emboli. Physicians also use LMWHs as prophylaxis following hip and knee replacement surgery. Low-molecular-weight heparins are at least as safe as unfractionated heparin (UFH) and can be administered by subcutaneous injection on an outpatient basis by a health care professional or, with appropriate training, by the patient, a family member, or another caregiver. The improved bioavailability and pharmacodynamic characteristics of LMWHs make outpatient therapy feasible. The LMWHs have changed the course of outpatient anticoagulation therapy because patients no longer need to remain hospitalized for initiation of oral therapy or for bridge therapy when undergoing invasive procedures that require temporary discontinuation of warfarin.1
Medical staff—family physicians, internists, and cardiologists—might encounter bleeding complications in patients using LMWH. The probable mechanisms underlying this scenario include possible accidental injection of enoxaparin intramuscularly as well as its pronounced anticoagulation effect in elderly patients and patients with increased bleeding tendency. When they encounter such bleeding in elderly and cachectic patients, medical staff should consider the site of LMWH injection because it is impossible to exclude the possibility that some patients might be injected intramuscularly in the outpatient setting. Thus, use of LMWH requires prudent application and deliberate follow-up in every case, as well as careful training for the patient or caregiver if he or she is to administer the injections. Owing to the risk of accidental intramuscular injection, we suggest that subcutaneous injection in the deltoid region might be safer if the injection is to be administered by the patient or by a caregiver who is not a physician.
Case description
A 76-year-old woman was admitted to hospital complaining of severe shortness of breath. She had been using furosemide and an angiotensin-converting enzyme inhibitor for the treatment of heart failure. Her blood pressure was 110/70 mm Hg. Her lips and mouth were reddish-blue, suggesting central cyanosis. She had serious pretibial edema. The physician felt a hyperdynamic jugular venous pulse at the left sternal border. Her heart sounds were dysrhythmic and tachycardic; a mild systolic murmur was heard at the apex. The physician observed an atrial fibrillation with rapid ventricular response in the electrocardiogram. A chest radiograph revealed cardiomegaly due to right atrial enlargement with prominent pulmonary vascular markings. In addition, an echocardiogram showed pulmonary hypertension and a patent foramen ovale. Ejection fraction was normal. A transesophageal echocardiogram was used for differential diagnosis.
Treatment was initiated with oral diltiazem (240 mg/d), intravenous diuretic, and nitroglycerin in addition to the enoxaparin (6000 IU twice daily, injected subcutaneously on the left side of the abdominal wall) and warfarin (5 mg/d). On the third day of her hospitalization, right heart catheterization was performed by insertion of a 6F Cournand catheter into the right femoral vein (without any punctures to her left side). The sheath was removed immediately. The patient described progressive abdominal pain 24 hours after insertion.
The patient’s abdomen appeared massively distended, and medical staff felt a mass in the left side of the abdomen (Figure 1). Emergent ultrasonograms revealed a heterogeneous lesion composed of cystic and solid components in the left lower quadrant of the abdomen extending from the inguinal region to the umbilicus. Computed tomography results showed a dense heterogeneous mass in the pelvic region and the left rectus abdominis muscle, suggesting hematoma and intraperitoneal bleeding (Figure 2). The patient had taken enoxaparin with 5 mg of warfarin daily for 3 days. Her hemoglobin level was 9 g/dL; her prothrombin time was 34.6 seconds (international normalized ratio [INR] 3.46). Anticoagulant treatment was discontinued, and the patient was given 2 units of fresh-frozen plasma and 8 units of erythrocyte suspension.
Figure 1.

The patient with ecchymosis in the abdominal wall and left flank
Figure 2.
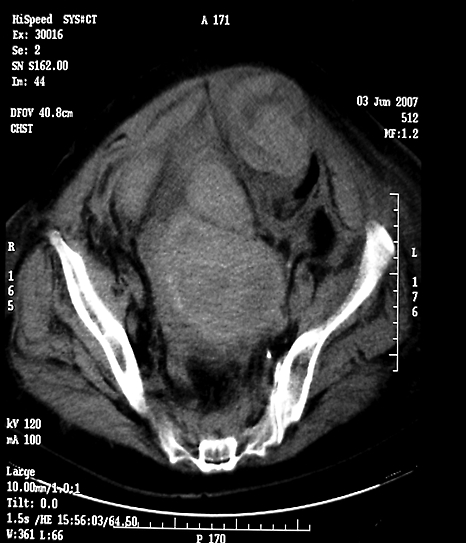
Computed tomography scan of the patient showing the hematoma limited in the left rectus abdominis sheath
A general surgery clinic was consulted and an operative procedure was recommended. The patient and her relatives decided against the operation. In the following days, her abdominal distention persisted. Her serum urea and creatinine levels progressively increased. Medical staff detected metabolic acidosis in blood gas analysis. Her urine output decreased, and she experienced difficulty breathing. She developed acute renal insufficiency and metabolic acidosis. She subsequently died despite vigorous supportive care.
