Abstract
OBJECTIVES: The aim of this study was to assess dietary practices and risk profile (hypertension, obesity, lipid profile and glycemic control) among people with diabetes in Al-Ain District, United Arab Emirates (UAE). METHODS: During 2006, we performed a cross-sectional study of diabetic patients attending diabetic outpatient clinics at Tawam Hospital and primary health care centers in Al-Ain District. Subjects completed an interviewer-administered questionnaire, blood pressure, body mass index, percentage body fat and abdominal circumference were measured and recorded and the most recent HbA1c levels and fasting lipid profile were identified. RESULTS: A sample of 409 diabetic patients was recruited, 50% of whom were illiterate. Only 24% read food labeling. 76% reported being unable to distinguish clearly between low and high carbohydrate index food items and no one reported counting calorie intake. 46% reported that they had never been seen by dietician since their diagnosis. Their overall risk profile, notably body weight, lipid profile and blood pressure, was very unfavorable; more than half of the study sample had uncontrolled hypertension and uncontrolled lipid profile and the majority was overweight (36%) or obese (45%). Abdominal obesity was particularly common (59%). Only 31% had an HbA1c of less than 7%. CONCLUSIONS: The dietary practices of diabetic patients in the UAE are inadequate and need improvement.
Keywords: diabetes, diet, obesity, glycemic control, UAE, diabetes care, compliance
Introduction
Diabetes mellitus (DM) in adults is a major worldwide health problem. Its prevalence is on the rise in many parts of the developing world in response to increasing prosperity and sedentary life styles. An example is the United Arab Emirates (UAE), which has seen enormous changes in lifestyle and wealth over the past few decades, similar to other Gulf States. The prevalence of diabetes in the UAE is rated as the second highest in the world according to the International Diabetes Federation (2007) [1]. Recently, age-standardized rates for DM (diagnosed and undiagnosed) and pre-diabetes in a population-based sample in Al-Ain were 29.0 and 24.2% respectively among 30-64 year olds [2].
The "ABC" of diabetes control, A1c, Blood pressure (BP), and LDL-Cholesterol, involves adopting lifelong healthy lifestyle measures, in addition to any pharmacological treatment that may be required. Appropriate dietary practices are a basic and integral part treating diabetes mellitus and may reduce the development of disease complications by improving risk factor profiles. The goals of diet control are to improve quality of life, nutritional status and risk factors as well as to prevent the chronic complications of diabetes. It is well documented that diet control can improve glycemic control [3] and may reduce glycosylated hemoglobin (HbA1c) by 1.0 to 2.0% [4, 5] and, when used in combination with other components of diabetes care, can further improve clinical and metabolic outcomes [4, 5]. This kind of improvement in glycemic control is related both to the degree of caloric restriction and weight reduction [6]. While it is acknowledged that dietary modification can improve many aspects of type 2 diabetes including obesity, hypertension, insulin release and responsiveness, in practice, lack of dietary compliance is a major limiting factor in achieving glycemic control in type 2 diabetes. In spite of the importance of diet in the management of diabetes mellitus, diabetic patients are often unaware of its place in ensuring good glycemic control. Even in communities with a good level of education, it is well known that patients commonly fail to adhere to dietary recommendations [7-9].
Achieving optimal glycemic control in diabetic patients has proven a real challenge to health providers in developing and developed countries alike. A Swedish survey found that only 34% of type 2 diabetes patients had good metabolic control [10]. In the UAE, the mean HbA1c of Emiratis with type 2 diabetes in primary health care settings has been shown to be 8.3%, and only 38% of patients had good glycemic control (HbA1c < 7.0%) [11]. In the UK, a study showed that only 39% patients ate within 20% of their prescribed carbohydrate intake [7]. Other studies in Mexico and Thailand showed non-compliance rates to diet of 62% and 45.7% respectively [12, 13]. To assess the current situation in relation to diet compliance and glycemic control in the UAE we decided to carry out a survey among diabetic patients in Al-Ain District of Abu Dhabi Emirate. To our knowledge, there is no previous study from the UAE addressing these issues.
