Serious outbreaks of food-borne illness, whether regional or national, dramatically raise community anxiety about personal health and increase the workloads of front-line physicians. The drama further increases when the offending microbe is not well known. This primer on listeriosis hones in on the microbe, the incidence of infection, clinical presentations, diagnosis, treatment and prevention. The information is based on a MEDLINE search on listeriosis and discussion with experts.
The microbe
Listeria monocytogenes is a small, gram-positive bacillus that can grow in anaerobic or aerobic conditions. It is found widely in the environment in soil, decaying vegetation and water and may be part of the fecal flora of many mammals, including healthy human adults.1
L. monocytogenes presents a particular concern with respect to food handling because it can grow at refrigerator temperatures (4°C to 10°C), temperatures commonly used to control pathogens in foods. Freezing also has little detrimental effect on the microbe. Although pasteurization is sufficient to kill Listeria, failure to reach the desired temperature in large packages can allow the organism to survive. Food can also be contaminated after processing by the introduction of unpasteurized material, as happens during the preparation of some cheeses. Listeria can also be spread by contact with contaminated hands, equipment and counter tops.
The centralized production of prepared ready-to-eat food products in Canada increases the risk of higher levels of contamination, since it requires that foods be stored for long periods at refrigerated temperatures that favour the growth of Listeria. During the preparation, transportation and storage of prepared foods, the organism can multiply to reach a threshold needed to cause infection.
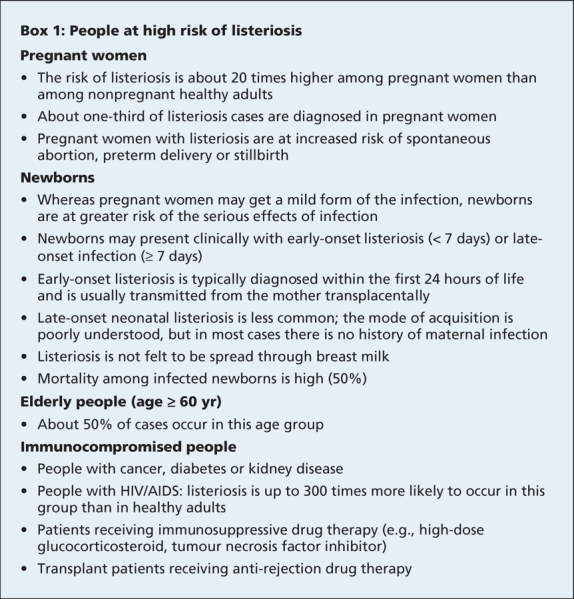
The approximate infective dose of L. monocytogenes is estimated to be 10–100 million colony forming units (CFU) in healthy hosts, and only 0.1–10 million CFU in people at high risk of infection (Box 1).2 Foods such as raw vegetables, raw (unpasteurized) milk and cheese, and meats (fresh and frozen) may become contaminated with L. monocytogenes because of where they come from and how they are processed. Ready-to-eat foods such as cold cuts or deli meats, cheeses and other dairy products are ideal sources for contamination.
Box 1.
Although L. monocytogenes was recognized as an animal pathogen over 80 years ago,3 the first outbreak confirming an indirect transmission from animals to humans was reported only in 1983, in Canada's Maritime provinces.4 In that outbreak, cabbages, stored in the cold over the winter, were contaminated with Listeria through exposure to infected sheep manure. A subsequent outbreak in California in 1985 confirmed the role of food in disseminating listeriosis. Since then Listeria has been implicated in many outbreaks of food-borne illness, most commonly from exposure to contaminated dairy products and prepared meat products, including turkey and deli meats, pâté, hot dogs and seafood and fish.5
Incidence of infection
The incidence of listeriosis is difficult to establish, since symptoms may be mistaken for a flu-like illness or gastroenteritis and appropriate cultures not obtained. The Canadian Listeriosis Reference Service was created in 2001 to actively investigate cases and develop a molecular epidemiology database of isolates as a resource for outbreak investigations. In 2006, listeriosis was named as a nationally notifiable disease by the Public Health Agency of Canada. Between 1995 and 1999 (the most recent years for which data are available), 25–51 cases occurred annually in Canada.6 However, passive surveillance programs such as this may suffer from underreporting of cases.5 Countries with surveillance programs have reported rates of infection from 0.6 to 6.2 cases per million, with countries having active surveillance programs reporting the highest incidence.5,7–11 The case-fatality rates vary from country to country, but invariably the highest mortality is among newborns with infection acquired from their mothers (25%–50%). Mortality among those over 60 years of age is also high (10%–20%).
