Abstract
Primaquine—an 8-aminoquinoline derivative—is one of the most effective drugs for use against the tissue stages of the malaria parasite. Unfortunately certain persons suffer from an inherited defect of metabolism which renders them susceptible to haemolysis after ingestion of the 8-aminoquinolines, certain other drugs and some vegetables. Susceptibility appears to be inherited by a partially dominant sex-linked gene of variable expression. In persons with full expression of this defect, intravascular haemolysis may be of such severity as to mimic blackwater fever.
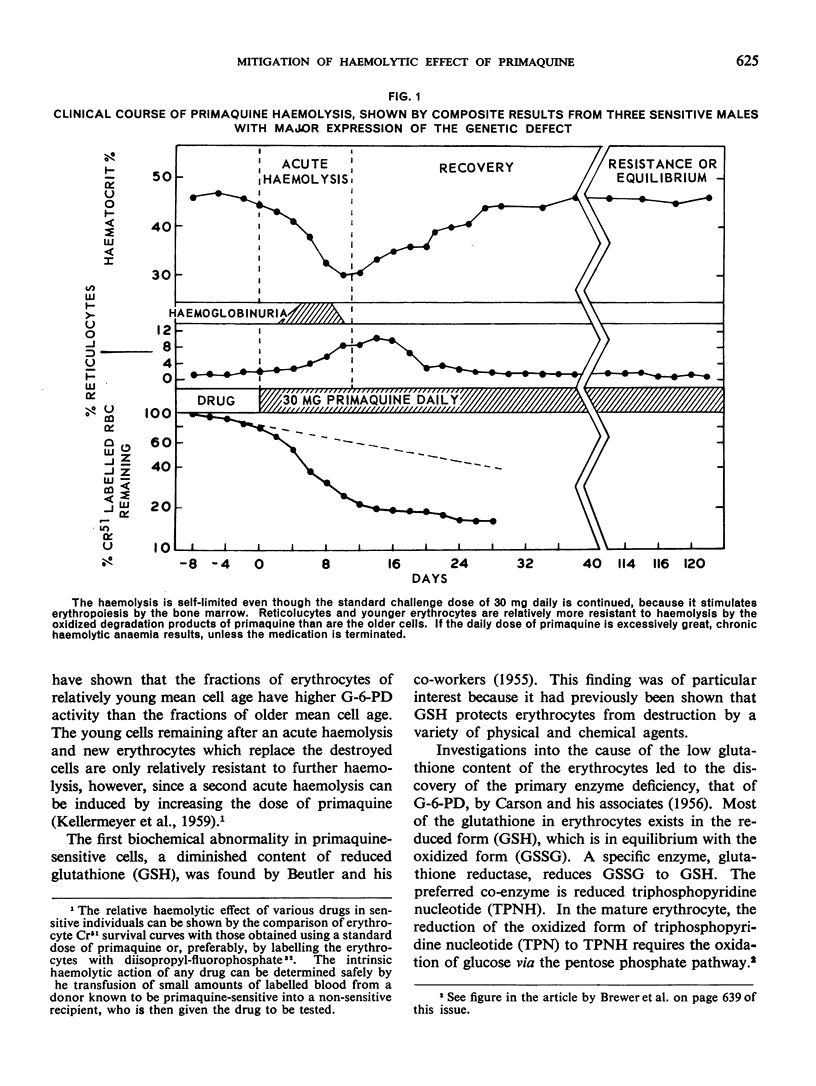
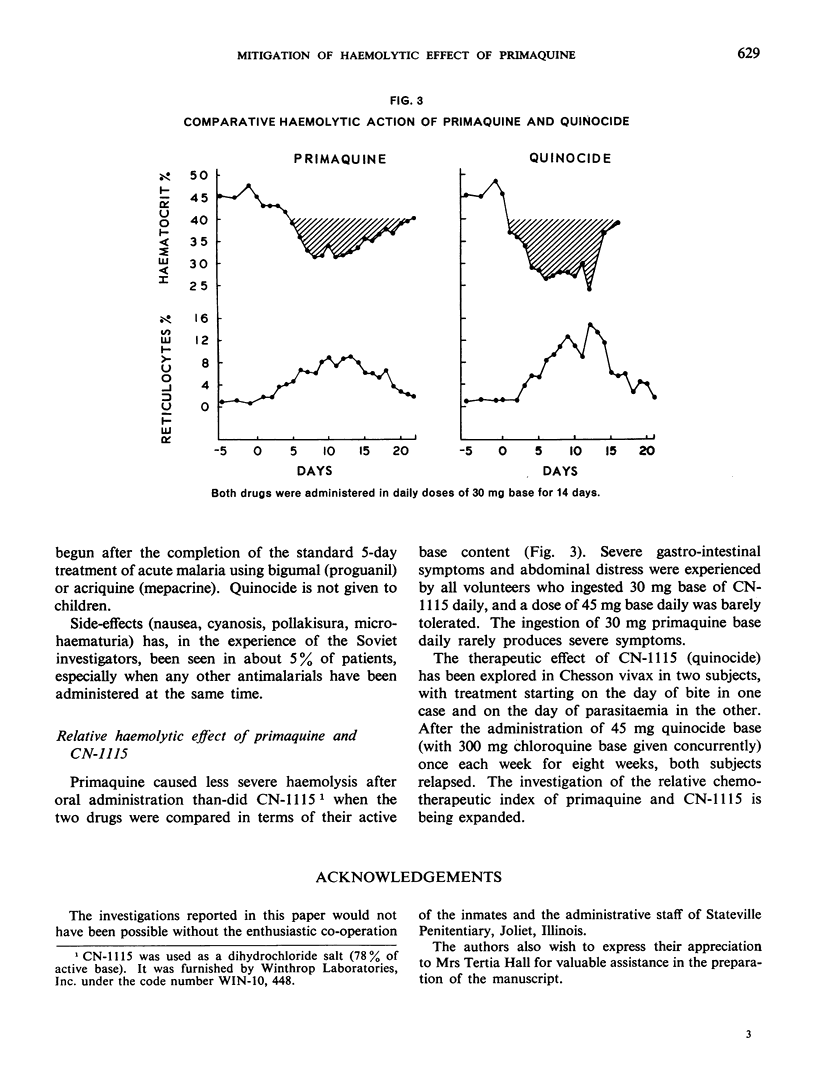
It has been shown that the haemolysis caused by daily doses of primaquine is self-limited, provided that such doses are not excessive, by virtue of the fact that the younger erythrocytes are relatively resistant to destruction by the drug.
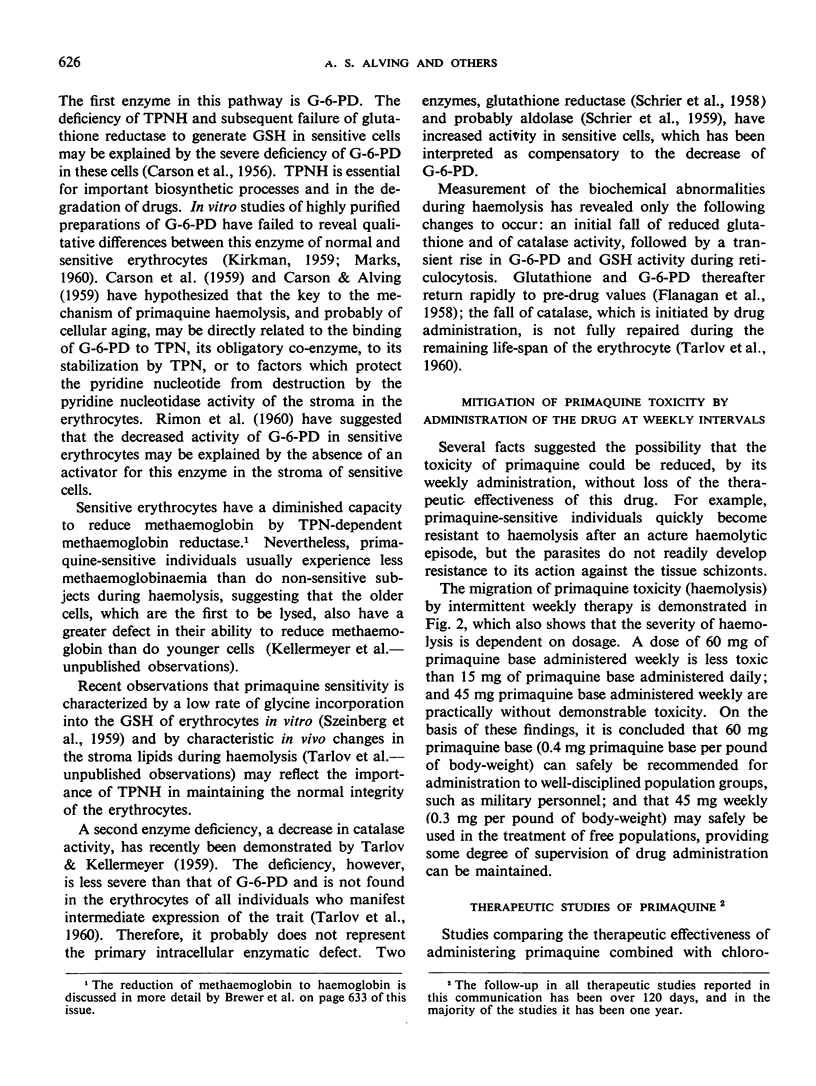
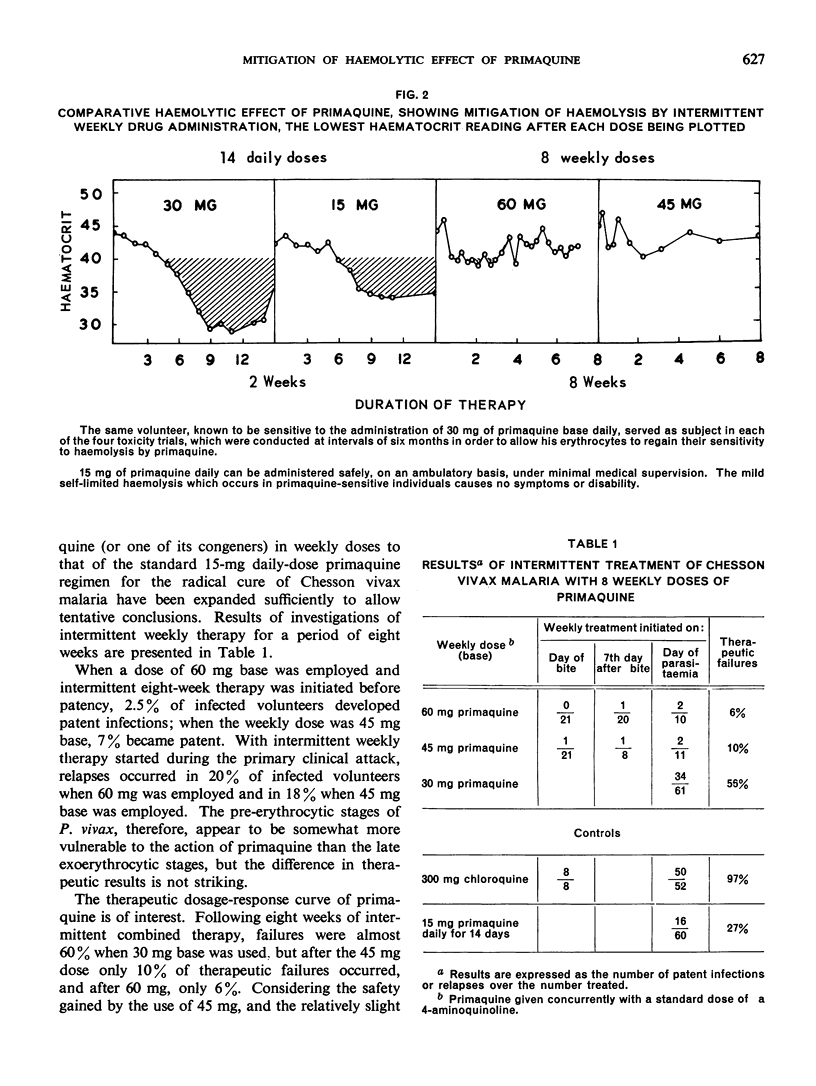
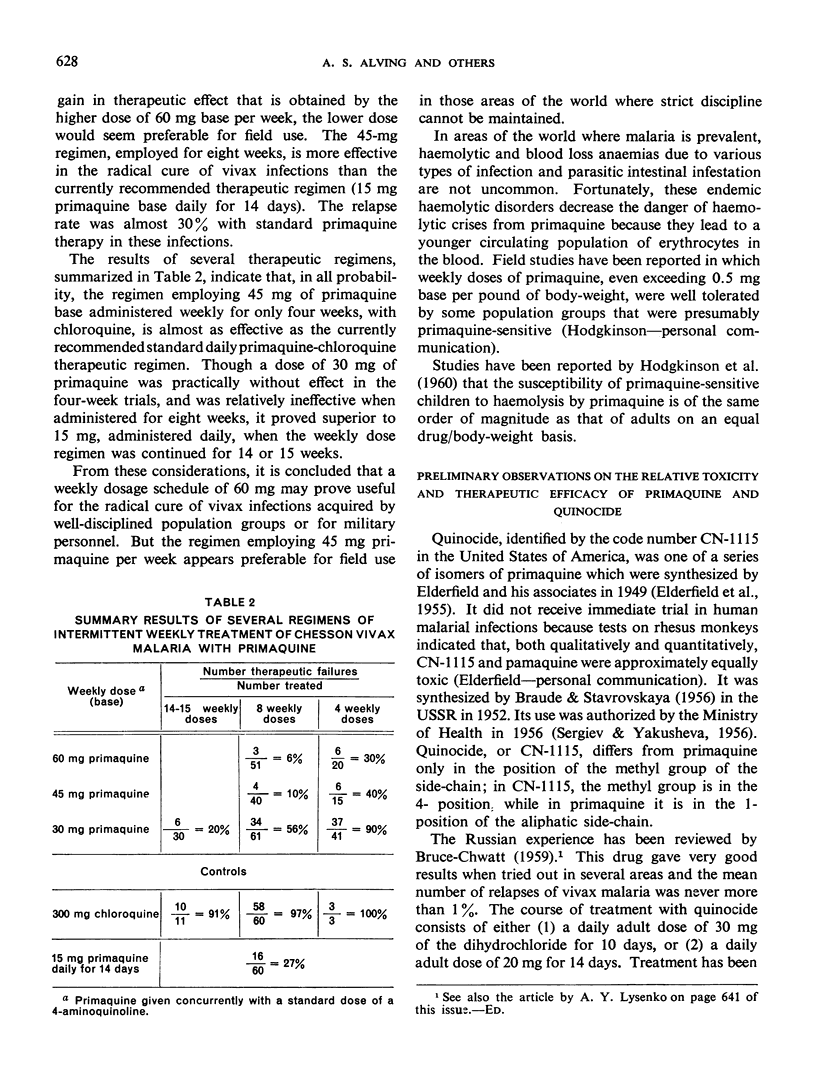
Therapeutic studies reported in the present paper indicate that the toxicity is markedly diminished by regimens requiring administration in weekly doses (together with the standard suppressive dose of chloroquine or one of its congeners) while its therapeutic effectiveness in the radical cure of Chesson vivax malaria is increased.
A weekly dose of 45 mg primaquine proved highly effective against severe Chesson vivax infections when administered for eight weeks. It cured 90% of infections, yet did not produce clinically demonstrable haemolysis in primaquine-sensitive adult males with major expression of the haemolytic trait.