Discussion
Rectus sheath hematoma is an uncommon but serious bleeding complication associated with anticoagulant and antiaggregant therapies. Hemorrhage within the rectus sheath can occur in a variety of conditions.2 It can develop owing to direct damage to the muscle itself or tearing in one of the superior or inferior epigastric vessels that run along its posterior aspect.
Different forms of heparin are widely used for many clinical conditions. Enoxaparin is a reasonable alternative to UFH owing to its favourable side-effect profile, ease of administration, and diminished need for laboratory monitoring. In most clinical circumstances, the risk of bleeding associated with the use of enoxaparin appears to be comparable to that of UFH.
We systematically searched MEDLINE (1966 to January 2008) and EMBASE (1974 to January 2008) using MeSH terms and text words including enoxaparin, heparin, hematoma, and rectus abdominis. Some of the articles found in the searches mentioned abdominal wall hematomas due to enoxaparin.3–11 Holmes et al reported a case of RSH as a cause of acute abdominal pain during treatment with enoxaparin.3 Aortoiliac and pelvic arteriography have shown needle puncture of the inferior epigastric artery might contribute to the occurrence of RSH. Bleeding was controlled through coil embolization of the inferior epigastric artery. Ortega-Carnicer and Ceres presented the case of a previously healthy patient who developed an RSH shortly after administration of enoxaparin, owing to unstable angina, and underwent urgent laparotomy.4
Concomitant use of drugs that also impair hemostasis (eg, antiplatelet agents) in elderly patients could increase risk of RSH. Adeonigbagbe et al presented the case of a 95-year-old patient who developed spontaneous RSH and an anterior pelvic hematoma while taking subcutaneous enoxaparin and warfarin for deep-vein thrombosis.5 The patient’s INR was 5.09 at the time of diagnosis. Davutoglu et al described a fatal secondary abdominal compartment syndrome that occurred after severe RSH with intraperitoneal bleeding in a younger patient who had taken warfarin and enoxaparin for thromboprophylaxis of prosthetic heart valves.6 Rectus sheath hematoma has also been described in a patient with acute coronary syndrome who was taking clopidogrel, aspirin, and LMWH.7
Cherry and Mueller reviewed the largest series of patients with RSH at the Mayo Clinic during a 10-year period.8 Of the 126 patients, 64% were female; the median age was 73 years. Most patients (69%) were prescribed some form of anticoagulation therapy. Nearly 25% were receiving anticoagulation and antiplatelet therapy simultaneously. It is unclear, however, whether those patients were at greater risk of RSH compared with patients receiving either anticoagulation or antiplatelet therapy alone.
In the case of the patient presented above, it seems that accidental intramuscular enoxaparin injection was predominantly responsible for hematoma formation, and warfarin use with high INR levels might have contributed to the extension of the hematoma.
In the randomized controlled trials in which warfarin and LMWH were coadministered, TIMI (Thrombolysis in Myocardial Infarction) or GUSTO (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) bleeding classifications were used to define severity. According to these classifications, retroperitoneal hematoma and RSH are considered to be major bleeding. Therefore, we do not know the prevalence of RSH in large registries and trials of anticoagulated patients. Overall mortality of those with RSH is reported to be 4%, but it dramatically increases to 25% among anticoagulated patients.9 Although it can be treated conservatively,10 surgical intervention is recommended in patients with large hematomas with hemodynamic instability.11 Endovascular embolization of suspect vessels is a suitable alternative to surgical management in cases in which the hematoma continues to expand.3
Conclusion
Family physicians are increasingly using enoxaparin to initiate anticoagulation for many clinical conditions in the outpatient setting. Enoxaparin is usually administered by a health care professional, by the patient, or by a family member trained in how to give the injections. The administration technique and injection sites could be puzzling for unpractised people who are obliged to use enoxaparin in the outpatient setting. We suggest that subcutaneous injections from the abdominal wall might increase the risk of hematoma, especially in elderly and thin patients with less abdominal fat. Health care professionals (such as family physicians) and patients and their relatives using enoxaparin might be well advised to avoid deep injections into the abdomen. Subcutaneous injections in the deltoid region could be safer.12
The importance of close monitoring of the INR to prevent hemorrhagic complications should also be emphasized. The INR can increase quickly, independent of dosage in elderly patients taking anticoagulants. In such cases, heparin treatment should be discontinued as soon as the desired INR levels are achieved.
