Abstract
Liquid and solid foods are documented to elicit differential appetitive and food intake responses. This study was designed to assess the influences of liquid vs solid meal replacement products on postprandial appetite ratings and subsequent food intake in healthy older adults. This study used a randomized and crossover design with two 1-day trials (1 week between trials), and 24 adults (12 men and 12 women) aged 50 to 80 years with body mass index (calculated as kg/m2) between 22 and 30 participated. After an overnight fast, the subjects consumed meal replacement products as either a beverage (liquid) or a bar (solid). The meal replacement products provided 25% of each subject's daily estimated energy needs with comparable macro-nutrient compositions. Subjects rated their appetite on a 100 mm quasilogarithmic visual analog scale before and 15, 30, 45, 60, 90, 120, and 150 minutes after consuming the meal replacement product. At minute 120, each subject consumed cooked oatmeal ad libitum to a “comfortable level of fullness.” Postprandial composite (area under the curve from minute 15 to minute 120) hunger was higher (P=0.04) for the liquid vs solid meal replacement products and desire to eat (P=0.15), preoccupation with thoughts of food (P=0.07), and fullness (P=0.25) did not differ for the liquid vs solid meal replacement products. On average, the subjects consumed 13.4% more oatmeal after the liquid vs solid (P=0.006) meal replacement product. These results indicate that meal replacement products in liquid and solid form do not elicit comparable appetitive and ingestive behavior responses and that meal replacement products in liquid form blunt the postprandial decline in hunger and increase subsequent food intake in older adults.
The physical form of food (eg, liquid vs solid) influences energy balance and body weight (1). Liquids have been reported to elicit stronger feelings of hunger (2-5) (ie, weaker appetitive response) than solids or no difference (1,6,7). Most (1,7,8), but not all (6) studies indicate that dietary compensation (ie, a reduction in subsequent energy intake to offset the amount of energy contained in a test food) did not occur when energy was consumed in liquid form and subsequent energy intake and body weight increased. Although aging influences appetite and energy intake (9), the majority of research evaluating the effects of energy in liquid vs solid foods on appetite and ingestive behavior has been conducted in young and middle-aged persons (1-4,6-8). Limited data collected in older adults (5) supports the notion that liquid-based energy elicits weaker appetitive responses.
Meal replacement products represent commercially available foods that are manufactured in liquid and solid forms. Liquid and solid meal replacement products are marketed to adults of all ages who desire help with weight loss, weight gain, weight management, or overall general health. The liquid and solid meal replacement products are sold with the implied understanding of comparable appetitive (appetite ratings) and ingestive behavior responses. The purpose of this study was to compare the effects of liquid vs solid meal replacement products on acute postprandial ratings of appetite and subsequent food intake in healthy older adults. We hypothesized that postprandial hunger, desire to eat, and preoccupation with thoughts of food would be higher, and fullness lower, after liquid meal replacement products were consumed. Also, subsequent food intake would be greater after the liquid meal replacement product.
Methods
Subjects
Thirty-six individuals living in the greater Lafayette, IN, community were recruited using newspaper advertisements. Participant eligibility included: age 50 to 80 years; body mass index 22 to 30 (calculated as kg/m2); nondia-betic; clinically normal kidney, liver, and cardiac functions; not currently taking any medications or supplements known to influence appetite; and for women, at least 2 years postmenopausal. Prestudy, each subject completed a self-reported medical history questionnaire, was approved by the study physician, and provided informed consent. The study was approved by Purdue University's Institutional Review Board and the subjects received monetary compensation for participating.
Data from 24 (12 men and 12 women) older (age 62±2 years) adults with a body mass index of 26.0±0.8 were included in the analyses. Data from 12 participants were excluded for the following reasons: schedule conflicts (one subject); inability to tolerate or consume the meal replacement products or oatmeal (three subjects); consumed all of the oatmeal, which prevented us from quantifying any intervention-related differences in food intake (three subjects); witnesses to another subject's intolerance to the meal replacement products, which could have influenced their own responses to the interventions (three subjects); and outliers (based on Box and Whisker plot, ±3 standard deviations of food intake and appetite ratings, two subjects). Twenty-four subjects permitted us to detect treatment effects equal to a standardized difference of 0.4 at the 5% probability level with approximately 90% power.
