Abstract
In this depression prevention trial, 341 high-risk adolescents (M age = 15.6, SD = 1.2) with elevated depressive symptoms were randomized to a brief group cognitive-behavioral (CB) intervention, group supportive-expressive intervention, bibliotherapy, or assessment-only control condition. CB participants showed significantly greater reductions in depressive symptoms than supportive-expressive, bibliotherapy, and assessment-only participants at posttest, though only the latter effect was significant at 6-month follow-up. CB participants showed significantly greater improvements in social adjustment and reductions in substance use at posttest and 6-month follow-up than participants in all three other conditions. Supportive-expressive and bibliotherapy participants showed greater reductions in depressive symptoms than assessment-only controls at certain follow-up assessments, but produced no effects for social adjustment and substance use. CB, supportive-expressive, and bibliotherapy participants showed a significantly lower risk for major depression onset over the 6-month follow-up than assessment-only controls. The evidence that this brief CB intervention reduced risk for future depression onset and outperformed alternative interventions for certain ecologically important outcomes suggests that this intervention may have clinical utility.
Keywords: depression, prevention, high-risk, adolescent, alternative interventions
Major depression in adolescents is a common, recurrent, and impairing condition that predicts future suicide attempts, academic failure, interpersonal problems, unemployment, substance abuse, and delinquency (Klein, Torpey, & Bufferd, 2008). Because less than one third of depressed youth receive treatment (Newman et al., 1996) it is crucial to develop prevention programs for this pernicious condition.
Most depression prevention programs focus on reducing negative cognitions because a negative view towards oneself, one’s experiences, and the future and a negative schema that biases the selection, encoding, and evaluation of information, theoretically increase risk for onset and persistence of depression (Beck, 1976). Negative cognitions predict future increases in depression among adolescents (Hankin, Abramson, & Siler, 2001; Lewinsohn et al., 1994; Nolen-Hoeksema, Girgus, & Seligman, 1992) and treatments targeting negative cognitions reduce depression (Brent et al., 1997; Reynolds & Coats, 1986; Rohde, Clarke, Mace, Jorgensen, & Seeley, 2004). Certain programs have also encouraged increased frequency of pleasant activities (Stice, Burton, Bearman, & Rohde, 2006), based on the behavioral theory of depression that posits that negative moods prompt a withdrawal from pleasant activities that exacerbates depressed mood (Lewinsohn, Youngren, & Grosscup, 1979). Low rates of pleasant activities predict future depressive symptoms during adolescence (Clarke et al., 1992) and behavioral activation treatments effectively decrease depression in adults (Jacobson et al., 1996). Other programs enhance protective factors, such as problem solving and social skills, based on evidence that depressed youth often exhibit deficiencies in these areas (Gillham et al., 2006b; Young, Mufson, & Davies, 2006). Theoretically, these deficits increase risk for onset and persistence of major depression because they lead to an erosion of social support and increase risk for negative life events and interpersonal problems. Deficits in problem solving and social skills increase risk for future onset and persistence of depression (Lewinsohn et al., 1994; Warner, Weissman, Fendrich, Wickramaratne, & Moreau, 1992).
Cognitive-behavioral (CB) interventions that focus on negative cognitions and pleasant activities have the largest evidence-base. CB interventions have produced significantly greater reductions in depressive symptoms than assessment-only control groups in both universal trials (Jaycox, Reivich, Gillham, & Seligman, 1994; Shochet et al., 2001; Spence, Sheffield, & Donovan, 2003) and selected trials involving youth at high-risk for depression (Burton, Stice, Bearman, & Rohde, 2007; Clarke et al., 1995, 2001; Seligman, Schulman, & Tryon, 2007). For instance, Clarke et al. (1995) found that a 15-session group CB intervention resulted in greater reductions in depressive symptoms by posttest than an assessment-only control condition for adolescents with depressive symptoms, though this effect was nonsignificant at 12-month follow-up. CB interventions have significantly reduced risk for future onset of major depression in some trials (Clarke et al., 1995; 2001), but not others (Gillham, Hamilton, Freres, Patton & Gallop, 2006a; Seligman, Schulman, DeRubeis, & Hollon 1999; Seligman et al., 2007; Sheffield et al., 2006). However, meta-analytic reviews indicate that the average effects from depression prevention trials are typically small and that the effects for universal programs are significantly smaller than those for selected programs (Horowitz & Garber, 2006; Stice, Shaw, Bohon, Marti, & Rohde, 2008). For instance, the average pre to post effect for selected programs was d = .30, compared to an average effect of d = .12 for universal programs (Horowitz & Garber, 2006).
Although CB prevention programs produce promising findings, the long duration of these interventions makes them challenging to implement. Thus, we developed a brief 4-session CB prevention program that focused on reducing negative cognitions and increasing pleasant activities, and evaluated it in preliminary trial involving high-risk adolescents with depressive symptoms (Stice et al., 2006). CB intervention participants showed significantly greater reductions in depressive symptoms than assessment-only controls at posttest and 1-month follow-up, but not at 6-month follow-up. The fact that the effects became nonsignificant by 6-month follow-up prompted us to expand the program into the 6-session intervention that was evaluated in the present trial. Thus, the first aim is to compare this brief 6-session CB depression prevention trial to an assessment-only control condition.
A second gap in the literature is that few trials have compared CB programs to placebo or alternative interventions. This is important because without such comparison conditions it is impossible to know whether effects resulted because of the specific therapeutic procedures theorized to produce intervention effects, nonspecific effects common to all psychosocial interventions (e.g., therapeutic alliance, group cohesion, installation of hope), or design artifacts (e.g., participant expectancies, demand characteristics). It is necessary to show that an intervention outperforms a placebo or alternative intervention to establish that it is efficacious (American Psychiatric Association, 1995). Only three trials have compared CB prevention programs to alternative interventions. Merry, McDowell, Wild, Bir, and Cunliffe (2004) found that a universal CB depression prevention program with an interpersonal focus produced significantly greater reductions in depressive symptoms at posttest than an arts and crafts intervention, though effects faded over 18-month follow-up. However, results are difficult to interpret because there was no assessment-only control condition to which to compare the two interventions and it seems unlikely that an arts and crafts class would be perceived as a credible intervention for depression. Stice et al. (2006) compared a CB intervention to supportive-expressive group therapy, bibliotherapy, expressive writing, and journaling interventions. Participants in all intervention conditions showed significantly greater reductions in depressive symptoms than assessment-only controls at posttest, but only CB and bibliotherapy produced intervention effects that persisted into follow-up. CB participants showed significantly greater reductions in depressive symptoms relative to only one of the four alternative interventions (journaling). Additionally, CB bibliotherapy participants showed significantly greater reductions in symptoms than expressive writing participants at 6-month follow-up. Results imply that nonspecific factors and design artifacts contribute to the apparent CB intervention effects or that there are multiple methods of reducing depressive symptoms. Yet, it is difficult to draw conclusions from this trial because the cell sizes were small and diagnostic interviews were not used, making it impossible to test whether this CB intervention reduced risk for future major depression onset relative to the other conditions. Gillham et al. (2007) found that a CB depression prevention program did not produce significantly greater reductions in depressive symptoms than a non-specific comparison intervention or an assessment-only control condition. These findings are puzzling because the CB prevention program has produced effects in previous trials (e.g., Jaycox et al., 1994), suggesting that the use of school counselors and teachers to deliver the program may have compromised fidelity and attenuated effects. Thus, the second aim was to conduct a more rigorous comparison of the CB intervention to a supportive-expressive group intervention and a CB bibliotherapy intervention.
