Abstract
Purpose
To study the architecture of clear corneal incisions for phacoemulsification cataract surgery using optical coherence tomography (OCT).
Setting
University-based cornea practice.
Methods
A prospective study of twenty eyes of twenty patients one month after cataract surgery performed by two experienced surgeons. Temporal clear corneal single-plane incisions were made with 3-mm metal keratomes; five of the twenty eyes received sutures for wound closure. Each eye was scanned before and 1 month after surgery with a prototype high-speed anterior segment OCT system (Carl Zeiss Meditec Inc.). The OCT scans were repeated 3 times during the same visit. The length of the corneal incision, thickness of the cornea, and position of the incision (distance from the external wound edge to the scleral spur) were measured using a computer caliper. The angle of the incision relative to the corneal surface was then calculated.
Results
The mean corneal incision length was 1.81±0.27mm, the mean corneal thickness at the incision was 747±67µm, and the mean distance between the incision and the scleral spur was 1.46±0.24mm. The average angle of the incision was 26.8±5.5°. The measurements were repeatable to within 0.072mm (pooled standard deviation) for the incision length, 11µm for the corneal thickness, and 0.042mm for the position of the incision. There was no statistically significant difference in any of the parameters between eyes with sutures and those without.
Conclusions
OCT provides an excellent way to evaluate corneal incisions in cataract surgery postoperatively. Measurements of wound dimensions using OCT are highly repeatable.
Introduction
Self sealing temporal clear corneal incisions are commonly used in cataract surgery because of the ease of construction and lack of bleeding. However, concerns for a potential increased risk of endophthalmitis as compared to scleral tunnel incisions have lingered.1–3 The self-sealing behavior of the wound is important as a barrier against intraocular infection. Several studies have attempted to correlate the dimensions of clear corneal incisions to functional wound sealing behavior.4–6 These studies have found that the dimensions of the wound and the angle of the incision are correlated to the self-sealing behavior of clear corneal incisions. Some authors have also studied the morphology of clear corneal incisions after cataract surgery and observed wound distortion from foldable intraocular lens implants and post-surgical stromal swelling.7, 8
These studies provided important insight into the self-sealing properties of clear corneal incisions, but none to date have provided accurate measurement of wound length in vivo. Optical coherence tomography (OCT) offers an excellent method for this purpose by providing high resolution images of the cornea in which the cataract incision is clearly visible. In this study, we used a high speed anterior segment OCT system that was able to measure corneal dimensions without significant motion error. The goal of this study is to demonstrate precision of OCT-measured wound dimensions in cataract patients and relate them to the surgical outcomes.
Methods
Study participants were recruited from the clinical practices of coauthors DH or JCS according to a prospective study protocol approved by the institutional review board of the University of Southern California. Informed consent was obtained and documented for every participant. The study adhered to the tenets of the Declaration of Helsinki. One randomly selected eye of each participant was studied. Cataract patients with no other ocular diseases were enrolled in the study. Imaging of the cornea and the anterior segment by OCT was performed before and 1 month after the cataract surgery. Postoperative OCT scans are used in this report to study the corneal incisions.
Both surgeons performed phacoemulsification through temporal uniplanar clear corneal incisions. The incisions were made with a 3-mm metal keratome (ClearCut HP, Alcon Laboratories, Fort Worth, TX). The surgeons aimed to produce a 2-mm long incision using the etched 2-mm mark on the ClearCut blade. Phacoemulsification was performed using the Alcon Infiniti system. Lens cortex was removed by automated irrigation and aspiration using coaxial or bimanual setup, depending on the surgeon’s preference. A foldable acrylic intraocular lenses, either the single-piece Acrylof™ lens (Alcon SN60WF or SA60AT) or the Tecnis™ lens (AMO ZA9003) were injected into capsular bag using the Monarch IIB (Alcon) or Emerald-Unfolder (AMO) implantation system, without any incisional enlargement of the clear corneal tunnel. The phacoemulsification and side-port incisions were sealed with stromal hydration by balanced salt solution. The eyes were filled with balanced salt solution to normal pressure on palpation. A single interrupted 10-0 nylon suture (Ethicon) was used to close the wound if the surgeon deemed it necessary. The reason for wound suturing include wound leak upon challenge with mild pressure near the wound and/or long axial length. All wounds were watertight by the end of the procedure. If present, the sutures were removed at the 1 week postoperative visit.