Methods
Subjects
The study was a cross-sectional evaluation of diabetic patients, either type 1 or 2, attending diabetic outpatient clinics at Tawam Hospital and randomly selected primary health care centers in Al-Ain District, performed during the period from May to October 2006. Al-Ain, located in the interior of Abu Dhabi Emirate, constitutes its second largest district, with an approximate population of 500,000. Patients who had been diagnosed with diabetes for at least one year and were aged 18 years and above were selected randomly from the clinic appointment list.
After obtaining informed consent (written consent from literate patients and a verbally informed consent from illiterate patients), patients were interviewed by a trained nurse. The questionnaire was based on a review of the literature and input from local experts. It had been piloted on ten diabetic patients and modified as necessary for clarity. It provided sociodemographic data, such as sex, age, marital status, level of education (on a scale of 1-5 ranging from illiterate to university level education), occupation, and health-related parameters such as smoking status, history of diabetes, current management, eating practices and sources of nutritional information. Each interview took 25-30 minutes.
Weight and height were measured using a portable digital scale and portable stadiometer. Abdominal circumference was measured with a flexible tape over loose thin clothing (for cultural reasons). Percentage body fat was assessed using the Tanita Body Composition Analyzer TBF-300. Blood pressure (BP) (systolic and phase-V diastolic) recordings were made after the subjects had rested in the sitting position for 10 minutes using a validated electronic sphygmomanometer. Three separate readings were taken and their mean recorded. The results of the most recent investigations, such as HbA1c and fasting lipid profile measured using a Beckman Coulter DXC800 auto-analyzer (Beckman Instruments, Inc., Fullerton, California), were obtained from patients’ medical records. The study was approved by the Al-Ain Medical District Human Research Ethics Committee.
Statistical methods
Standard descriptive and analytical statistical methods for univariate and bivariate analysis, such as means, 95% confidence intervals, independent sample t-tests, and Chi-square tests for association, were used. Spearman's correlation coefficient (rho) was used as a measure of correlation. For multivariate analysis, multiple linear regression was performed with demographic, dietary and behavioral items identified beforehand. SPSS 15.0 was employed for all analyses.
Results
General