We selected two alternative interventions that varied along the dimensions theorized to contribute to therapeutic effects. Because we wanted to examine an active intervention that possessed all of the nonspecific factors of a psychosocial group intervention, but no CB content, we included a supportive-expressive group therapy condition. Because we wanted to examine an intervention that included the content of CB interventions, but without the nonspecific factors, we included a CB bibliotherapy condition. The goals of non-directive supportive-expressive interventions, which have been used in prior treatment trials (Brent et al., 1997; Shaw, 1977), are to establish and maintain rapport, provide support, and help the client identify and express emotions. Kolko, Brent, Baugher, Bridge, and Birmaher (2000) found that depression remission rates were significantly greater for CB treatment than non-directive supportive-expressive psychotherapy at posttest, though this effect did not persist through 2-year follow-up. Bibliotherapy, or the prescription of books for the treatment of a disorder, is an inexpensive and accessible medium for intervention delivery. CB bibliotherapy has outperformed assessment-only control conditions for the treatment of depression for adolescents and adults (Cuijpers, 1997; Gregory, Schwer-Canning, Lee, & Wise, 2004). Ackerson, Scogin, McKendree-Smith, and Lyman (1998) found that CB bibliotherapy was superior to an assessment-only control condition for adolescents with moderate depressive symptoms through 1-month follow-up. We thought it particularly vital to compare the apparent intervention of choice for the prevention of depression (CB) to bibliotherapy because the latter is less expensive and easier to disseminate.
Finally, it is vital to demonstrate that interventions impact ecologically valid outcomes. Thus, the third aim was to test whether the CB intervention improves social adjustment in school, peer, and family domains and reduces psychiatric problems that may represent counter-productive attempts to regulate negative affect: binge eating and substance use (Cooper, Frone, Russell, & Mudar, 1995; McCarthy, 1990).
In sum, the first aim was to compare the effectiveness of a brief group CB depression prevention program for high-risk youth to an assessment-only control condition. The second aim was to compare this CB program to two active control conditions that provided selected aspects of the CB group: CB skills in bibliotherapy and nonspecific factors in supportive-expressive group treatment. The third aim was to test whether the CB program produced significantly stronger improvements in social adjustment and reductions in binge eating and substance use. We targeted adolescents with depressive symptoms because meta-analytic reviews indicated that selected programs targeting high-risk youth produce larger effects than universal programs that are offered to all adolescents (Horowitz & Garber, 2006; Stice, Shaw et al., 2008). Participants who are struggling with subdiagnostic depression may be more likely to engage in the prevention program because they are more motivated to change. It may also be easier to acquire intervention skills when they can be applied to current psychiatric symptoms. We focused on adolescents with depressive symptoms because risk factor studies have found that this is typically the most potent predictor of future onset of major depression (Lewinsohn et al., 1994; Stice, Hayward, Cameron, Killen, & Taylor, 2000; Weissman et al., 1992) and this population has responded to CB prevention programs (Clarke et al., 1995, 2001).
Methods
Participants
Participants were 341 high school students (56% female) who ranged in age from 14 to 19 years (M = 15.6; SD = 1.2) at pretest. The sample was composed of 2% Asians, 9% African Americans, 46% Caucasians, 33% Hispanics, and 10% who specified other or mixed heritage. Educational attainment of parents, a proxy for socioeconomic status, was 26% high school graduate or less; 17% some college; 35% college graduate; 18% graduate degree. The sample was fairly representative of the populations from which we sampled in terms of ethnicity (7% African American, 18% Hispanic, 65% Caucasian), and parental education (34% high school graduate or less; 25% some college; 26% college graduate; 15% graduate degree). Twenty-eight percent of the sample had received treatment services for emotional/behavioral problems during the 12-month period preceding the study.
Procedures
Participants were recruited using mass mailings, handbills distributed during the lunch hour, and posters that invited students experiencing sadness to participate in a trial of interventions designed to improve current and future mood. Interested students (6–10% across schools) were given a depressive symptom screen (the Center for Epidemiologic Studies-Depression scale [CES-D; Radloff, 1977]) and a consent form for them and their parents to sign. Those who returned a signed consent form and scored 20 or above on the CESD were invited to complete a pretest (baseline) assessment. The cut-point for inclusion was based on research using the CES-D as screening tools for adolescent depressive disorders (Roberts, Lewinsohn, & Seeley, 1991). Those who met criteria for current major depression upon interview were excluded and given treatment referrals (there were no other exclusion criteria). All participants were provided with treatment referral information and encouraged to seek treatment if their depressive symptoms worsened during the study. If a participant endorsed suicidal ideation on the interview, project staff called the student and parent to contract for safety, reiterate the importance of seeking treatment, and provide additional referral information. An emergency response plan for suicide attempts was prepared, but was not needed.
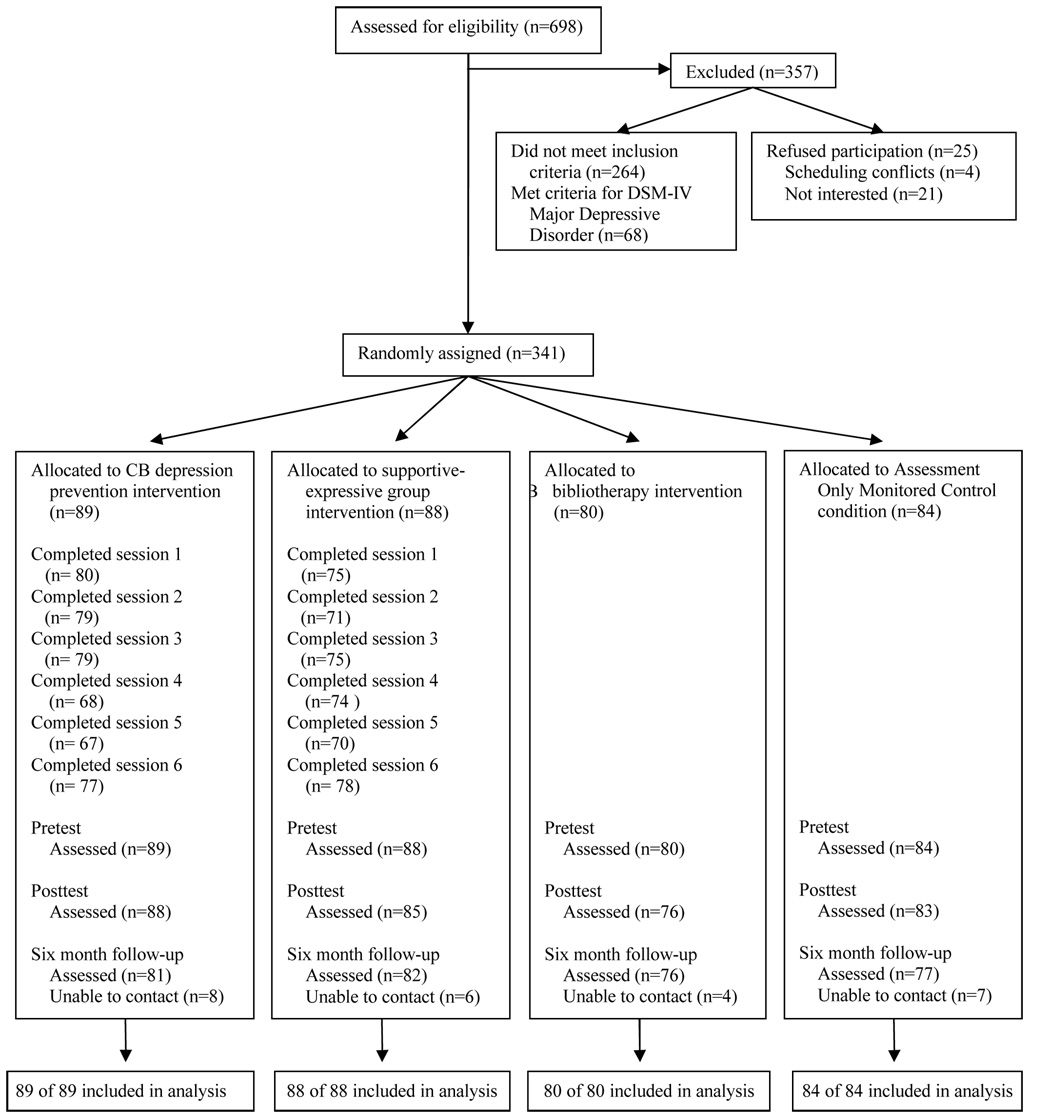
Participants were recruited at six schools (40–75 students per school) between 2004 and 2007. Eligible participants were randomly assigned, within blocks created by gender and school, by the project coordinator using computer-generated random numbers to one of four conditions: (1) CB group (n = 89), (2) supportive-expressive group (n = 88), (3) bibliotherapy (n = 80), or (4) assessment-only control (n = 84). CB and supportive-expressive group interventions consisted of six weekly 1-hour sessions facilitated by a clinical graduate student and co-facilitated by an undergraduate; groups contained 6–10 participants. A total of 13 facilitators (10 women, 3 men) conducted the inventions (5 conducted CB groups only, 3 conducted supportive-expressive groups only, 5 conducted both). Facilitators were assigned to condition on the basis of time availability, training experience, treatment preference, and gender. If a participant missed a session, a brief (10–15 minute) individual session was conducted with the youth to review missed material when possible. Detailed manuals were used for the two group interventions, containing verbatim scripts and solutions to common problems.