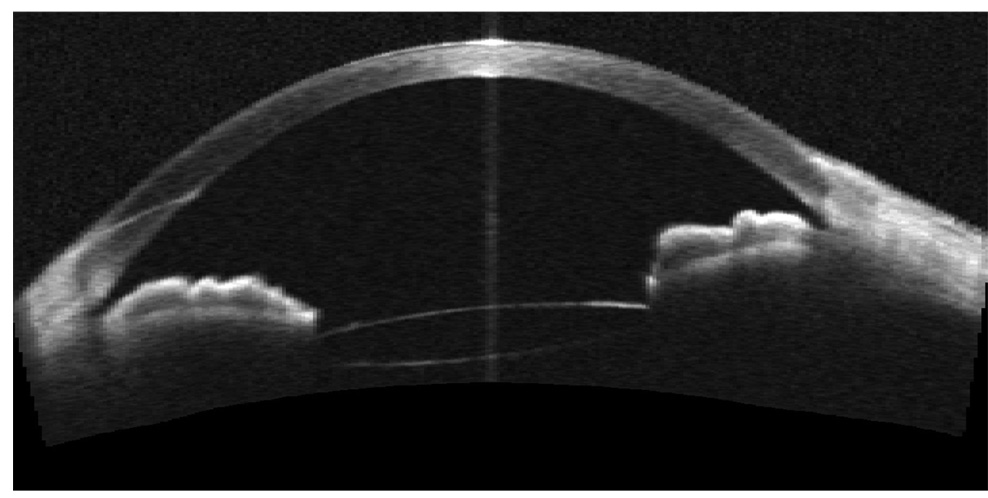
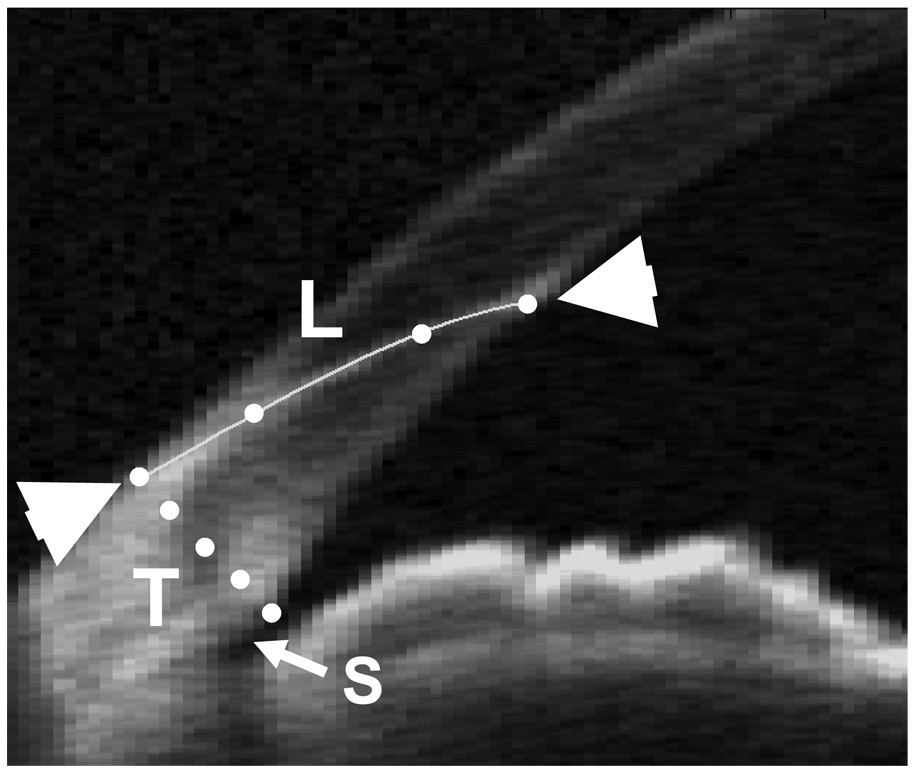
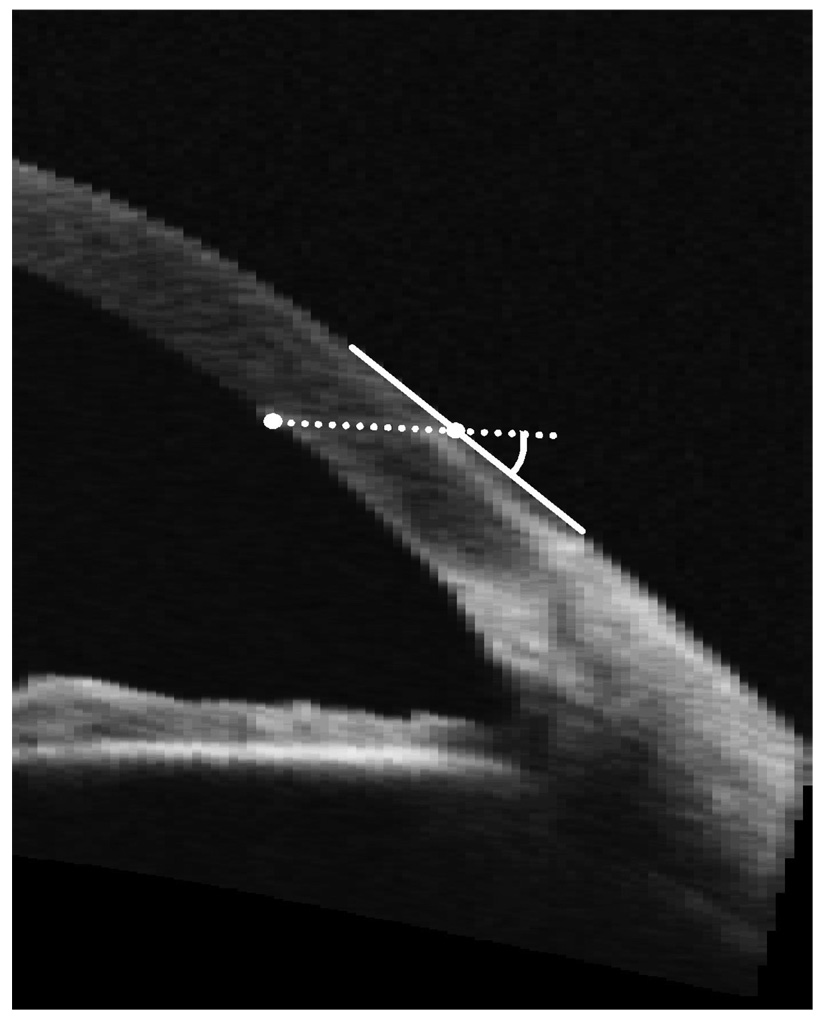
A prototype high-speed anterior segment OCT system (Carl Zeiss Meditec, Dublin, CA) was used to image the cornea 1 month after the surgery. The OCT system has been previously described.9 Briefly, it operates at 1310 nm wavelength, acquires 2000 axial scans per second, and has an axial resolution of 17 microns. The scan geometry was rectangular. Angle-to-angle (16 mm wide) horizontal OCT scans centered on the vertex were performed 3 times (Figure 1). The image depth was set to be 8mm (in air). The scan dimensions were calibrated with the tool and method as described in a previous publication.9 Since the cataract surgery incisions were located at the temporal limbus, the scans generally pass through the center of the incisions. The image distortion due to refraction and transition of the group index a the air-cornea interface was removed using a dewarping algorithm.10 Measurements of the thickness of the cornea at the external opening of the wound, and distance between the internal wound opening and the scleral spur were taken in each of the three scans using a computer caliper (Figure 2). The incision length was measured using a 4-point spline curve fitted to the wound to account for the curvature of the wound (Figure 2), the line integral of this curve was then calculated to give the length. The angle of the wound incision was measured between the corneal surface tangent at the external wound opening and the line connecting the internal and external wound openings (Figure 3).