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ALVING A. S., ARNOLD J., HOCKWALD R. S., CLAYMAN C. B., DERN R. J., BEUTLER E., FLANAGAN C. L. Potentiation of the curative action of primaquine in vivax malaria by quinine and chloroquine. J Lab Clin Med. 1955 Aug;46(2):301–306. [PubMed] [Google Scholar]
- ALVING A. S., ARNOLD J., ROBINSON D. H. Mass therapy of subclinical vivax malaria with primaquine. J Am Med Assoc. 1952 Aug 23;149(17):1558–1562. doi: 10.1001/jama.1952.72930340017010. [DOI] [PubMed] [Google Scholar]
- ALVING A. S., CARSON P. E., FLANAGAN C. L., ICKES C. E. Enzymatic deficiency in primaquine-sensitive erythrocytes. Science. 1956 Sep 14;124(3220):484–485. doi: 10.1126/science.124.3220.484-a. [DOI] [PubMed] [Google Scholar]
- ALVING A. S., HANKEY D. D., COATNEY G. R., JONES R., Jr, COKER W. G., GARRISON P. L., DONOVAN W. N. Korean vivax malaria. II. Curative treatment with pamaquine and primaquine. Am J Trop Med Hyg. 1953 Nov;2(6):970–976. [PubMed] [Google Scholar]
- ALVING A. S., KELLERMEYER R. W., TARLOV A., SCHRIER S., CARSON P. E. Biochemical and genetic aspects of primaquine-sensitive hemolytic anemia. Ann Intern Med. 1958 Aug;49(2):240–248. doi: 10.7326/0003-4819-49-2-240. [DOI] [PubMed] [Google Scholar]
- ARCHAMBEAULT C. P. Mass antimalarial therapy in veterans returning from Korea. J Am Med Assoc. 1954 Apr 24;154(17):1411–1415. doi: 10.1001/jama.1954.02940510011005. [DOI] [PubMed] [Google Scholar]