Participants completed a survey and diagnostic interview at pretest, posttest, and 6-month follow-up. They were paid $20 for completing each assessment. Assessors, who were blinded to condition, had at least a BA in psychology and received 40 hours of training in the use of the semi-structured interviews, which involved didactic presentations on diagnostic criteria and interview skills, practice ratings of pre-recorded interviews, and interview role-plays. Assessors were required to show a minimum kappa agreement of .80 with expert raters before starting data collection and to maintain this throughout the study (assessed in a randomly selected 10% of taped interviews). Assessments and groups were conducted at schools. The local Institutional Review Board approved this study.
Facilitator Training and Supervision
Facilitators and co-facilitators first read the published efficacy trials to introduce them to the major concepts involved in the CB depression prevention program and then read the CB and supportive-expressive intervention scripts. Next, they attended a 2-day training workshop conducted by Dr. Rohde in which they reviewed the components of each session and role-played the challenging aspects of the programs. The crisis response plan was then reviewed. During the groups, Dr. Rohde conducted separate weekly supervision meetings with the CB and supportive-expressive facilitators to provide corrective feedback. Prior to the meetings, facilitators provided a written summary of each session. Drs. Rohde and Stice were available in the event of any worsening of depressive symptoms, suicidal ideation, or other psychiatric crisis.
Dr. Rohde rated recordings of the sessions for adherence and competence using scales adapted from prior trials (Rohde et al., 2004). Two sessions from the first group for each facilitator and one from each subsequent group were randomly selected for ratings (a total of 23 CB sessions and 20 supportive-expressive were rated [27% total]). Adherence was measured using session-specific checklists for the concepts, skills, and exercises detailed in the scripts. Each item was rated for full, partial, or minimal presentation. General facilitator competence was rated using 18 3-point items that assessed the various indicators of a competent therapist (e.g., leader fosters supportive group process, allocates time fairly across group members). These scales have shown inter-rater reliability in previous research (M ICC = .72). Facilitators received written and verbal supervision based on the tape review.
CB Depression Prevention Intervention
In the design of our brief CB program we drew upon the Clarke et al. (1995) program, general CB concepts for the prevention and treatment of depression, and our experience with the design of eating disorder prevention programs. Didactic presentation was minimized because psychoeducational interventions are less effective than interventions that actively engage participants (Stice & Shaw, 2004). The 6 weekly 1-hour sessions focused on building group rapport, increasing participant involvement in pleasant activities, and replacing negative cognitions with positive cognitions. In-session exercises were used that require youth to apply the skills taught in the intervention. We used homework to reinforce the skills taught in the sessions and help participants learn how to apply these skills to their daily life. We also used motivational enhancement exercises to maximize willingness to use the new skills, strategic self-presentation to facilitate internalization of key principles, behavioral techniques to reinforce use of the new skills, and group activities to foster feelings of social support and group cohesion.
Supportive-Expressive Group Intervention
Based on non-directive supportive psychotherapy (Brent et al., 1997), the goals of this condition were to establish and maintain rapport, provide support, and help participants identify and express feelings; this group did not cover any specific skills from the other conditions. The 6 weekly 1-hour sessions provided a forum to discuss feelings in a safe environment based on the rationale that (a) sharing our inner feelings with another person reduces stress and improves our mood, (b) listening to others helps us realize we are not alone, and (c) it’s more helpful to listen than tell others what to do. The core of the sessions was devoted to open sharing, providing participants with a venue to discuss and process their emotional experiences since the previous meeting. Participants were encouraged to discuss changes in their experiences, as well as any emerging problems or worries. No direct advice was given, but participants and facilitators actively supported and responded to one another. All sessions concluded with a summary statement by the facilitators that focused on common themes the emerged in the session.
Bibliotherapy Intervention
Participants in the bibliotherapy condition were given copies of Feeling Good (Burns, 1980). It provides relevant and practical CB techniques for preventing and reducing negative moods and is considered to be an effective self-help book for the treatment and prevention of depression. It is written at a high-school reading level. Topics covered include understanding feelings of sadness, building self-esteem, overcoming feelings of guilt and helplessness, and coping with stress and daily hassles. Participants were told, “This book has been shown to be helpful to some individuals who are feeling sad or depressed. This copy is yours to keep, so feel free to write or highlight in it as you read. We encourage you to use this as a self-help resource.”
Assessment-Only Control Condition
At pretest, participants were given an NIMH brochure that describes major depression and recommends treatment for depressed youth ("Let’s Talk About Depression" NIH Pub. 01-4162), as well as information about local treatment options. They completed the same assessments as those in the other conditions, which allowed us to monitor depression and suicidal ideation, and to contact parents and provide treatment referrals as necessary (as was done in all conditions). Participants and their parents were also asked to contact research staff if they believe that the adolescent’s depression had worsened. We selected this control group because it represents an ecologically valid control condition of what is generally provided to youth in the local schools.
Measures
Depressive symptoms and diagnosis
Sixteen items assessing DSM-IV major depression symptoms were adapted from the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS; Puig-Antich & Chambers, 1983), a semi-structured diagnostic interview. Participants reported the peak severity of each symptom over their lifetime or since the last interview using an expanded response format (response options: 1 = not at all to 4 = severe symptoms [ratings of 3 and 4 reflecting diagnostic levels]). Severity ratings for each symptom were averaged to form a continuous depressive symptom composite. Responses were also used to determine whether participants met diagnostic criteria for major depression since the last assessment. This adapted version of the K-SADS has shown test-retest reliability (k = .63 – 1.00), inter-rater reliability for depression diagnosis (k = .73 – 1.00), internal consistency (α = .68 – .84), and predictive validity (Nolen-Hoeksema, Stice, Wade, & Bohon, 2007).
We also included the 21-item Beck Depression Inventory (BDI, Beck, Steer, & Garbin, 1988) to allow more direct comparisons to results from previous depression prevention trials. For each item, participants select among four alternative responses reflecting the increasing levels of symptom severity (0 = no symptom present to 3 = severe symptom present). The BDI has acceptable internal consistency (α = .73 to .95), test-retest reliability (r = .60 to .90), and convergent validity with clinician ratings of depressive symptoms (M r = .75; Beck et al., 1988). Although we report results for the BDI, we focus on the interviewer-rated depressive symptoms in the results and discussion sections because we have more confidence in interview-rated data (labeled depressive symptoms throughout).
Social adjustment
We used 17 items adapted from Social Adjustment Scale-Self Report for Youth (Weissman, Orvaschel, & Padian, 1980) to assess social adjustment in school, peer, spare time, and family domains (response options: 1 = never to 5 = always). The 17-item version has shown internal consistency (α = .77), 1-week test-retest reliability (r = .83) and sensitivity to treatment (Stice, Marti et al., 2008).