EDITOR’S KEY POINTS.
Rectus sheath hematoma is an uncommon but serious complication of anticoagulation and antiplatelet therapies. It can occur as a consequence of damage to the muscle directly or to the blood vessels.
This case report describes a fatal rectus sheath hematoma in an elderly woman that occurred following injections of enoxaparin abdominally, in conjunction with warfarin use.
The authors caution that in thin or elderly patients, or in those on concomitant anticoagulation or antiplatelet agents, the deltoid region might be a safer injection site for low-molecular-weight heparins.
POINTS DE REPÈRE DU RÉDACTEUR.
L’hématome à la paroi du grand droit est une complication rare mais grave des thérapies anticoagulantes et antiplaquettaires. Il peut se produire à la suite d’un dommage direct au muscle ou aux vaisseaux sanguins.
Cette étude de cas décrit un hématome fatal à la paroi du grand droit chez une femme âgée qui s’est produit après des injections abdominales d’énoxaparine combinées à l’utilisation de warfarin.
Les auteurs font la mise en garde suivante: chez les patients minces ou plus âgés ou ceux qui utilisent concurremment des agents anticoagulants ou antiplaquettaires, la région deltoïdienne est un site d’injection plus sécuritaire pour les héparines de bas poids moléculaire.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Competing interests
None declared
References
- 1.Du Breuil AL, Umland EM. Outpatient management of anticoagulation therapy. Am Fam Physician. 2007;75(7):1031–42. [PubMed] [Google Scholar]
- 2.Miyauchi T, Ishikawa M, Miki H. Rectus sheath hematoma in an elderly woman under anti-coagulant therapy. J Med Invest. 2001;48(3–4):216–20. [PubMed] [Google Scholar]
- 3.Holmes SJ, Yale SH, Mazza JJ. Rectus sheath hematoma as a cause of acute abdominal pain. Am Fam Physician. 2001;64(10):1681–2. [PubMed] [Google Scholar]
- 4.Ortega-Carnicer J, Ceres F. Rectus sheath haematoma with severe haemodynamic compromise after enoxaparin use for unstable angina. Resuscitation. 2003;57(1):113–4. doi: 10.1016/s0300-9572(02)00431-8. [DOI] [PubMed] [Google Scholar]
- 5.Adeonigbagbe O, Khademi A, Karowe M, Gualtieri N, Robilotti J. Spontaneous rectus sheath hematoma and an anterior pelvic hematoma as a complication of anticoagulation. Am J Gastroenterol. 2000;95(1):314–5. doi: 10.1111/j.1572-0241.2000.01718.x. [DOI] [PubMed] [Google Scholar]
- 6.Davutoglu V, Kervancioglu S, Sezen Y. Large rectus muscle hematoma with intraperitoneal bleeding and fatal abdominal compartment syndrome complicating anticoagulant therapy. Clin Appl Thromb Hemost. 2005;11(1):109–11. doi: 10.1177/107602960501100115. [DOI] [PubMed] [Google Scholar]
- 7.Tuncer C, Sökmen G, Güven A, KöleoIlu M, Oncel H, Süner A. [A patient with an acute coronary syndrome and abdominal rectus sheath haematoma mimicking acute abdomen. ] Anadolu Kardiyol Derg. 2004;4(4):372–3. [Turkish] [PubMed] [Google Scholar]
- 8.Cherry WB, Mueller PS. Rectus sheath hematoma. Review of 126 cases at a single institution. Medicine (Baltimore) 2006;85(2):105–10. doi: 10.1097/01.md.0000216818.13067.5a. [DOI] [PubMed] [Google Scholar]
- 9.Werdehoff SG, Blomkalns AL. Rectus sheath hematoma. Omaha, NE: eMedicine, WebMD; 2005. [Google Scholar]
- 10.Berná J, Zuazu I, Madrigal M, García-Medina V, Fernández Guirado F. Conservative treatment of large rectus sheath hematoma in patients undergoing anticoagulant therapy. Abdom Imaging. 2000;25(3):230–4. doi: 10.1007/s002610000007. [DOI] [PubMed] [Google Scholar]
- 11.Biffl WL, Moore EE, Burch JM, Offner PJ, Franciose RJ, Johnson JL. Secondary abdominal compartment syndrome is a highly lethal event. Am J Surg. 2001;182(6):645–8. doi: 10.1016/s0002-9610(01)00814-5. [DOI] [PubMed] [Google Scholar]
- 12.Crooke B, Callaway LK. Fatal haemorrhage associated with enoxaparin. Intern Med J. 2007;37(3):207–8. doi: 10.1111/j.1445-5994.2006.01288.x. [DOI] [PubMed] [Google Scholar]