A sample of 409 diabetic patients (mean age 51.44 ± 11.2 years) was recruited (Table 1). Of the total population, 96% had type 2 DM (Table 2), 22% were using insulin and 98% were taking one or more oral hypoglycemic agents. 61% were female and 50% were illiterate (36% of males and 59% of females).
Table 1. Sociodemographic characteristics of diabetic patients in Al-Ain District, UAE (n = 409).
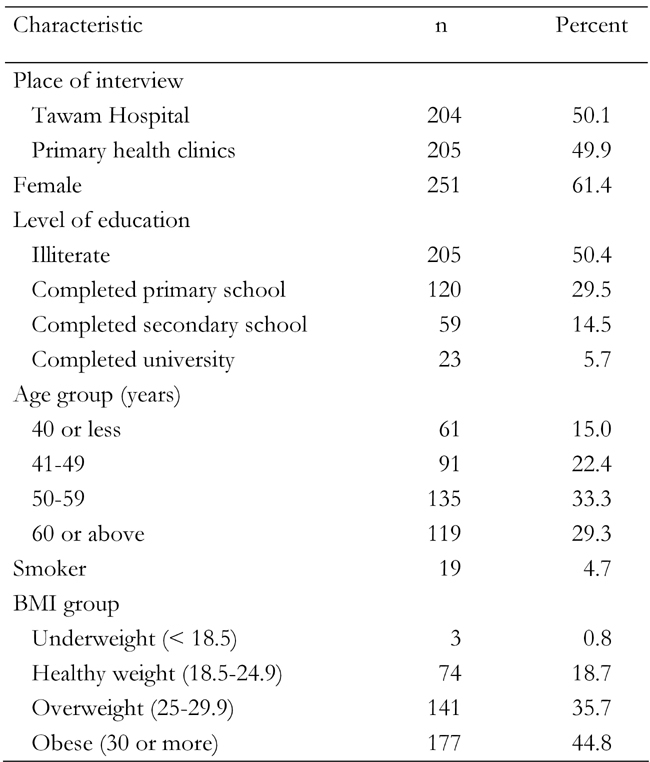
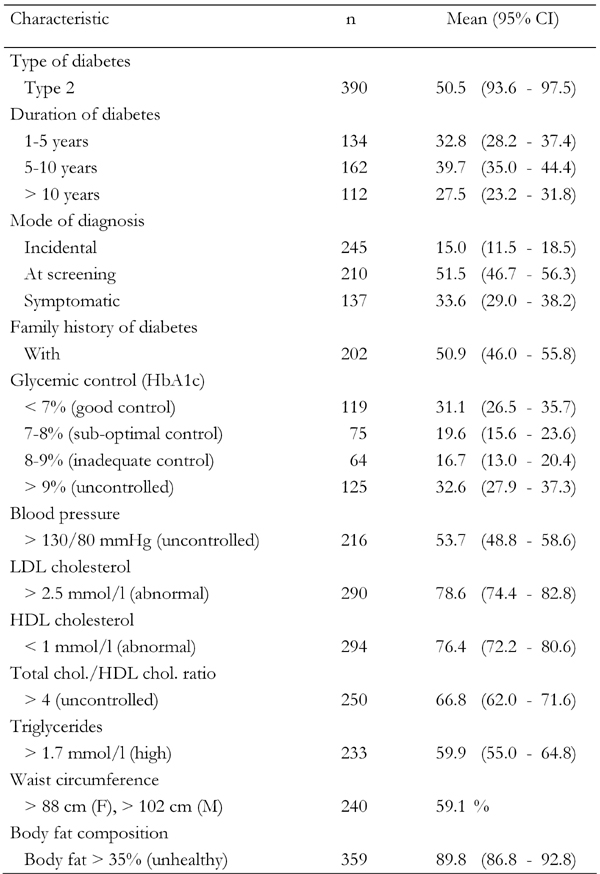
Table 2. Clinical characteristics of diabetic patients in Al-Ain District, UAE (n = 409).
Dietary habits and compliance
Forty-six percent reported that they had never been seen by a dietician since their diagnosis. There was no statistically significant difference between males and females in this respect; neither was there a difference in terms of age or level of education.
Only 51% reported taking low fat or skimmed milk, and 8% used double cream milk. 42% failed to remove the fat from meat and 23% did not remove skin from chicken before cooking. There was no statistically significant effect of sex, age or education on these behaviors. In 11%, the main method of cooking was frying. Only 24% paid attention to food labeling (38% among literates and 12% of illiterates, probably read by relatives) and 76% reported being unable to distinguish clearly between low and high carbohydrate index food items. No one reported counting calorie intake. Although the majority of subjects reported that they usually eat with their family members, in only 45% of cases did family members accompany patients, who received formal dietary consultations, to diabetes education sessions.
Doctors were reported to be the best source of advice regarding diet by the vast majority of patients (95%). Dieticians, relatives, friends, mass media, internet and nurses were not considered to be the mainstream source of dietary advice.
Glycemic control
60% of our patients reported that they performed self-testing for blood glucose. Only 31% had an HbA1c of less than 7%.
The number of carbonated drinks was the only variable significantly associated with HbA1c level (Spearman's rho = 0.12, p = 0.02), although the association was weak. Non-drinkers had lower levels of HbA1c (7.85 ± 2.00) compared with drinkers (regular carbonated drink: 8.19 ± 2.24, diet carbonated drink: 8.18 ± 2.48). There was a trend towards a statistically significant positive association between the consumption of carbonated drinks and HbA1c levels. The association became significant in multivariate analysis, when we regressed HbA1c levels on demographic, dietary and behavioral variables. Then we found that, in addition to the number of carbonated drinks (beta = 0.201, p = 0.029), age (beta = -0.023, p = 0.047) and level of education (beta = -0.262, p = 0.06) had a marginal significant association with HbA1c levels. Rather surprisingly, neither measure was influenced by age or level of education.