Substance use
Substance use was measured with 10 items from Stice, Barrera, and Chassin, (1998). Adolescents reported the frequency of intake during the past 6 months of beer/wine/wine coolers and hard liquor, frequency of heavy drinking (5 or more drinks in a row), frequency of times drunk, and frequency of marijuana, stimulants, downers, inhalants, and hallucinogen use. Items used 6-point response scales ranging from never to 3–7 times a week. Items were averaged to form an overall substance use measure, which was normalized with an inverse transformation. This scale has shown internal consistency (r = .87), 1-year test-retest reliability, and predictive validity for substance abuse symptoms (r = .72; Stice et al., 1998).
Bulimic pathology
The Eating Disorder Diagnostic Interview (Stice, Marti et al., 2008) assessed DSM-IV symptoms of bulimia nervosa. Items assessing frequency of binge eating and compensatory behavior (including vomiting, laxative/diuretic use, fasting, and excessive exercise) over the past month were summed to create an overall index of the behavioral symptoms of this disorder at each assessment. This composite was normalized with an inverse transformation. The symptom composite has shown internal consistency (α = .92), 1-week test-retest reliability (r = .90), sensitivity to detecting intervention effects, and predictive validity for future onset of depression (Stice, Marti et al., 2008).
Treatment variables
To compare the perceived credibility of the conditions, 4-items were administered prior to randomization assessing the expected benefit of, and preference for, CB group, supportive-expressive group, and bibliotherapy interventions. At posttest, participants rated their satisfaction with their intervention condition and the degree to which they felt prepared to avoid future depression using 5-point scales. Those assigned to bibliotherapy completed a 3-items at posttest to track how much of the book they had read, when they read it (e.g., right away, when bored, when upset, never) and future plans to use the book.
Results
Preliminary Analysis
Participants assigned to the four conditions did not differ on demographic factors, treatment services received for emotional/behavior problems during the past year, or baseline versions of the outcomes, with the exception of baseline depressive symptoms (F [3,334] = 4.80; p = .003; η2 = .04) (Table 1 reports means for outcomes across conditions and assessments). Thus, the baseline depressive symptom composite was used as a covariate in all outcome analyses. Mean scores for the treatment expectancy were similar across the three intervention conditions: CB 2.3 (SD = 0.8), supportive-expressive 2.6 (SD = 0.7), and bibliotherapy 2.4 (SD = 0.8), suggesting similar expected benefits from the interventions.
Table 1.
Descriptive Statistics by Treatment Condition for Study Outcome Measures
| CB N = 89 |
Supportive N = 88 |
Bibliotherapy N = 80 |
Control N = 84 |
|||||
|---|---|---|---|---|---|---|---|---|
| Outcome Measures | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Depressive symptoms | ||||||||
| T1 | 1.87 | 0.35 | 1.84 | 0.37 | 1.68 | 0.31 | 1.80 | 0.30 |
| T2 | 1.53 | 0.33 | 1.62 | 0.33 | 1.60 | 0.35 | 1.70 | 0.36 |
| T3 | 1.53 | 0.43 | 1.56 | 0.42 | 1.44 | 0.38 | 1.70 | 0.44 |
| Beck Depression Inventory | ||||||||
| T1 | 20.03 | 10.35 | 20.27 | 9.83 | 18.20 | 7.53 | 19.60 | 9.23 |
| T2 | 10.77 | 9.04 | 14.67 | 10.62 | 14.25 | 8.98 | 16.71 | 9.74 |
| T3 | 12.18 | 9.56 | 13.10 | 10.25 | 15.73 | 10.36 | 17.22 | 10.93 |
| Social adjustment | ||||||||
| T1 | 2.80 | 0.49 | 2.74 | 0.49 | 2.73 | 0.52 | 2.73 | 0.52 |
| T3 | 2.52 | 0.49 | 2.63 | 0.55 | 2.66 | 0.46 | 2.69 | 0.50 |
| Substance use frequency | ||||||||
| T1 | 0.47 | 0.54 | 0.61 | 0.77 | 0.59 | 0.71 | 0.39 | 0.60 |
| T2 | 0.41 | 0.58 | 0.63 | 0.87 | 0.63 | 0.78 | 0.40 | 0.57 |
| T3 | 0.42 | 0.65 | 0.67 | 0.87 | 0.72 | 0.97 | 0.59 | 0.81 |
| Bulimic symptom frequency | ||||||||
| T1 | 3.27 | 6.47 | 4.90 | 9.63 | 3.40 | 7.23 | 4.41 | 10.02 |
| T2 | 3.45 | 7.93 | 2.55 | 7.12 | 1.96 | 4.47 | 2.80 | 6.98 |
| T3 | 1.44 | 4.89 | 1.78 | 6.12 | 1.95 | 4.94 | 2.04 | 7.81 |
Note. CB = Cognitive-behavioral therapy; SD = standard deviation.
Attendance was similar across groups, 44% of CB participants attended all 6 sessions compared to 45% of supportive-expressive participants; 86% percent of CB participants and 89% of supportive-expressive participants attended at least 3 of the 6 sessions. Seven percent of the CB participants completed all 5 homework assignments, 20% completed 3–4 assignments, 25% completed 1–2 assignments, and 48% completed none. Among bibliotherapy participants, 28% indicated they read at least half the book, 44% read less than a quarter, and 28% did not read any. Of those who read at least part of the book 26% indicated they read the book when depressed, 62% when bored, and 12% immediately after receiving the book. Seventy-six percent of the CB condition indicated they were pleased or extremely pleased with the intervention compared to 71% of the supportive-expressive condition, and 29% of the bibliotherapy condition. Eight-four percent of the CB participants indicated they felt prepared to avoid future depression compared to 63% of the supportive-expressive participants, 64% of the bibliotherapy participants, and 44% of the control participants.
With regard to fidelity, 96% of the CB components and 100% of the supportive-expressive components were rated as full adherence. With regard to therapist competence, 94% of the items in the CB sessions were rated at good competence (5% at partial and 1% at poor) and 94% of the items in the supportive-expressive sessions were rated at good competence (6% at partial, 0% at poor). Participant ratings of therapist competence on a 5-point scale were similar for the CB group (4.6, SD = 0.7) and the supportive-expressive group (4.5, SD = 0.8). No instances of crossover (i.e., use of skills from the alternate intervention) were identified in the taped sessions.
A subset of 64 participants (20 at 6-month follow-up; 44 at 1-year follow-up) answered questions about cross-condition contamination. Most did not remember the other conditions (84%) and had not talked with anyone from the other conditions (88%). Of the 10 who reported knowing the other conditions, responses were vague (e.g., “I don’t know what they did but I know they met and talked”) or incorrect (e.g., “One got individual counseling”). No participant correctly identified all conditions. Of the 8 participants who had talked with a participant in another condition, responses were vague and referred to only one alternate condition (e.g., “He said they just talked”). No participant stated that hearing about the other groups or talking with other participants had changed their behaviors.
Three percent of participants did not provide data at posttest and 9% did not provide data at 6-month follow-up. Attrition did not differ significantly across the four conditions (χ2 [3, N = 338] = 0.95, p = .81); attrition was 11% in the CB and 8% for all three other conditions. Attrition was not related to any pretest variables. We employed an intent-to-treat analysis by using maximum-likelihood estimates to impute missing data with the SPSS Missing Value Analysis module, as it produces more accurate and efficient parameter estimates than list-wise deletion or last-observation-carried-forward (Schafer & Graham, 2002).
Intervention Effects for Primary Outcomes
Omnibus repeated measures ANCOVA models tested whether there were differential changes in the continuous outcomes across conditions over the study period (condition was a 4-level between-subjects factor, time was a 3-level within-subject factor). Time × Condition interactions indicated there was significantly differential change across conditions for depressive symptoms (F [6,674] = 6.33; p < .001; η2 = .05), BDI (F [6,674] = 6.14; p < .001; η2 = .05), social adjustment (F [3,337] = 3.51; p = .016; η2 = .03), and substance use (F [6,674] = 3.60; p = .002; η2 = .03), but not for bulimic symptoms (F [6,674] = 1.14; p = .339; η2 = .01). There were no significant Time X Condition X School interactions for the continuous outcomes, suggesting that intervention effects were similar across schools. For outcomes with significant omnibus Time X Condition interactions, separate follow-up repeated measures ANCOVA models tested whether groups significantly differed from each other from pre to post and from pre to 6-month follow-up. The Time X Condition interactions (Table 2) test whether participants in one condition showed significantly greater changes on the outcome than those in the other condition.