Clinical presentations
Initial symptoms of infection include nonspecific flu-like symptoms, nausea, vomiting, cramps, diarrhea and fever. There are few clinical features that are unique to listeriosis. Therefore, clinicians must consider a variety of potential causes for infection, including viral infections (influenza) and other bacterial infections that may cause sepsis or meningitis. Symptoms can develop at any time from 2 to 70 days after eating contaminated food. Except for vertical mother–fetus transmission, most cases of listeriosis begin with ingestion of the organism from a food source.
Most healthy adults and children who consume contaminated food experience only mild to moderate symptoms. The infection is usually self-limited, since, in healthy hosts, exposure to Listeria stimulates the production of tumour necrosis factor and other cytokines, which activate monocytes and macrophages to eradicate the organism.12,13 Few people with normal immune function go on to have more severe, life-threatening forms of listeriosis, characterized by septic shock, meningitis and encephalitis.
In contrast, people with poor immune function are at much higher risk of severe, life-threatening forms of listeriosis. High-risk groups include pregnant women, newborns, elderly people (≥ 60 years of age) and people with a weakened immune system (Box 1). Individuals taking tumour necrosis factor inhibitors and transplant recipients taking anti-rejection drugs are now included in this high-risk group.14
Pregnant women with listeriosis may have only mild symptoms of the infection. However, they are at increased risk of having a spontaneous abortion during the first trimester or of giving birth to a premature infant with acute sepsis if they are exposed later in the pregnancy.
Newborns may present clinically with early- (< 7 days) or late-onset forms of infection (≥ 7 days). Those with the early-onset form are often diagnosed in the first 24 hours of life with sepsis. Early-onset listeriosis is most often acquired from the mother through transplacental transmission. Late-onset neonatal listeriosis is less common than the early-onset form. Clinical symptoms may be subtle and include irritability, fever and poor feeding.13 The mode of acquisition of late-onset listeriosis is poorly understood, but acquisition of the organism after birth is implicated, since there is usually no maternal infection in such cases. The organism is not felt to be spread through breast-feeding.
Common clinical features among patients with nonperinatal forms of listeriosis include meningitis (about 33% of such cases) and septicemia (25%). Less commonly, patients may have inflammatory gastroenteritis, endocarditis or joint infections.8,13
Diagnosis and management
Early diagnosis and treatment of listeriosis in high-risk patients is critical, since the outcome of untreated infection can be devastating. This is especially true for pregnant women because of the increased risk of spontaneous abortion and preterm delivery. Depending on the risk group, rates of death from listeriosis range from 10% to 50%, with the highest rate among newborns in the first week of life.
The Public Health Agency of Canada convened an expert panel in August 2008 to provide information to health care professionals and the general public on the diagnosis and management of listeriosis during the recent outbreak. The following information is based on the panel's discussion and addresses what should be done for patients who have eaten food items that are suspected of being contaminated with Listeria and who have symptoms of diarrhea with or without fever.
For healthy adults and children with a normal immune system, no Listeria-specific investigation is required. Gastroenteritis due to Listeria infection has a short duration and is self-limited in this population. Culture of a stool specimen for common bacterial enteric pathogens may be warranted if indicated by the person's history and clinical condition.