Experimental Design
A within-subject design was used with each subject completing 2 days of testing in random order separated by 1 week. At approximately 0700 hours (10-hour fasting state) the participants reported to the laboratory, were seated in a secluded area without communication with the other participants, and consumed within 15 minutes either a liquid meal replacement product (served at 4°C to 6°C in a large opaque mug with a lid) or a solid meal replacement product (served at 22°C to 25°C on a plate after being cut into bite-size pieces to equalize the visual presentation of the bars among the subjects), plus 237 g (8 oz) water to alleviate thirst.
Two hours after consuming the meal replacement product (Minute 120), the subjects were provided a bowl of cooked, hot oatmeal (76°C at the time of serving) and asked to consume it ad libitum to a “comfortable level of fullness.” The 120-minute time point corresponded with a time when postprandial hunger was rising, but still below the fasting level. Each bowl contained the following ingredients: rolled oats (120 g dry weight), 2% reduced-fat milk (75 g), brown sugar (24 g), salt (1 g), and water (550 g), which represented three commercial servings. The total amount of oatmeal consumed was quantified (±0.1 g) by weighing the bowl before and after the subject ate (digital scale SB 8001, Mettler-Toledo International Inc, Columbus, OH). The oatmeal texture (ie, semisolid; viscosity 16,200 cps, and hardness 0.8 g) was between the liquid meal replacement product (viscosity 38 cps) and solid meal replacement product (hardness 1,064 g).
Meal Replacement Products
The liquid and solid meal replacement products (preload) were vanilla Ensure Complete Balanced Nutrition beverage and Ensure Cinnamon Oat'n Raisin nutrition and energy bar (Ross Products Division, Abbott Laboratories Inc, Columbus, OH). They contained comparable energy and macronutrients (see the Table) obtained from the Nutrition Facts labels. The meal replacement product preloads were portioned to provide 25% of each subject's daily energy need (estimated using the sex-specific Harris-Benedict equation [10]) and a physical activity level factor of 1.5 (sedentary) (11). These portions resulted in each person consuming two to two and a half servings of the meal replacement product.
Table.
Mean weight, energy density, energy content, and macronutrient content of the liquid and solid meal replacement products consumed by older adults in a study of postprandial appetite ratings
| Property | Liquid meal replacement producta | Solid meal replacement productb |
|---|---|---|
| Weight (g)c | 572±21 | 146±5 |
| Energy density (kcal/g) | 0.98 | 3.83 |
| Energy (kcal)c | 559±20 | 559±20 |
| Carbohydrate (g)c | 89±3 | 86±3 |
| Fiber (g) | 0 | 5±0.2 |
| Fat (g)c | 13±0 | 15±1 |
| Protein (g)c | 21±1 | 24±1 |
Ingredients (from highest to lowest content in the liquid meal replacement product; quantities not provided on the manufacturer's label): water, sugar, corn syrup, maltodextrin (corn), calcium caseinate, high-oleic safflower oil, canola oil, soy protein isolate, whey protein concentrate, and corn oil (also 32 vitamins and mineral compounds).
Ingredients (from highest to lowest content in the solid meal replacement product; quantities not provided on the manufacturer's label): yogurt coating, high-fructose corn syrup, soy protein isolate, raisins, honey, crisp rice, toasted rolled oats, fructose, maltodextrin, fructooligosaccharides, whey protein concentrate, glycerone, guar gum, calcium caseinate, high-oleic sunflower oil, high-oleic safflower oil (also 26 vitamins and mineral compounds).
Data expressed as mean±standard error of the mean.
Appetite Assessment
Appetite was assessed immediately before (minute 0), then 15, 30, 45, 60, 90, and 120 minutes after the meal replacement product was consumed, and 30 minutes after eating the oatmeal (minute 150). Perceived hunger, feeling of fullness, desire to eat, and preoccupation with thoughts of food were rated on a 100 mm quasilogarith-mic visual analog scale, which is a valid and reliable tool (12). The vertical axis end descriptors were “barely detectable (2 mm)” and “strongest imaginable (100 mm),” and the intermediate descriptors were “weak (6 mm),” “moderate (17 mm),” “strong (34 mm),” and “very strong (53 mm).” The subject was asked to make a horizontal mark through the vertical axis that best matched how they felt at the time. From minute 15 to minute 120, the postprandial area under the curve (AUC) was calculated by the trapezoidal method (13).