Table 2.
Repeated Measures ANCOVA Pairwise Contrasts
| CB | Supportive-expressive | Bibliotherapy | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coeff | SE | 95% CI | p | d | Coeff | SE | 95% CI | p | d | Coeff | SE | 95% CI | p | d | ||
| Supportive | ||||||||||||||||
| - Pre to post | .10 | .04 | .02–.17 | .011 | .28 | |||||||||||
| - Pre to 6 mo. | .04 | .04 | −.04–.13 | .304 | .11 | |||||||||||
| Bibliotherapy | ||||||||||||||||
| - Pre to post | .19 | .04 | .11–.27 | <.001 | .52 | .10 | .04 | .01–.17 | .022 | .28 | ||||||
| - Pre to 6 mo. | .06 | .04 | −.03–.15 | .180 | .18 | .01 | .04 | −.07–.10 | .737 | .03 | ||||||
| Control | ||||||||||||||||
| - Pre to post | .17 | .04 | .10–.25 | <.001 | .46 | .07 | .04 | .01–.15 | .074 | .19 | .02 | .04 | −.06–.10 | .593 | .04 | |
| - Pre to 6 mo. | .16 | .04 | .08–.25 | <.001 | .42 | .12 | .04 | .03–.20 | .008 | .28 | .10 | .04 | .01–.19 | .023 | .28 | |
| Supportive | ||||||||||||||||
| - Pre to post | 2.59 | 0.97 | 0.69–4.49 | .008 | .29 | |||||||||||
| - Pre to 6 mo. | 0.48 | 1.06 | −1.60–2.56 | .654 | .05 | |||||||||||
| Bibliotherapy | ||||||||||||||||
| - Pre to post | 3.76 | 0.99 | 1.82–5.70 | <.001 | .41 | 1.17 | 0.99 | −0.77–3.11 | .240 | .13 | ||||||
| - Pre to 6 mo. | 3.81 | 1.09 | 1.67–5.95 | <.001 | .38 | 3.33 | 1.09 | 1.19–5.47 | .002 | .33 | ||||||
| Control | ||||||||||||||||
| - Pre to post | 4.51 | 0.98 | 2.59–6.43 | <.001 | .50 | 1.92 | 0.98 | 0.00–3.84 | .051 | .21 | .75 | 1.00 | −1.21–2.71 | .456 | .08 | |
| - Pre to 6 mo. | 3.87 | 1.08 | 1.75–5.99 | <.001 | .39 | 3.39 | 1.08 | 1.27–5.51 | .002 | .34 | .06 | 1.11 | −2.12–2.24 | .957 | .01 | |
| Supportive | ||||||||||||||||
| - Pre to 6 mo. | .12 | .06 | .02–.23 | .023 | .28 | |||||||||||
| Bibliotherapy | ||||||||||||||||
| - Pre to 6 mo. | .14 | .06 | .03–.25 | .012 | .29 | .02 | .06 | −.09–.13 | .758 | .03 | ||||||
| Control | ||||||||||||||||
| - Pre to 6 mo. | .16 | .06 | .05–.27 | .004 | .35 | .04 | .06 | −.07–.15 | .511 | .04 | .02 | .06 | −.09–.13 | .736 | .03 | |
| Supportive | ||||||||||||||||
| - Pre to post | .06 | .03 | −.01–.13 | .069 | .19 | |||||||||||
| - Pre to 6 mo. | .09 | .04 | .00–.17 | .042 | .20 | |||||||||||
| Bibliotherapy | ||||||||||||||||
| - Pre to post | .08 | .04 | .01–.02 | .027 | .21 | .02 | .04 | −.05–.09 | .656 | .03 | ||||||
| - Pre to 6 mo. | .11 | .04 | .02–.19 | .013 | .28 | .02 | .04 | −.06–.11 | .608 | .04 | ||||||
| Control | ||||||||||||||||
| - Pre to post | .08 | .04 | .01–.15 | .019 | .28 | .02 | .04 | −.05–.09 | .584 | .01 | <.01 | .04 | −.07–.07 | .924 | .01 | |
| - Pre to 6 mo. | .17 | .04 | .09–.26 | <.001 | .46 | .09 | .04 | .01–.17 | .035 | .21 | .07 | .04 | −.02–.15 | .121 | .19 | |
Note. CB = Cognitive-Behavioral Therapy; Coeff = coefficient; SE = standard error; d = Cohen’s d; CI = confidence interval; p = p-value.
CB participants showed significantly greater reductions in depressive symptoms than assessment-only controls by posttest and 6-month follow-up. CB participants also showed significantly greater reductions in depressive symptoms than supportive-expressive and bibliotherapy participants at posttest, but not at 6-month follow-up. Supportive-expressive and bibliotherapy participants showed significantly greater reductions in depressive symptoms than assessment-only controls at 6-month follow-up, but not at posttest. Supportive-expressive participants showed significantly greater reductions in depressive symptoms than bibliotherapy participants at posttest, but not at 6-month follow-up.
The number of sessions attended for the CB condition (M = 3.3, SD = 2.5) correlated with change in depressive symptoms from pre to post (r = .27; p= .012), suggesting that the more sessions attended, the greater the reduction in depressive symptoms. In contrast, the amount of pages read for bibliotherapy participants was not significantly correlated with change in depressive symptoms from pre to post (r = .06; p = .59).
CB participants showed significantly greater improvements in social adjustment than supportive-expressive, bibliotherapy, and assessment-only participants at 6-month follow-up (this measure was not administered at posttest). Post hoc analyses revealed that the CB participants improved the greatest within the school adjustment domain. There were no significant differences in change for social adjustment for supportive-expressive, bibliotherapy, or assessment-only participants.
CB participants showed significantly greater reductions in substance use than assessment-only controls at posttest and 6-month follow-up. CB participants also showed significantly greater reductions in substance use relative to supportive-expressive participants at 6-month follow-up (but not at posttest) and relative to bibliotherapy participants at both posttest and 6-month follow-up. Supportive-expressive participants showed significantly less increases in substance use than assessment-only controls at 6-month follow-up, but not at posttest. The significant effects for the continuous outcomes were small to medium in magnitude.
We used the reliable change index to test for clinical significant change in depressive symptoms and social adjustment over the 6-month follow-up (Jacobson & Truax, 1991). There were significantly different rates of reliable change in depressive symptoms (χ2 [3/341] = 10.37, p = .016) and social adjustment (χ2 [3/325] = 10.58, p = .014) across conditions. Follow-up contrasts for depressive symptoms indicated that reliable change rates were significantly higher in CB (43%, p = .002, OR = 2.9, 95% CI = 1.5 – 5.8), supportive-expressive (36%, p = .021, OR = 2.3, 95% CI = 1.1 – 4.5), and bibliotherapy participants (35%, p = .036, OR = 2.1, 95% CI = 1.1 – 4.3) than in assessment-only controls (20%). Follow-up contrasts for social adjustment indicated that reliable change rates were significantly higher in CB participants (33%) than in the bibliotherapy (13%, p = .005, OR = 3.1, 95% CI = 1.4 – 7.0) and assessment-only participants (16%, p = .017, OR = 2.5, 95% CI = 1.2 – 5.2; respectively).