Figure 1.
Cataract wound measurements were made on optical coherence tomography (OCT) horizontal cross-sections.
Figure 2.
The incision length was measured by a 4-point (dots) spline between the internal and external wound openings (triangles). The distance between the internal opening and the scleral spur (S) was also measured.
Figure 3.
The angle of the incision was measured between the corneal surface tangent (solid line) and the line connecting the internal and external wound openings (dotted line).
Results
Twenty participants were enrolled. A suture was used to close the wound in five of the 20 cases. No intraoperative complications were observed. No cases of hypotony, wound leak, shallow chamber or endophthalmitis were observed at the 1 day, 1 week or 1 month postoperative visits.
The average corneal thickness at the incision entry point was 747 ±67 µm (mean ± standard deviation, range: 619µm to 843µm). The average length of the incision was 1.81±0.27mm (range: 1.41mm to 2.39mm). This was significantly different from the intended length of 2.0 mm (p = 0.005). The average length of the linear approximation of the incision from external to internal opening was 1.71±0.34mm, this length was not significantly different than the curvilinear length, p=0.07.
The average angle of the incision relative to the tangent plane to the corneal surface was 26.8±5.5° (range: 22.7 ° to 37.4°). The average distance between the internal edge of the wound and the scleral spur was 1.46±0.24mm (range: 0.97mm to 1.82mm). The measurements in this study were repeatable to within 0.072mm (pooled standard deviation) for the incision length, 11µm for the corneal thickness, and 0.042mm for the position of the incision. There were no significant differences in any of the measured parameters between eyes that received sutures at time of surgery and those that did not: angle of incision p=0.14, incision length p=0.23, corneal thickness p=0.27.
Discussion
Several authors have previously studied clear corneal incision integrity and healing. Mackool and Russell studied wound leakage in relation to incision length and width in cadaver eyes under a variety of external pressure challenges.4 They concluded that wounds of greater than 2.0 mm in length and 3.0 to 3.5 mm in width as measured manually by caliper demonstrated sufficient self sealing to be comparable to the integrity of scleral tunnel incisions. Kohnen, et al, examined incision size and wound tearing from foldable intraocular lens implants through clear corneal incisions in cadaver eyes using measurement calipers and scanning electron microscopy.8 Torres, et al, used a retinal optical coherence tomography (OCT) system with adjustments to image the cornea to measure the incision angle and observe wound sealing at 1, 3, and 30 days postoperatively.6 They found no correlation between the structural integrity of the wound and the incision angle. However, the incision angle they measured was not adjusted for the sector-scan geometry and refractive index transition at the air-corneal boundary. Taban, et al, used OCT to observe wound gaping immediately after surgery in enucleated human and rabbit eyes under conditions of varying intraocular pressure (IOP) and angles of the incision.5 They found that larger angles of incision (approaching 90°) tended to seal better under conditions of lower IOP whereas incisions with a low angle of approach tended to seal better with a higher IOP. Recently, Fine, et al, used the Visante Anterior Segment OCT system (Carl Zeiss Meditec, Inc., Dublin, CA) to observe clear corneal cataract incisions, finding that the stromal swelling lasts for at least 24 hours and that the incision’s arc length was generally longer than the chord length due to its arcuate architecture.7 However, no measurements of wound dimensions were reported.