Diversionary Task
To minimize the potential for biased responding, subjects were informed that the intent of the study was to assess the effects of the meal replacement products on hand grip strength, which was measured five times during each testing day (data not reported).
Statistical Analysis
Statistical analyses were performed with the Statistical Analyses Systems software (version 9.1.3, 2002-2003, SAS Inc, Cary, NC). The AUC for each appetite rating and oatmeal consumption were assessed using repeated measure analysis of variance with meal replacement products as repeated effects in the model. A paired t test was used to assess the difference between liquid and solid before the meal replacement product was consumed (baseline, minute 0) and after the consumption of the oatmeal (minute 150). Data are reported as mean±standard error of the mean and significance was defined as P<0.05. All data were collected and entered into a Microsoft Excel (version 5.1.2600, 2003, Microsoft Corp, Redmond, WA) spreadsheet in duplicates. The spreadsheets were checked by other members of the research team to avoid transcription errors.
Results And Discussion
At minute 0 (baseline) and minute 150 (30 minutes post oatmeal), indexes of appetite were not different between liquid vs solid meal replacement products. Fifteen minutes after both meal replacement products were consumed, hunger, desire to eat, and preoccupation with thoughts of food decreased and fullness increased. During minute 15 to minute 120, these indexes of appetite gradually returned toward baseline. Hunger AUC was higher for the liquid vs solid meal replacement products (see panel A of the Figure). The AUC for desire to eat, preoccupation with thoughts of food, and fullness was not different between the liquid and solid meal replacement products (see panels B through D of the Figure). On average, subjects consumed 13.4% more oatmeal after the liquid vs solid (338±33 vs 298±32; P=0.006) meal replacement product.
Figure.
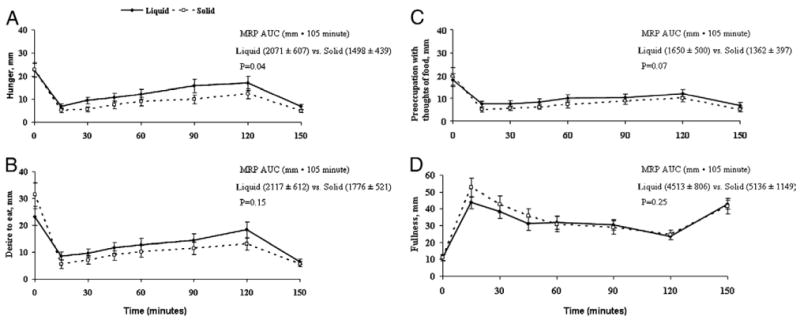
Appetite ratings area under the curve (AUC) across 105 minutes (minutes 15 to 120) in healthy older adults (N=24). Liquid or solid meal replacement products (MRP) were consumed after Minute 0 appetite ratings and oatmeal was consumed after Minute 120 appetite ratings. Appetite was assessed on a quasilogarithmic 100 mm visual analog scale.
The results of this study indicate that these older adults experienced higher postprandial hunger and consumed more food at the next eating occasion after consuming a liquid vs solid meal replacement product. The differential hunger response between the liquid and solid meal replacement product is comparable to the response our research group observed when older adults consumed other types of commercially available meal replacement products (5), and we are apparently the first to document differences in ingestive behavior in older people. This underscores the importance of the physical form of food as an effecter of appetite, food intake, and by inference, body weight control.
The finding of an average 13.4% higher food intake after the liquid vs solid meal replacement product supports our hypothesis. These results also support research by Mourao and colleagues (7) who reported that lean and obese, young to middle-aged men and women consumed 12%, 19%, and 15% more total energy on days when they consumed portioned quantities of high-carbohydrate, high-fat, and high-protein foods, respectively, in liquid vs solid form (7). Dietary compensation was not evaluated in our study. However, a meta-analysis of 42 studies found that dietary compensation was not observed after liquids were ingested, whereas a modest adjustment in free-feeding intake was observed for semi-solids, and a stronger compensation response was noted for solids (8). Similarly, more recent research (1) showed that a liquid preload elicited a weaker dietary compensation response than the solid preload and increased body weight, body mass index, and energy intake. In contrast, another study found that postprandial hunger was not different when subjects consumed such food items as regular cola (liquid) vs cookies (solid) (6). Dietary compensation was not evaluated and differences in nutrient composition and not requiring the subject to fast initially might have confounded this assessment (6). Collectively, these results suggest that beverages are more likely to promote a positive energy balance than solid food.