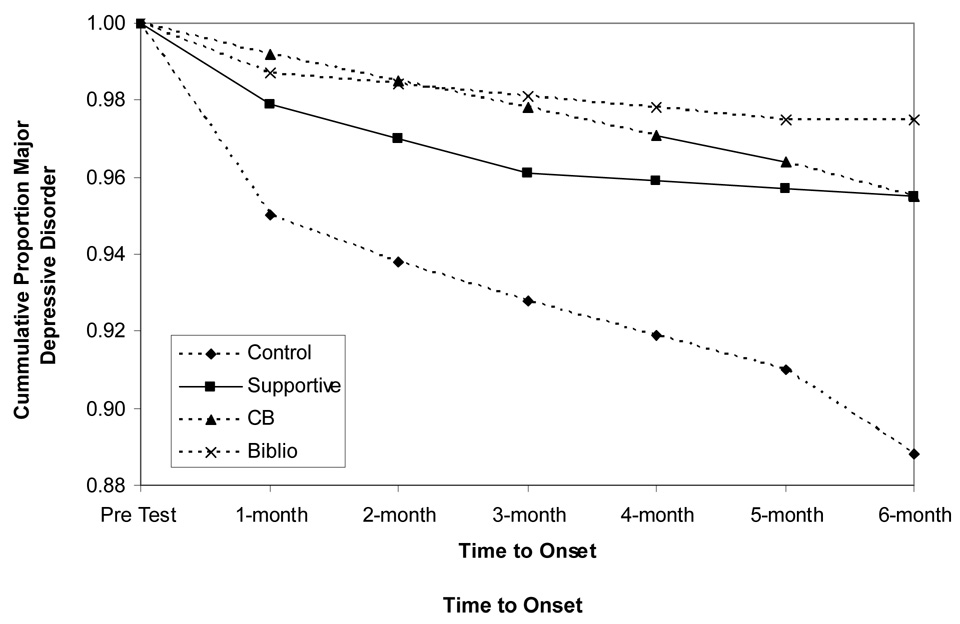
Intervention Effects for Major Depression Onset
By 6-month follow-up, 25 (7.3%) of the participants had shown onset of major depression: 11 control participants (13.1%), 6 CB participants (6.8%), 6 supportive-expressive participants (6.7%), and 2 bibliotherapy participants (2.5%). Figure 1 shows cumulative survival functions adjusted for pretest depressive symptoms for the percentage of participants in each condition that showed onset of major depression from pretest to 6-month follow-up. Cox proportional hazard models indicated that CB, supportive-expressive, and bibliotherapy participants showed a significantly lower risk for major depression onset over the 6-month follow-up period than assessment-only controls (β = .92, p < .05, OR = 2.5; β = .89, p < .05, OR = 2.4; and β = 1.51, p < .05, OR = 4.5 respectively), controlling for pretest depressive symptoms. The differences in major depression onset rates across the three active interventions were not significant.
Figure 1.
Covariate-adjusted survival curves for onset of major depression by intervention condition
Discussion
The first aim was to test whether a brief CB depression prevention program would outperform an assessment-only control group. Results indicated that this brief CB intervention produced significantly greater reductions in depressive symptoms than observed in assessment-only controls at posttest and 6-month follow-up and that these changes were clinically significant. These results are similar to those observed for longer selected (Clarke et al., 2001; Seligman et al., 2007) and universal (Jaycox et al., 1994; Spence et al., 2003) CB depression prevention programs. The present effect sizes for depressive symptoms (d = .46) at posttest and d = .42 at 6-month follow-up) were medium in magnitude and compare well to the average effect sizes at these time points from recent meta-analytic reviews of depression prevention programs (d = .16 and .11 respectively; [Horowtiz & Garber, 2006]) and (d = .28 and .20 respectively; [Stice, Shaw et al., 2008]), particularly give that our intervention was only 6 sessions (vs. an average of 11 sessions). The average effect size for the 6-session version of our CB depression prevention program (d = .44) was smaller than the average effect size from our early evaluation of our 4-session version of this intervention (d = .65; Stice et al., 2006); it is possible that this latter effect size was larger because that trial included college students, whereas the present trial focused on high school students. It was also encouraging that the CB intervention significantly reduced risk for onset of major depression relative to assessment-only controls, that only two depression prevention programs have achieved this effect (Clarke et al., 2001; Young, Mufson, & Davies, 2006). Furthermore, the fact that the majority of participants were ethnic minority youth suggests that this intervention may be effective for diverse populations.
The average participant in the present study attended only 3.3 of our 6 sessions (55%), which is proportionally similar to the average attendance rate of 9 out of 15 session intervention (60%) for Clarke et al., (1995) and the 6.7 out of 12 session intervention (56%) for Gillham et al., (2007). These findings imply that merely shortening an intervention does not result in proportionally greater attendance. The fact that session attendance is considerably higher (91%) for eating disorder prevention programs (Stice. Marti et al., 2008) suggests that individuals who sign up for selected depression prevention programs may have characteristics that limit attendance (i.e., hopelessness or pessimism). We found that offering snacks to students and holding raffles for prizes for those attending all sessions improved attendance. However, we suspect that session attendance could be improved by including more fun activities and using motivational enhancement exercises to combat the pessimism and hopelessness that high-risk adolescents may experience. Fortunately, both group interventions were intentionally designed to provide basically the same information in each session (e.g., each CB session consisted of a “changing doing” and a “changing thinking” segment). Therefore, missing any one session would not have resulted in the participant missing an essential element of the intervention.
The second aim was to test whether the brief CB program outperformed two alternative interventions. We compared group CB to supportive-expressive therapy and CB bibliotherapy as they can be conceptualized as dismantled aspects of group CB, with the supportive-expressive group providing nonspecific therapeutic factors without a CB-specific focus, and bibliotherapy delivering CB content without group-based nonspecific factors. The CB program produced significantly larger reductions in depressive symptoms by posttest than both alternative interventions, but these effects were nonsignificant at 6-month follow-up and there were no significant differences in the rates of major depression onset across the three interventions. This is a novel contribution to the literature because few trials have compared a CB depression prevention program to credible alternative interventions. On the one hand, it was noteworthy that the present CB program produced larger intervention effects relative to both a structurally equivalent intervention that contained all of the nonspecific elements of group therapy and a program that contained similar cognitive-behavioral content for certain outcomes and at certain follow-up assessments. To our knowledge, this trial has provided the most rigorous test of a CB depression prevention intervention to date. Findings imply that the stronger intervention effects observed for the group CB intervention were due to a confluence of both nonspecific factors and CB content. Findings also suggested that CB produces a more rapid reduction in depressive symptoms than the other alternative interventions. The present findings converge with prior randomized trials in which CB treatment for adolescent depression has produced significantly greater pre to post reductions in depressive symptoms than alternative active interventions, such as family therapy, non-directive supportive-expressive therapy, and life skills training (Brent et al., 1997; Rohde et al., 2004; Shaw, 1977), though other treatment trials have not found that CBT produced superior effects to alternative interventions (Jacobson et al., 1996; Reynolds & Coats, 1986; Treatment for Adolescents with Depression Study Team, 2004).
On the other hand, certain effects did not persist through 6-month follow-up and CB did not reduce risk for onset of major depression relative to both supportive-expressive and bibliotherapy, which is arguably the most important outcome for a depression prevention trial. This does not appear to be solely due to the passage of time, as the participants in the assessment-only condition showed higher rates of depression onset through 6-month follow-up and did not show the reductions in depressive symptoms by 6-month follow-up seen in the three active intervention conditions. Although it is tempting to conclude that these null findings at 6-month follow-up suggest that the effects are merely due to nonspecific factors, this seems unlikely given that these processes would have both been most potent from pre to post – which is the interval over which CB significantly outperformed both alternative interventions. Moreover, CB did produce stronger effects for social adjustment and substance use that persisted through 6-month follow-up, which cannot be easily attributed to nonspecific effects. Interestingly, even the current treatments of choice for certain disorders, such as CBT for bulimia nervosa, binge eating disorder, and depression, often do not significantly outperform alternative interventions over long-term follow-ups, though they typically do in the short-term (Brent et al., 1997; Fairburn et al., 1995; Wilfley et al., 2002). Similarly, certain eating disorder prevention programs have produced significantly stronger intervention effects than alternative interventions, but these effects likewise fade over follow-up (Stice, Marti et al., 2008). These sleeper effects, in which individuals in the active comparison conditions show improvement after posttest (see Table 1) implies that if an individual engages in any intervention, they may be more willing to try alternative methods of resolving the problem in the future. Perhaps once individuals commit to an intervention, they shift from a contemplation phase to an action phase as suggested by the transtheoretical model of behavior change (Prochaska & DiClemente, 1986). This may explain why CB did not significantly reduce risk for onset of major depression relative to the supportive-expressive and bibliotherapy control conditions.