- ARNOLD J., ALVING A. S., HOCKWALD R. S., CLAYMAN C. B., DERN R. J., BEUTLER E., FLANAGAN C. L., JEFFERY G. M. The antimalarial action of primaquine against the blood and tissue stages of falciparum malaria (Panama, P-F-6 strain). J Lab Clin Med. 1955 Sep;46(3):391–397. [PubMed] [Google Scholar]
- ARNOLD J., ALVING A. S., HOCKWALD R. S., CLAYMAN C. B., DERN R. J., BEUTLER E., JEFFERY G. M. The effect of continuous and intermittent primaquine therapy on the relapse rate of Chesson strain vivax malaria. J Lab Clin Med. 1954 Sep;44(3):429–438. [PubMed] [Google Scholar]
- ARNOLD J., ALVING A. S., HOCKWALD R. S., CLAYMAN C. B., DERN R. J., BEUTLER E., JEFFERY G. M. The effect of continuous and intermittent primaquine therapy on the relapse rate of Chesson strain vivax malaria. J Lab Clin Med. 1954 Sep;44(3):429–438. [PubMed] [Google Scholar]
- BEUTLER E., DERN R. J., ALVING A. S. The hemolytic effect of primaquine. III. A study of primaquine-sensitive erythrocytes. J Lab Clin Med. 1954 Aug;44(2):177–184. [PubMed] [Google Scholar]
- BEUTLER E., DERN R. J., FLANAGAN C. L., ALVING A. S. The hemolytic effect of primaquine. VII. Biochemical studies of drug-sensitive erythrocytes. J Lab Clin Med. 1955 Feb;45(2):286–295. [PubMed] [Google Scholar]
- BRODIE B. B., GILLETTE J. R., LA DU B. N. Enzymatic metabolism of drugs and other foreign compounds. Annu Rev Biochem. 1958;27(3):427–454. doi: 10.1146/annurev.bi.27.070158.002235. [DOI] [PubMed] [Google Scholar]
- BRUCE-CHWATT L. J. Malaria research and eradication in the USSR. A review of Soviet achievements in the field of malariology. Bull World Health Organ. 1959;21:737–772. [PMC free article] [PubMed] [Google Scholar]