There are a number of reasons for the differential responses between the liquid and solid meal replacement products in this study. Mastication of the solid could have provided a satiety signal not triggered by swallowing the liquids (3). The subjects might have perceived that solid foods contain more energy and have greater satiation and satiety properties than a liquid (14). Liquids have been documented to have a more rapid gastrointestinal transit time than solids, which can result in a different time course of nutrient exposure to purported nutrient sensors in the gut or proximal duodenum with possible implications for appetite and meal initiation (15,16). Energy density of food, a characteristic difference between liquids and solids of the same energy content, can influence appetite and food intake (17). Our results would support this statement because the liquid meal replacement product was less energy dense than the solid meal replacement product with similar energy content.
We consider strengths of this study to include the controlled environmental and experimental conditions and continuous supervision maintained in the laboratory setting while appetite and food intake responses were quantified, the use of diversionary activities to mask the actual research objective, and the use of commercially available products. A limitation of our study is the lack of stratification by sex and age. The modest differences in ingredients between the liquid and solid products might be considered a weakness. The solid meal replacement product contained rolled oats and the subjects might have reduced their subsequent oatmeal intake due to being tired of the taste and texture of rolled oats. The participants were not informed that the solid meal replacement product contained rolled oats and the rolled oats were not visibly in their whole form. Some may view having different fiber contents in the liquid and solid meal replacement product as a limitation. Studies have shown that fiber does not affect appetite (18,19). A previous study observed greater postprandial hunger in older people who consumed liquid vs solid meal replacement products when the liquid meal replacement product had a higher fiber content (5). Some may view not including a trial without a preload as a limitation, but the focus of this study was to measure intake after the preload and not dietary compensation.
Conclusions
Meal replacement products are manufactured in liquid and solid forms and are often sold and purchased without regard to whether the form of the product influences appetite and ingestive behavior. The results from this study challenge these assumptions. The primary findings that the ingestion of a meal replacement product in liquid form elicited a blunted postprandial decline in hunger and an average of 13.4% higher food intake at the next eating occasion demonstrate that the physical form of food influences appetite and ingestive behavior. It is important that health care providers find suitable dietary strategies to help older individuals decrease or increase their energy intake to achieve desired nutrition goals and to maintain or re-establish proper nutritional status. With regard to body weight control, older individuals who are underweight might benefit more from consuming liquid meal replacement products and those individuals who are overweight might benefit more from consuming solid meal replacement products.
Acknowledgments
This study was supported by National Institutes of Health grant no. R01 AG021911, National Institutes of Health diversity supplement to National Institutes of Health R01 grant; the Agricultural Research Program, Lynn and Graduate School Fellowships at Purdue University; and the American Egg Board Egg Nutrition Center.
The authors thank the volunteers who participated in this study, Arthur Rosen, MD, for providing medical coverage, and Andreana Robertson for help with statistical analyses.
Footnotes
These data were originally presented as an abstract at the Experimental Biology Conference, San Diego, CA, April 2-6, 2005.
References
- 1.DiMeglio DP, Mattes RD. Liquid vs solid carbohydrate: Effects on food intake and body weight. Int J Obes Relat Metab Disord. 2000;24:794–800. doi: 10.1038/sj.ijo.0801229. [DOI] [PubMed] [Google Scholar]