It is important to acknowledge that both bibliotherapy and the supportive-expressive intervention produced significantly stronger reductions in depressive symptoms relative to the assessment-only control condition by 6-month follow-up, which were clinically significant, even though the effects were not significant at posttest. This is noteworthy given that only 25% of depression prevention programs that have been evaluated in previous trials have achieved this effect (Stice, Shaw et al., 2008). Even more impressive is the fact that both CB bibliotherapy and the supportive-expressive intervention significantly reduced the risk for future major depression onset because only 8% of previously evaluated prevention programs have produced such a prophylactic effect (Clarke et al., 2001; Young et al., 2006). The positive effects for bibliotherapy are particularly noteworthy because they replicate and extend findings from our earlier preliminary prevention trial (Stice et al., 2006). These findings suggest it may be worth investigating bibliotherapy further given that it is considerably easier and less expensive than a group intervention, though satisfaction was lowest in the bibliotherapy condition. Regarding the degree of participation in bibliotherapy, while the selected book is quite long (over 600 pages), the reader is taught the general model of cognitive therapy for depression in the first 50 pages. Therefore, even a partial “dose” of the intervention may be sufficient for an effect. We are less enthusiastic regarding effectiveness and dissemination research for the supportive-expressive intervention because it is more difficult to administer than the more scripted CB group intervention and requires closer supervision of the facilitators.
The third aim was to test whether the CB intervention produced significantly stronger improvements in social adjustment and reductions in binge eating and substance use. The evidence that the CB participants showed significantly larger improvements in social adjustment, particularly in the school setting, relative to supportive-expressive, bibliotherapy, and assessment-only controls is noteworthy, as most past trials have not included this type of ecologically valid outcome. These effects were small to moderate in magnitude. These findings are important because disturbances in these functional domains have been found to increase risk for onset of future major depression (Lewinsohn et al., 1994). The fact that neither supportive-expressive or bibliotherapy participants showed stronger improvements on this outcome than assessment-only controls provides an additional indication to the superiority of the group CB intervention. The improvements in social adjustment, in addition to reductions in current and future depression, may justify the added expense of providing group CB over bibliotherapy.
It was encouraging that CB participants showed decreases in substance use over follow-up relative to the increases observed for supportive-expressive, bibliotherapy, and assessment-only controls. These effects were small to medium in magnitude. That this effect emerged relative to all three comparison groups and that neither the supportive-expressive or bibliotherapy intervention produced effects for this ecologically valid outcome provides another indication of the superiority of the CB intervention. These findings are noteworthy because a review of the literature suggests that most substance abuse prevention programs have not produced such prophylactic effects, particularly in relation to alternative interventions. The fact that this effect did not emerge in the previous trial of the 4-session version of this brief intervention (Stice et al., 2006) implies that a more intensive dose may be necessary to realize this effect. Although it is tempting to conclude that those in the CB intervention showed reductions in substance use because they had less negative affect that motivated them to use substances, other active interventions did produce significant decreases in depressive symptoms. Findings might suggest that social adjustment changes drive the effects for substance use, as adjustment effects were specific to the CB intervention. The dual effects for depression and substance use are encouraging because prevention programs that produce effects for more than one psychiatric problem have greater public health utility and cost effectiveness than those that produce effects for only one problem.
The CB intervention did not produce reductions in bulimic symptoms as observed in an earlier trial involving young women (Burton et al., 2007). The fact that post hoc analyses indicated that these effects did not emerge in the present trial when we focused exclusively on adolescent girls suggests that this effect is relatively small and only inconsistently observed.
The limitations of this trial should be noted. First, it was not possible to assess all outcomes that might have been affected by these interventions (e.g., anxiety disorders and social support) because of respondent burden concerns. Second, all of the outcomes relied on youth self-report. Greater confidence could be placed in the findings if multiple informants had been used. Third, it would have been desirable to collect objective measures of social adjustment, such as grades and attendance data from the schools. Fourth, because we did not exclude participants with previous depressive episodes, it is possible that the interventions prevent onset of a mixture of first major depression episodes and recurrent episodes. Finally, it would have been useful to collect more systematic data on potential contamination across conditions, as to our knowledge this question has not been addressed with empirical data from large prevention trials.
In balance, results suggest that this brief CB depression prevention program produced clinically meaningful intervention effects, including reductions in depressive symptoms and substance use, lower risk for onset of major depression, and improved social adjustment. Most effects emerged relative to the assessment-only control condition, but many emerged relative to alternative interventions. Although the alternative interventions produced several effects, the magnitude and breadth of the effects were greater for the CB program. Future reports will test whether these effects persist over a longer-term follow-up, will examine of the mediators that theoretically account for the effects of each intervention, and will explore moderators of the intervention effects. Nonetheless, the results from this trial, in conjunction with the positive effects observed for earlier iterations of this intervention (Burton et al., 2007; Stice et al., 2006), imply that it may be time to initiate an effectiveness trial that tests whether the brief CB depression prevention program produces effects when school staff (e.g., school counselors and nurses) recruit and deliver the intervention in schools. Few prevention programs have been evaluated in effectiveness trials. The brief nature of this CB intervention may make it particularly attractive to schools and should make it easier and less expensive to implement. Future research should also examine ways of increasing the effects of CB prevention programs, such as increasing session attendance, improving homework compliance, or supplementing group CB with bibliotherapy. Finally, research should begin to investigate dissemination of brief CB depression prevention programs, with a focus on barriers that will hamper wide-scale implementation. With ongoing programmatic research, we may yet realize the ultimate goal of reducing the prevalence of depression through prevention.
Acknowledgments
This study was supported by a research grant (MH67183) from the National Institute of Health.