We were surprised to find that the average incision (chord) length (1.8 mm) was significantly shorter than the intended length of 2.0 mm. The surgeons observed that in most cases the incision was seen as slightly longer than 2.0 mm intraoperatively, because entry into the anterior chamber was made by a downward angulation of the blade when the entry point was already at the 2-mm etching on the ClearCut blade. The 10% shortfall might be explained by the stretching of the cornea under the force of the advancing blade. If this is true, we should observe less discrepancy if a diamond blade that cuts with less force was used. Nonetheless, most of our incisions were self-sealing, as were single-plane clear corneal incisions made with metal or diamond blades in several other studies.5, 7, 11
Some authors have advocated that proper self-sealing cataract incisions should be square or near-square.12, 13 Our results suggest a near-square incision is not necessary for self-sealing in most cases.
We suggest that studies of self-sealing incisions use OCT or other tomographic imaging technique to measure actual wound angle and length. This may be more accurate than markings on blades or physical sectioning of the eye, which could introduce distortions.
We have high confidence that the OCT measurements in this study were accurate. The dimension of the OCT image was calibrated to an accuracy of ±5 µm. The unprocessed OCT image is distorted by refraction at the air-cornea and cornea-aqueous interfaces due to the difference in the speed of light in air, cornea and aqueous medium. This distortion was removed using computer image processing according to Fermat’s principle,10 which is theoretically exact. Since the index of air (1.000), cornea (1.389 ± 0.004) and the aqueous humor (1.343 ± 0.001) are known to very high precision,14 the dewarping process can be very precise. Dewarping software was available on the Zeiss Visante system used by Fine et al. in their cataract wound study,7 but not on the Zeiss Stratus system (a retinal scanner) used in the study by Torres et al.6 Proper calibration and dewarping is essential in anterior segment OCT measurements.
The angle of blade entry into the cornea has been shown to affect the self-sealing properties of the wound. At one extreme, an angle of 90°, or perpendicular to the wound, has almost no structural integrity under physiologic conditions, whereas smaller angles of approach have been shown to be more effective at creating a self-sealing wound.5 The angle of the incision in this study, 28°, appeared to be shallow enough to create a self sealing wound. The shallow angle gives the wound structural integrity, as the intraocular pressure would press the lower lip of the incision against the upper lip. A previous OCT study by Torres et al. measured widely incision angles of 33 to 85 degrees,6 which was probably due to a lack of dewarping to correct image distortions and dimensions. Our measurements showed the incision angle to be fairly consistent, within a range of ±5° standard deviation.
We did not observe any external or internal wound gaping in our OCT images. Fine et al found that wounds that did not receive stromal hydration may develop internal gaping and biplanar (with external groove) incisions develop both internal and external wound gaps.7 Torres et al. found internal gaping their uniplanar incisions in 25% of cases at 24 hours and 10% at 1 month.6 The incisions were made by surgeons in training in 55% of cases in the Torres series. The lack of gaping in our series might be due to the uniplanar construction, stromal hydration, experienced surgeons, more frequent use of sutures, and the late time of imaging (1 month after surgery).
In conclusion, OCT imaging is a fast, noncontact and precise method to measure the dimensions, shape and position of cataract surgical incisions. We recommend that cataract surgeons use OCT to measure cataract wounds and confirm the absence of gaping. This information may help in the development of a consistent technique to create self-sealing incisions and decrease the risk of endophthalmitis. We hope our measurement methods will be adapted in future studies.
Acknowledgments
Financial and proprietary interest:
Maolong Tang, Yan Li and David Huang received research grants from Carl Zeiss Meditec Inc. David Huang receives patent royalty from the Massachusetts Institute of Technology based on optical coherence tomography technology licensed to Carl Zeiss Meditec. David Huang receives research grants, stock options, potential patent royalties, and travel support from Optovue, Inc.
Financial Support:
The study was supported by NIH grants R01 EY018184, R01 EY013516 and P30 EY03040, a grant from Research to Prevent Blindness, Inc., and research grants from Carl Zeiss Meditec Inc.