- CHILDS B., ZINKHAM W., BROWNE E. A., KIMBRO E. L., TORBERT J. V. A genetic study of a defect in glutathione metabolism of the erythrocyte. Bull Johns Hopkins Hosp. 1958 Jan;102(1):21–37. [PubMed] [Google Scholar]
- COOPER W. C., MYATT A. V., HERNANDEZ T., JEFFERY G. M., COATNEY G. R. Studies in human malaria. XXXI. Comparison of primaquine, isopentaquine, SN-3883, and pamaquine as curative agents against Chesson strain vivax malaria. Am J Trop Med Hyg. 1953 Nov;2(6):949–957. [PubMed] [Google Scholar]
- DERN R. J., BEUTLER E., ALVING A. S. The hemolytic effect of primaquine. V. Primaquine sensitivity as a manifestation of a multiple drug sensitivity. J Lab Clin Med. 1955 Jan;45(1):30–39. [PubMed] [Google Scholar]
- DERN R. J., WEINSTEIN I. M., LEROY G. V., TALMAGE D. W., ALVING A. S. The hemolytic effect of primaquine. I. The localization of the drug-induced hemolytic defect in primaquine-sensitive individuals. J Lab Clin Med. 1954 Feb;43(2):303–309. [PubMed] [Google Scholar]
- DESFORGES J. F., THAYER W. W., DAWSON J. P. Hemolytic anemia induced by sulfoxone therapy, with investigations into the mechanisms of its production. Am J Med. 1959 Jul;27(1):132–136. doi: 10.1016/0002-9343(59)90067-1. [DOI] [PubMed] [Google Scholar]
- EDGCOMB J. H., ARNOLD J., YOUNT E. H., Jr, ALVING A. S., EICHELBERGER L., JEFFERY G. M., EYLES D., YOUNG M. D. Primaquine, SN 13272, a new curative agent in vivax malaria; a preliminary report. J Natl Malar Soc. 1950 Dec;9(4):285–292. [PubMed] [Google Scholar]
- FLANAGAN C. L., SCHRIER S. L., CARSON P. E., ALVING A. S. The hemolytic effect of primaquine. VIII. The effect of drug administration on parameters of primaquine sensitivity. J Lab Clin Med. 1958 Apr;51(4):600–608. [PubMed] [Google Scholar]