- 2.Bolton RP, Heaton KW, Burroughs LF. The role of dietary fiber in satiety, glucose, and insulin: Studies with fruit and fruit juice. Am J Clin Nutr. 1981;34:211–217. doi: 10.1093/ajcn/34.2.211. [DOI] [PubMed] [Google Scholar]
- 3.Haber GB, Heaton KW, Murphy D, Burroughs LF. Depletion and disruption of dietary fibre. Effects on satiety, plasma-glucose, and serum-insulin. Lancet. 1977;2:679–682. doi: 10.1016/s0140-6736(77)90494-9. [DOI] [PubMed] [Google Scholar]
- 4.Rothacker DQ, Watemberg S. Short-term hunger intensity changes following ingestion of a meal replacement bar for weight control. Int J Food Sci Nutr. 2004;55:223–226. doi: 10.1080/09637480410001734111. [DOI] [PubMed] [Google Scholar]
- 5.Tieken SM, Leidy HJ, Stull AJ, Mattes RD, Schuster RA, Campbell WW. Effects of solid vs liquid meal-replacement products of similar energy content on hunger, satiety, and appetite-regulating hormones in older adults. Horm Metab Res. 2007;39:389–394. doi: 10.1055/s-2007-976545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Almiron-Roig E, Flores SY, Drewnowski A. No difference in satiety or in subsequent energy intakes between a beverage and a solid food. Physiol Behav. 2004;82:671–677. doi: 10.1016/j.physbeh.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Mourao DM, Bressan J, Campbell WW, Mattes RD. Effects of food form on appetite and energy intake in lean and obese young adults. Int J Obes (Lond) 2007;31:1688–1695. doi: 10.1038/sj.ijo.0803667. [DOI] [PubMed] [Google Scholar]
- 8.Mattes RD. Dietary compensation by humans for supplemental energy provided as ethanol or carbohydrate in fluids. Physiol Behav. 1996;59:179–187. doi: 10.1016/0031-9384(95)02007-1. [DOI] [PubMed] [Google Scholar]
- 9.Chapman IM, MacIntosh CG, Morley JE, Horowitz M. The anorexia of ageing. Biogerontology. 2002;3:67–71. doi: 10.1023/a:1015211530695. [DOI] [PubMed] [Google Scholar]
- 10.Harris J, B F. A Biometric Study of Basal Metabolism in Man. Washington, DC: Carnegie Institute of Washington; 1919. [Google Scholar]
- 11.Shetty PS, Henry CJ, Black AE, Prentice AM. Energy requirements of adults: An update on basal metabolic rates (BMRs) and physical activity levels (PALs) Eur J Clin Nutr. 1996;50 1:S11–S23. [PubMed] [Google Scholar]
- 12.Stubbs RJ, Hughes DA, Johnstone AM, Rowley E, Reid C, Elia M, Stratton R, Delargy H, King N, Blundell JE. The use of visual analogue scales to assess motivation to eat in human subjects: A review of their reliability and validity with an evaluation of new hand-held computerized systems for temporal tracking of appetite ratings. Br J Nutr. 2000;84:405–415. doi: 10.1017/s0007114500001719. [DOI] [PubMed] [Google Scholar]
- 13.Wolever TM, Jenkins DJ. The use of the glycemic index in predicting the blood glucose response to mixed meals. Am J Clin Nutr. 1986;43:167–72. doi: 10.1093/ajcn/43.1.167. [DOI] [PubMed] [Google Scholar]
- 14.Wooley OW, Wooley SC, Dunham RB. Can calories be perceived and do they affect hunger in obese and nonobese humans? J Comp Physiol Psychol. 1972;80:250–258. doi: 10.1037/h0033069. [DOI] [PubMed] [Google Scholar]
- 15.Phillips RJ, Powley TL. Gastric volume rather than nutrient content inhibits food intake. Am J Physiol. 1996;271(3 Pt 2):R766–R769. doi: 10.1152/ajpregu.1996.271.3.R766. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz GJ, Moran TH. Duodenal nutrient exposure elicits nutrient-specific gut motility and vagal afferent signals in rat. Am J Physiol. 1998;274(5 Pt 2):R1236–R1242. doi: 10.1152/ajpregu.1998.274.5.R1236. [DOI] [PubMed] [Google Scholar]
- 17.Bell EA, Castellanos VH, Pelkman CL, Thorwart ML, Rolls BJ. Energy density of foods affects energy intake in normal-weight women. Am J Clin Nutr. 1998;67:412–420. doi: 10.1093/ajcn/67.3.412. [DOI] [PubMed] [Google Scholar]
- 18.Frost GS, Brynes AE, Dhillo WS, Bloom SR, McBurney MI. The effects of fiber enrichment of pasta and fat content on gastric emptying, GLP-1, glucose, and insulin responses to a meal. Eur J Clin Nutr. 2003;57:293–298. doi: 10.1038/sj.ejcn.1601520. [DOI] [PubMed] [Google Scholar]
- 19.Heini AF, Lara-Castro C, Schneider H, Kirk KA, Considine RV, Weinsier RL. Effect of hydrolyzed guar fiber on fasting and postprandial satiety and satiety hormones: A double-blind, placebo-controlled trial during controlled weight loss. Int J Obes Relat Metab Disord. 1998;22:906–909. doi: 10.1038/sj.ijo.0800680. [DOI] [PubMed] [Google Scholar]


