Abstract
Muscular complications are uncommon but have been reported after radiofrequency (RF) ablation of renal tumors. Ablation of renal lesions near the psoas muscle may result in paresthesia in the distribution of the genitofemoral nerve. The present report describes a case of sensory and muscular dysfunction after RF ablation of a renal lesion lying on top of the psoas muscle that was treated without hydrodissection. To prevent this complication, hydrodissection was effectively used in two other patients during RF ablation of lesions abutting or in close proximity to the psoas muscle.
Effective targeting of renal lesions during radiofrequency (RF) ablation may require patient positioning to move the lesion of interest away from adjacent structures such as bowel or ureter to allow complete treatment of the lesion without collateral injury. Positioning may not allow safe access and targeting of some lesions, and additional maneuvers may be required to protect injury to nearby structures. Various techniques have been used for this purpose, including hydrodissection, gas instillation, and balloon instillation (1,2). Hydrodissection may provide a means to protect adjacent organs.
CASE REPORT
A 34-year-old woman with von Hippel–Lindau disease underwent percutaneous RF ablation of a 3-cm posterior left renal lesion adjacent to the psoas muscle (Fig 1) with use of a single perfused electrode probe with a 200-W generator with impedance-controlled feedback (Cool-tip; Valleylab, Boulder, CO). After the procedure, the patient reported paresthesia of the left groin area and isolated difficulty with flexion of the thigh. The patient had no motor deficit at the knee or in extension of the thigh. On 3-month follow-up, the patient reported complete recovery of thigh flexion and left groin paresthesia with no permanent sequelae. The patient had not undergone any specific therapy.
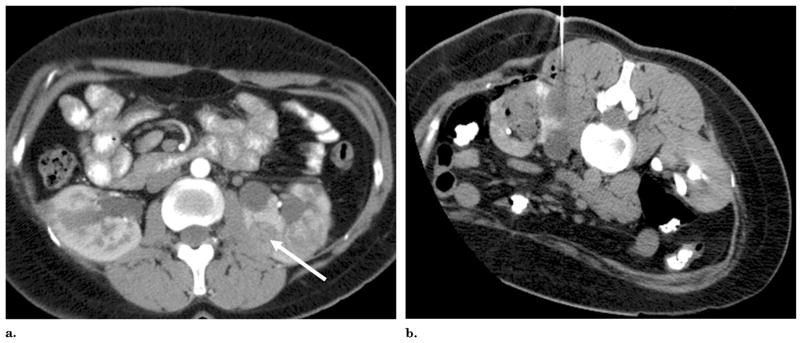
Figure 1.
(a) CT scan before RF ablation shows left renal mass (arrow) abutting psoas muscle. (b) CT of left renal mass after RF ablation on the day of treatment without hydrodissection, resulting in muscular deficit and transient weakness with hip flexion.
In subsequent cases of RF ablation of renal lesions abutting the psoas muscle, hydrodissection was used to move the renal lesion away from the psoas muscle before RF ablation. A 32-year-old man with von Hippel–Lindau disease underwent percutaneous RF ablation of a left posterior renal lesion with retroperitoneal instillation of 350 mL of 5% dextrose in water via a 20-gauge Chiba needle under direct ultrasound (US) visualization with computed tomography (CT) confirmation of kidney displacement (Fig 2). The patient reported no motor or sensory deficits after the RF ablation procedure.
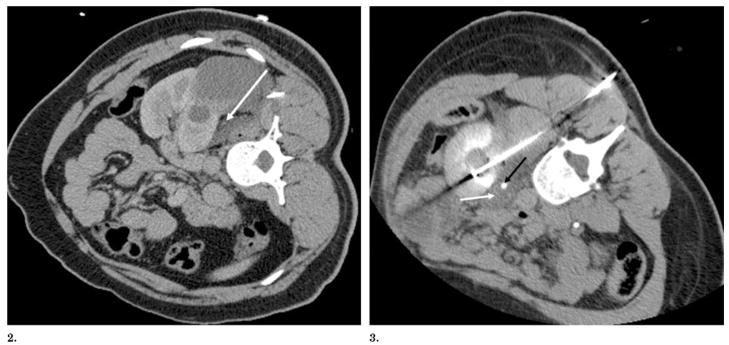
Figure 2.