- GROSS R. T., HURWITZ R. E., MARKS P. A. An hereditary enzymatic defect in erythrocyte metabolism: glucose-6-phosphage dehydrogenase deficiency. J Clin Invest. 1958 Aug;37(8):1176–1184. doi: 10.1172/JCI103707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HOCKWALD R. S., ARNOLD J., CLAYMAN C. B., ALVING A. S. Toxicity of primaquine in Negroes. J Am Med Assoc. 1952 Aug 23;149(17):1568–1570. doi: 10.1001/jama.1952.72930340027010c. [DOI] [PubMed] [Google Scholar]
- KIRKMAN H. N. Charasteristics of glucose-6-phosphate dehydrogenase from normal and primaquine-sensitive erythrocytes. Nature. 1959 Oct 24;184:1291–1292. doi: 10.1038/1841291a0. [DOI] [PubMed] [Google Scholar]
- LARIZZA P., BRUNETTI P., GRIGNANI F., VENTURA S. L'individualità bio-enzimatica dell'eritrocito fabico; sopra alcune anomalie biochimiche ed enzimatiche delle emazie nei pazienti affetti da favismo e nei loro familiari. Haematologica. 1958;43(3):205–250. [PubMed] [Google Scholar]
- MARKS P. A., GROSS R. T. Erythrocyte glucose-6-phosphate dehydrogenase deficiency: evidence of differences between Negroes and Caucasians with respect to this genetically determined trait. J Clin Invest. 1959 Dec;38:2253–2262. doi: 10.1172/JCI104006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SANSONE G., SEGNI G. Nuovi aspetti dell'alterato biochimismo degli eritrociti di favici: assenza pressochè completa della glucoso-6-P deldrogenasi. Boll Soc Ital Biol Sper. 1958 Apr 15;34(7):327–329. [PubMed] [Google Scholar]