Biography

Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nagaki Y, Hayasaka S, Kadoi C, et al. Bacterial endophthalmitis after small-incision cataract surgery. J Cataract Refract Surg. 2003;29:20–26. doi: 10.1016/s0886-3350(02)01483-9. [DOI] [PubMed] [Google Scholar]
- 2.Cooper BA, Holekamp NM, Bohigian G, Thompson PA. Case-control Study of Endophthalmitis After Cataract Surgery Comparing Scleral Tunnel and Clear Corneal Wounds. Am J Ophthalmol. 2003;136:300–305. doi: 10.1016/s0002-9394(03)00202-2. [DOI] [PubMed] [Google Scholar]
- 3.Taban M, Behrens A, Newcomb RL, et al. Acute Endophthalmitis Following Cataract Surgery. Arch Ophthalmol. 2005;123:613–620. doi: 10.1001/archopht.123.5.613. [DOI] [PubMed] [Google Scholar]
- 4.Mackool RJ, Russell RS. Strength of clear corneal incisions in cadaver eyes. J Cataract Refract Surg. 1996;22:721–725. doi: 10.1016/s0886-3350(96)80310-5. [DOI] [PubMed] [Google Scholar]
- 5.Taban M, Rao B, Reznik J, et al. Dynamic Morphology of Sutureless Cataract Wounds - Effect of Incision Angle and Location. Surv Ophthalmol. 2004;49 Suppl 2:S62–S72. doi: 10.1016/j.survophthal.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Torres LF, Saez-Espinola F, Colina JM, et al. In vivo architectural analysis of 3.2 mm clear corneal incisions for phacoemulsification using optical coherence tomography. J Cataract Refract Surg. 2006;32:1820–1826. doi: 10.1016/j.jcrs.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 7.Fine IH, Hoffman RS, Packer M. Profile of clear corneal cataract incisions demonstrated by ocular coherence tomography. J Cataract Refract Surg. 2007;33(1):94–97. doi: 10.1016/j.jcrs.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 8.Kohnen T, Lambert RJ, Koch DD. Incision Sizes for Foldable Intraocular Lenses. Ophthalmology. 1997;104:1277–1286. doi: 10.1016/s0161-6420(97)30147-x. [DOI] [PubMed] [Google Scholar]
- 9.Li Y, Shekhar R, Huang D. Corneal pachymetry mapping with high-speed optical coherence tomography. Ophthalmology. 2006;113(5):792–799. doi: 10.1016/j.ophtha.2006.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Westphal V, Rollins AM, Radhakrishnan S, Izatt JA. Correction of geometric and refractive image distortions in optical coherence tomography applying Fermat's principle. Optics Express. 2002;10(9):397–404. doi: 10.1364/oe.10.000397. [DOI] [PubMed] [Google Scholar]
- 11.McDonnell PJ, Taban M, Sarayba MA, et al. Dynamic Morphology of Clear Corneal Cataract Incisions. Ophthalmology. 2003;110:2342–2348. doi: 10.1016/S0161-6420(03)00733-4. [DOI] [PubMed] [Google Scholar]
- 12.Masket S, Belani S. Proper wound construction to prevent short-term ocular hypotony after clear corneal incision cataract surgery. J Cataract Refract Surg. 2007;33:383–386. doi: 10.1016/j.jcrs.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 13.Ernest PH, Lavery KT, Kiessling LA. Relative strength of scleral corneal and clear corneal incisions constructed in cadaver eyes. J Cataract Refract Surg. 1994;20(6):626–629. doi: 10.1016/s0886-3350(13)80651-7. [DOI] [PubMed] [Google Scholar]
- 14.Lin RC, Shure MA, Rollins AM, et al. Group index of the human cornea at 1.3-microm wavelength obtained in vitro by optical coherence domain reflectometry. Opt Lett. 2004;29(1):83–85. doi: 10.1364/ol.29.000083. [DOI] [PubMed] [Google Scholar]