For high-risk patients (Box 1), more aggressive investigation and management strategies should be followed. If the patient has diarrhea only, culture of a stool specimen for common bacterial enteric pathogens may be indicated. If the patient has a fever, bacteremia must be suspected. Two blood samples for aerobic culture should be drawn. Listeria is only one of many bacteria that may cause infections in such patients; thus, investigations and treatment should be directed to cover common causes in addition to Listeria.
For pregnant women with a fever or signs of sepsis, blood and urine samples should be obtained for culture. Empiric therapy, including ampicillin, should be started for coverage of Listeria.
For infants born to women suspected of having listeriosis, blood cultures should be taken and antibiotic therapy started.
Listeria is susceptible to ampicillin, which should be given with gentamicin to patients with sepsis. If further advice on the management of patients with listeriosis is needed, it should be obtained in consultation with the appropriate specialist such as an obstetrician, a neonatologist or infectious disease specialist.
Prevention of infection
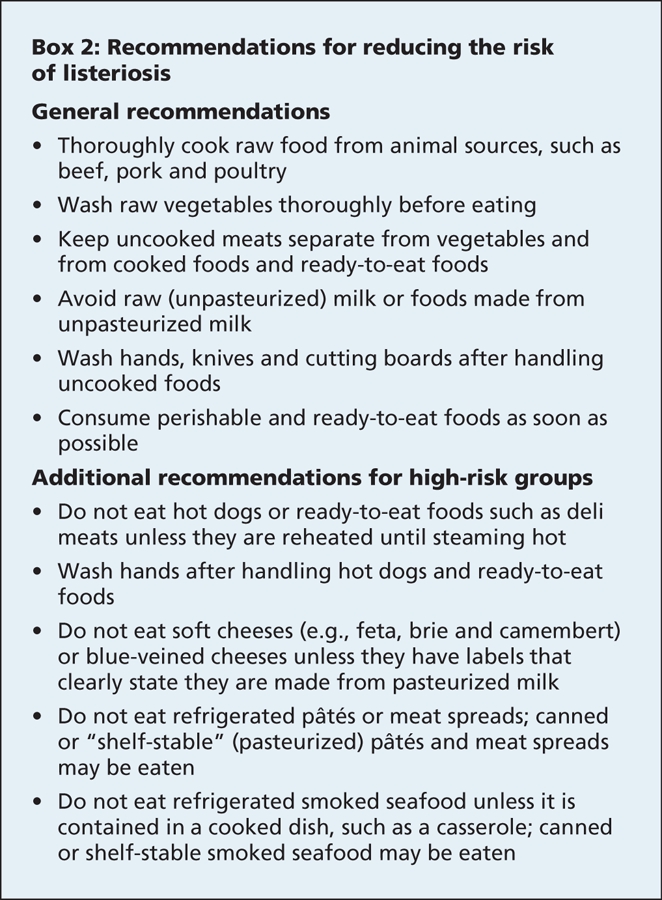
Given the characteristics of Listeria and the risk of infection, what can be done to minimize and prevent infection? The Canadian Food Inspection Agency and the US Centers for Disease Control and Prevention have made recommendations to protect against listeriosis in the home. People with a poor immune system and pregnant women are advised to take even more rigorous precautions by avoiding foods that may become contaminated with Listeria (Box 2).5,7
Box 2.
Summary
Although food-borne outbreaks of listeriosis are uncommon, they remain a major public health problem. In the United States, about 20%–65% of deaths from all food-borne infections are due to Listeria.5 Therefore, detecting an outbreak early and identifying its source is a priority. Prompt reporting of all cases of Listeria infection to public health authorities is important to assist them in early detection of an outbreak.
During an outbreak of listeriosis, vigilance in the preparation of food is especially important for immunocompromised patients and pregnant women. Initial manifestations of infection are nonspecific and include flu-like symptoms. Such symptoms should be thoroughly investigated if they develop in patients at high risk of listeriosis (Box 1). In contrast, in patients with normal immune function, symptoms are usually milder and the infection self-limited; such patients do not need tests or treatment. Proper preparation, storage and handling of food by industry and in the home can minimize the risk of a widespread outbreak.