- SCHRIER S. L., KELLERMEYER R. W., CARSON P. E., ICKES C. E., ALVING A. S. The hemolytic effect of primaquine. IX. Enzymatic abnormalities in primaquine-sensitive erythrocytes. J Lab Clin Med. 1958 Jul;52(1):109–117. [PubMed] [Google Scholar]
- SCHRIER S. L., KELLERMEYER R. W., CARSON P. E., ICKES C. E., ALVING A. S. The hemolytic effect of primaquine. X. Aldolase and glyceraldehyde-3-phosphate dehydrogenase activity in primaquine-sensitive erythrocytes. J Lab Clin Med. 1959 Aug;54:232–240. [PubMed] [Google Scholar]
- SZEINBERG A., ASHER Y., SHEBA C. Studies on glutathione stability in erythrocytes of cases with past history of favism or sulfa-drug-induced hemolysis. Blood. 1958 Apr;13(4):348–358. [PubMed] [Google Scholar]
- SZEINBERG A., SHEBA C., ADAM A. Enzymatic abnormality in erythrocytes of a population sensitive to Vicia faba or haemolytic anemia induced by drugs. Nature. 1958 May 3;181(4618):1256–1256. doi: 10.1038/1811256a0. [DOI] [PubMed] [Google Scholar]
- SZEINBERG A., SHEBA C., ADAM A. Selective occurrence of glutathione instability in red blood corpuscles of the various Jewish tribes. Blood. 1958 Nov;13(11):1043–1053. [PubMed] [Google Scholar]
- ZINKHAM W. H., LENHARD R. E., Jr, CHILDS B. A deficiency of glucose-6-phosphate dehydrogenase activity in erythrocytes from patients with favism. Bull Johns Hopkins Hosp. 1958 Apr;102(4):169–175. [PubMed] [Google Scholar]
- ZINKHAM W. H., LENHARD R. E., Jr Metabolic abnormalities of erythrocytes from patients with congenital nonspherocytic hemolytic anemia. J Pediatr. 1959 Sep;55:319–336. doi: 10.1016/s0022-3476(59)80228-6. [DOI] [PubMed] [Google Scholar]