Figures 2, 3. (2) CT after hydrodissection and before RF ablation shows left kidney displaced from psoas muscle with decubitus positioning and percutaneous instillation of 350 mL of 5% dextrose in water (arrow). (3) CT scan during RF ablation shows a left renal mass abutting the psoas muscle after instillation of 5% dextrose in water (white arrow) into the retroperitoneum, with the patient in a near-prone position. The ureter is seen medial to the kidney (black arrow) and is also protected by a fluid pocket.
In another case, a 36-year-old woman with von Hippel–Lindau disease underwent percutaneous RF ablation of a left posterior kidney lesion with hydrodissection with 115 mL of 5% dextrose in water under CT and US guidance to displace and protect the nearby psoas muscle and ureter from injury (Fig 3). This patient experienced no motor or sensory sequelae after the RF ablation procedure.
All patients were treated with a 200-W, 480-kHz cooled-tip monopolar generator (Valleylab). All tumors were between 2.2 cm and 2.5 cm in diameter. The ablation endpoint was 12 minutes according to the manufacturer’s recommendations. Each patient underwent one ablation session with variable overlapping ablations per patient (1.5 for patient 1, two for patients 2 and 3; one ablation for 12 minutes in one location). All patients were seen before discharge 1 day after RF ablation and in the clinic 3 months, 6 months, and 12 months afterward.
DISCUSSION
Minimally invasive ablative therapies such as RF ablation, cryotherapy, microwave ablation, and high-intensity focused US are more commonly being used for treatment of small renal lesions. Although published long-term results are sparse, the nephron-sparing nature of the techniques offers decreased morbidity and invasiveness. Successful treatment with such techniques is predicated on effective targeting. Nearby structures can alter the risk profile related to potential collateral thermal injury. Ways to avoid potential complications of these minimally invasive techniques are being clarified as more experience is gained. A multi-institutional review of complications of RF ablation and cryotherapy (3) identified pain or paresthesia at the probe site as the most frequent minor complication, which resolves in the majority of cases with no sequelae. More uncommonly, flank wall weakness or laxity is reported subsequent to RF ablation (4). Others have described the prevention of injury to the genitofemoral nerve during RF ablation of medial kidney tumors by use of a “lever technique” to move the kidney away from the psoas muscle (5). Tumors with exophytic or cortical components in the medial or posterior location could increase the risk of injury to the muscle or nerve. However, the exact incidence and risk profiles are unknown.
In summary, we present a case of muscular complication of RF ablation that likely resulted from close proximity of the ablated lesion to the psoas muscle and two cases in which hydro-dissection was subsequently used to displace the lesion away from the adjacent psoas muscle with no subsequent neurologic or muscular deficit reported. Further studies are needed to validate the safety and efficacy of this maneuver.
Hydrodissection may present an effective means to prevent collateral injury to nearby structures when simple patient positioning does not displace adjacent sensitive structures. Although it is described for protecting the bowel, this technique may also prove to prevent muscular or nerve injury in lesions abutting the psoas muscle or retroperitoneal nerves.
Acknowledgments
This research was supported in part by the Intramural Research Program of the National Institutes of Health. None of the authors have identified a conflict of interest.
Abbreviation
- RF
radiofrequency
References
- 1.Farrell MA, Charboneau JW, Callstrom MR, et al. Paranephric water instillation: a technique to prevent bowel injury during percutaneous renal radio frequency ablation. Am J Roentgenol. 2003;181:1315–1317. doi: 10.2214/ajr.181.5.1811315. [DOI] [PubMed] [Google Scholar]
- 2.Kam AW, Littrup PJ, Walther MM, et al. Thermal protection during percutaneous thermal ablation of renal cell carcinoma. J Vasc Interv Radiol. 2004;15:753–758. doi: 10.1097/01.rvi.0000133535.16753.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson DB, Solomon SB, Su LM, et al. Defining the complications of cryoablation and radio frequency ablation of small renal tumors: a multi-institutional review. J Urol. 2004;172:874–87. doi: 10.1097/01.ju.0000135833.67906.ec. [DOI] [PubMed] [Google Scholar]
- 4.Bhayani SB, Allaf ME, Su LM, et al. Neuromuscular complications after percutaneous radiofrequency ablation of renal tumors. Urology. 2005;65:592. doi: 10.1016/j.urology.2004.09.053. [DOI] [PubMed] [Google Scholar]
- 5.Boss A, Clasen S, Kuczyk M, et al. Thermal damage of the genitofemoral nerve due to radiofrequency ablation of renal cell carcinoma: a potentially avoidable complication. Am J Roentgenol. 2005;185:1627–1631. doi: 10.2214/AJR.04.1946. [DOI] [PubMed] [Google Scholar]