Thanks go to project research assistants, Courtney Byrd, Kathryn Fischer, Amy Folmer, Cassie Goodin, Jacob Mase, and Emily Wade, a multitude of undergraduate volunteers, the Austin Independent School District, and the participants who made this study possible.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at http://www.apa.org/journals/ccp/
References
- Ackerson J, Scogin F, McKendree-Smith N, Lyman RD. Cognitive bibliotherapy for mild and moderate adolescent depressive symptomatology. Journal of Counseling and Clinical Psychology. 1998;66:685–690. doi: 10.1037//0022-006x.66.4.685. [DOI] [PubMed] [Google Scholar]
- American Psychological Association Task Force on Psychological Intervention Guidelines. Template for developing guidelines: Interventions for mental disorders and psychological aspects of physical disorders. Washington, DC: APA; 1995. [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. New York: International University Press; 1976. [Google Scholar]
- Beck AT, Steer RM, Garbin M. Psychometric properties of the Beck Depression Inventory: 25 years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Brent DA, Holder D, Kolko D, Birmaher B, Baugher M, Roth C, Iyengar S, Johnson BA. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Archives of General Psychiatry. 1997;54:877–885. doi: 10.1001/archpsyc.1997.01830210125017. [DOI] [PubMed] [Google Scholar]
- Burton EM, Stice E, Bearman SK, Rohde P. An experimental test of the affect-regulation model of bulimic symptoms and substance use: An affective intervention. International Journal of Eating Disorders. 2007;40:27–36. doi: 10.1002/eat.20292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke G, Hawkins W, Murphy M, Sheeber L, Lewinsohn PM, Seeley JR. Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: A randomized trial of group cognitive intervention. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:312–321. doi: 10.1097/00004583-199503000-00016. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Hornbrook M, Lynch F, Polen M, Gale J, Beardslee W, O’Connor E, Seeley J. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Archives of General Psychiatry. 2001;58:1127–1134. doi: 10.1001/archpsyc.58.12.1127. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Norman PA, Welch SL, O’Connor ME, Doll HA, Peveler RC. A prospective study of outcome in bulimia nervosa and the long-term effects of three psychological treatments. Archives of General Psychiatry. 1995;52:304–312. doi: 10.1001/archpsyc.1995.03950160054010. [DOI] [PubMed] [Google Scholar]
- Gillham JE, Hamilton J, Fresesm DR, Patton K, Gallop R. Preventing depression among early adolescents in the primary care setting: A randomized controlled study of the Penn Resiliency Program. Journal of Abnormal Child Psychology. 2006;34:203–219. doi: 10.1007/s10802-005-9014-7. [DOI] [PubMed] [Google Scholar]
- Gillham JE, Reivich KJ, Freres DR, Chaplin TM, Shatte AJ, Samuels B, et al. School-based prevention of depressive symptoms: A randomized controlled study of the effectiveness and specificity of the Penn Resiliency Program. Journal of Consulting and Clinical Psychology. 2007;75:9–19. doi: 10.1037/0022-006X.75.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillham JE, Reivich KJ, Freres DR, Lascher M, Litzinger S, Shatte A, Seligman ME. School-based prevention of depression and anxiety symptoms in early adolescence: A pilot of a parent intervention component. School Psychology Quarterly. 2006;21:323b–348b. [Google Scholar]
- Gregory RJ, Schwer-Canning S, Lee TW, Wise JC. Cognitive bibliotherapy for depression: A meta-analysis. Professional Psychology: Research and Practice. 2004;35:275–280. [Google Scholar]
- Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan JK, et al. A component analysis of cognitive-behavioral treatment for depression. Journal of Consulting and Clinical Psychology. 1996;64:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jaycox LH, Reivich KJ, Gillham J, Seligman MEP. Prevention of depressive symptoms in school children. Behavioral Research and Therapy. 1994;32:801–816. doi: 10.1016/0005-7967(94)90160-0. [DOI] [PubMed] [Google Scholar]
- Klein DN, Torpey DC, Bufferd SJ. Depressive disorders. In: Beauchaine TP, Hinshaw SP, editors. Child and Adolescent Psychopathology. 2008. pp. 477–509. [Google Scholar]
- Kolko DJ, Brent DA, Baugher M, Bridge J, Birmaher B. Cognitive and family therapies for adolescent depression: Treatment specificity, mediation, and moderation. Journal of Consulting and Clinical Psychology. 2000;68:603–614. [PubMed] [Google Scholar]
- Lewinsohn PM, Roberts RE, Seeley JR, Rohde P, Gotlib IH, Hops H. Adolescent psychopathology: II. Psychosocial risk factors for depression. Journal of Abnormal Psychology. 1994;103:302–315. doi: 10.1037//0021-843x.103.2.302. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Youngren MA, Grosscup SJ. Reinforcement and depression. In: Dupue RA, editor. The psychobiology of depressive disorders: Implications for the effects of stress. New York: Academic Press; 1979. pp. 291–316. [Google Scholar]
- McCarthy M. The thin ideal, depression, and eating disorders in women. Behavioral Research and Therapy. 1990;28:205–218. doi: 10.1016/0005-7967(90)90003-2. [DOI] [PubMed] [Google Scholar]
- Merry S, McDowell H, Wild C, Bir J, Cunliffe R. A randomized placebo-controlled trial of a school-based depression prevention program. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:538–547. doi: 10.1097/00004583-200405000-00007. [DOI] [PubMed] [Google Scholar]
- Newman DL, Moffitt TE, Caspi A, Magdol L, Silva PA, Stanton WR. Psychiatric disorder in a birth cohort of young adults: Prevalence, comorbidity, clinical significance, and new case incidence from ages 11 to 21. Journal of Consulting and Clinical Psychology. 1996;64:552–562. [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Girgus JS, Seligman ME. Predictors and consequences of childhood depressive symptoms: A 5-year longitudinal study. Journal of Abnormal Psychology. 1992;101:405–422. doi: 10.1037//0021-843x.101.3.405. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Stice E, Wade E, Bohon C. Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in adolescent females. Journal of Abnormal Psychology. 2007;116:198–207. doi: 10.1037/0021-843X.116.1.198. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Toward a comprehensive model of behavior change. In: Miller WR, Heather N, editors. Treating addictive behaviors: Processes of change. New York: Plenum Press; 1986. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reynolds WM, Coats KI. A comparison of cognitive-behavioral therapy and relaxation training for the treatment of depression in adolescents. Journal of Consulting and Clinical Psychology. 1986;54:653–660. doi: 10.1037//0022-006x.54.5.653. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: A comparison of depression scales. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:58–66. doi: 10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- Rohde P, Clarke GN, Mace DE, Jorgensen JS, Seeley JR. An efficacy/effectiveness study of cognitive-behavioral treatment for adolescents with comorbid major depression and conduct disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:660–668. doi: 10.1097/01.chi.0000121067.29744.41. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Seligman ME, Schulman P, DeRubeis RJ, Hollon SD. The prevention of depression and anxiety. Prevention and Treatment. 1999;2 np. [Google Scholar]
- Seligman ME, Schulman P, Tryon AM. Group prevention of depression and anxiety symptoms. Behaviour Research and Therapy. 2007;45:1111–1126. doi: 10.1016/j.brat.2006.09.010. [DOI] [PubMed] [Google Scholar]
- Shaw BF. Comparison of cognitive therapy and behavior therapy in the treatment of depression. Journal of Consulting and Clinical Psychology. 1977;45:543–551. doi: 10.1037//0022-006x.45.4.543. [DOI] [PubMed] [Google Scholar]
- Shochet IM, Dadds MR, Holland D, Whitefield K, Harnett PH, Osgarby SM. The efficacy of a universal school-based program to prevent adolescent depression. Journal of Clinical Child Psychology. 2001;30:303–315. doi: 10.1207/S15374424JCCP3003_3. [DOI] [PubMed] [Google Scholar]
- Spence SH, Sheffield JK, Donovan CL. Preventing adolescent depression: An evaluation of the problem solving for life program. Journal of Consulting and Clinical Psychology. 2003;71:3–13. doi: 10.1037//0022-006x.71.1.3. [DOI] [PubMed] [Google Scholar]
- Stice E, Barrera M, Jr, Chassin L. Prospective differential prediction of adolescent alcohol use and problem use: Examining mechanisms of effect. Journal of Abnormal Psychology. 1998;107:616–628. doi: 10.1037//0021-843x.107.4.616. [DOI] [PubMed] [Google Scholar]
- Stice E, Burton E, Bearman SK, Rohde P. Randomized trial of a brief depression prevention program: An elusive search for a psychosocial placebo control condition. Behaviour Research and Therapy. 2006;45:863–876. doi: 10.1016/j.brat.2006.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Hayward C, Cameron R, Killen JD, Taylor CB. Body image and eating related factors predict onset of depression in female adolescents: A longitudinal study. Journal of Abnormal Psychology. 2000;109:438–444. [PubMed] [Google Scholar]
- Stice E, Marti N, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. 2008 doi: 10.1037/a0015168. Submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treatment for Adolescents with Depression Study Team. The Treatment for Adolescents with Depression Study (TADS): Short-Term Effectiveness and Safety Outcomes. Journal of the American Medical Association. 2004;292:807–820. [Google Scholar]
- Young JF, Mufson L, Davies M. Efficacy of interpersonal psychotherapy-adolescent skills training: An indicated preventive intervention for depression. Journal of Child Psychology and Psychiatry. 2006;47:1254–1262. doi: 10.1111/j.1469-7610.2006.01667.x. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Orvaschel H, Padian N. Children's symptom and social functioning self-report scales: Comparison of mothers' and children's reports. Journal of Nervous and Mental Disease. 1980;168:736–740. doi: 10.1097/00005053-198012000-00005. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Welch R, Stein R, Borman Spurrell E, Cohen LR, Saelens BE, et al. A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Archives of General Psychiatry. 2002;59:713–721. doi: 10.1001/archpsyc.59.8.713. [DOI] [PubMed] [Google Scholar]