Footnotes
Published at www.cmaj.ca on Sept. 11, 2008.
Competing interests: None declared.
Correspondence to: Dr. Robert Bortolussi, Department of Pediatrics, IWK Health Centre, Goldbloom Pavilion, 5890 University Ave., Halifax NS B3K 6R8; fax 902 470-7232; bob.bortolussi@iwk.nshealth.ca
REFERENCES
- 1.Schlech WF III, Schlech WF IV, Haldane H, et al. Does sporadic Listeria gastroenteritis exist? A 2-year population-based survey. Clin Infect Dis 2005;41:778-84. [DOI] [PubMed]
- 2.Farber JM, Ross WH, Harwig J. Health risk assessment of Listeria monocytogenes in Canada. Int J Food Microbiol 1996;30:145-56. [DOI] [PubMed]
- 3.Murray EGD, Webb RA, Swann MBR. A disease of rabbits characterized by a large mononuclear leucocytosis, caused by a hitherto undescribed Bacillus: Bacterium monocytogenes (n. sp.). J Pathol Bacteriol 1926;29:407.
- 4.Schlech WF III, Lavign PM, Bortolussi R, et al. Epidemic listeriosis — evidence for transmission by food. N Engl J Med 1983;308:203-6. [DOI] [PubMed]
- 5.Lynch M, Painter J, Woodruff R., et al. Surveillance for foodborne-disease outbreaks — United States, 1998–2002. MMWR Surveill Summ 2006; 55(SS10):1-34. Available: www.cdc.gov/mmwr/preview/mmwrhtml/ss5510a1.htm (accessed 2008 Sept 4). [PubMed]
- 6.Public Health Agency of Canada. Notifiable Diseases On-Line. Notifiable disease incidence by age group — listeriosis, 2006. Ottawa: The Agency. Available: http://dsol-smed.hc-sc.gc.ca/dsol-smed/ndis/c_age3_e.html (accessed 2008 Sept 6).
- 7.Food Safety Network. Listeria fact sheet — updated. Guelph (ON): University of Guelph; 2003. Available: www.foodsafetynetwork.ca/en/article-details.php?a=3&c=14&sc=112&id=439 (accessed 2008 Aug 25).
- 8.Koch J, Stark K. Significant increase of listeriosis in Germany — epidemiological patterns 2001–2005. Euro Surveill 2006;11:85-8. [PubMed]
- 9.Siegman-Igra Y, Levin R, Weinberger M, et al. Listeria monocytogenes infection in Israel and review of cases worldwide. Emerg Infect Dis 2002;8:305-10. [DOI] [PMC free article] [PubMed]
- 10.Okutani A, Okada Y, Yamamoto S, et al. Nationwide survey of human Listeria monocytogenes infection in Japan. Epidemiol Infect 2004;132:769-72. [DOI] [PMC free article] [PubMed]
- 11.Doorduyn Y, de Jager CM, van der Zwaluw WK, et al. Invasive Listeria monocytogenes infections in the Netherlands, 1995–2003. Eur J Clin Microbiol Infect Dis 2006;25:433-42. [DOI] [PubMed]
- 12.Cresence V, Dharsana K, Lekshmi M, et al. Listeria — review of epidemiology and pathogenesis. J Microbiol Immunol Infect 2007;40:4-13. [PubMed]
- 13.Bortolussi R, Mailman T. Listeriosis. In: Feigin R, Cherry J, Demmler-Harrison G, et al, editors. Textbook of Pediatric Infectious Diseases. 5th ed. Philadelphia (PA): WB Saunders; 2004. p. 1330-6.
- 14.Hamilton CD. Immunosuppression related to collagen-vascular disease or its treatment. Proc Am Thorac Soc 2005;2:456-60. [DOI] [PMC free article] [PubMed]