Risk profile
Overall risk profile, particularly body weight, lipid profile, and blood pressure was very poor: more than half of the study sample had inadequate blood pressure and lipid control. (see Table 2). According to body mass index (BMI), only 19% of the studied sample was of normal weight; the majority was either overweight (25 < BMI < 30, 36%) or obese (BMI ≥ 30, 45%). Abdominal obesity (>88 cm for females and >102 cm for males) was present in 59% of the total sample and was more common among females (77%) than males (30%) (chi-square test, p < 0.01).
Intake of staple food (mostly derived from rice and wheat, such as pasta) was also related to blood pressure, as both the number of spoons of staple food (beta = 1.62) and BMI (beta = 0.33), as well as age (beta = 0.16), were significantly related to mean blood pressure (MBP) in a multiple linear regression analysis of MBP on age, anthropometric and nutritional variables.
Multiple linear regression of BMI on sex, age, education, and various nutritional and exercise variables showed that BMI was mainly related to gender (females 4.8 kg/m2 heavier) and the number of spoons of carbohydrate staple (rice, macaroni etc) they take (approximately 0.9 kg/m2 heavier per daily spoon of staple (mean daily intake 3.12 spoons, SD = 0.98)).
Discussion
Although diet is the cornerstone of treatment of diabetes mellitus, patients find this area of self-management difficult. Most of the dietary habits of these patients were violating good dietary advice, as is clear from the contents of their reported diets as well as from their BMI. It is unclear whether this is due to non-compliance or non-adherence, or lack of clear, comprehensible resources and guidelines. Also, many (mainly elderly) patients were illiterate, requiring guidelines to be memorized or the constant support of literate relatives. Many patients were not seen by dieticians, a situation generally obtaining in poorer countries [14]. That these problems are shared with neighboring countries is no surprise. In the similar community of Saudi Arabia, it was reported that only 40% of diabetic patients had good compliance with their diet [15].
Self monitoring of blood glucose was also poor, consistent with earlier findings [2]. This is probably related to a lack of awareness of its importance in the management of diabetes, as there are no relevant financial barriers. While for UAE nationals the government provides glucometers, test strips, lancets and swabs free of charge, the care of persons with diabetes in the UAE is currently unbalanced. Although the latest tests and medications are available, lifestyle changes and basic diabetic education fall short of the ideal.
The main sources of dietary knowledge were generally treating physicians, with minor inputs from the family and social circle. Making the right daily choices of healthy food is challenging and needs individualized dietary prescription best delivered by a dedicated diabetes dietician. Most patients are followed up by primary care physicians and, unfortunately, the current primary health care system in Al-Ain is not based on continuity of care and accountability, but rather on rapid access without appointment to any available physician.
Our study suggests that restricting the amount of starchy staple foods could be of great importance, as this was correlated with both BMI and blood pressure. Although carbonated drinks were associated with poor control of diabetes, we do not think that there is enough evidence to recommend restricting consumption of the sugar-free variants of these beverages. Perhaps our finding may be partly due to confounding or reverse causation (e.g. patients with less well controlled diabetes are thirstier than those with well controlled diabetes, assuming that they quench their thirst with carbonated drinks).
Dietary prescriptions should begin by determining the patient's dietary preferences, patterns of physical activity, social support, education level, time constraints and other challenges. It is important to individualize dietary counseling, as standardized routine counseling will fail to empower patients to self-manage their disease [16]. A dietary history is helpful in assessing caloric intake, dietary content and carbohydrate consistency. It is important to remember that the more marked the changes are from what the patient likes to eat, the less likely the patient is to comply with dietary prescription [17].
A further possible step that could be considered to improve compliance is involving relatives. Despite the fact that most patients live and eat with their extended family, only 45% reported that their family members were involved in the dietary consultation. The engagement of family members in dietary consultation and diabetic education is essential, especially in this setting [18]. This is supported by various studies, which show that involvement of the family in patient care was strongly associated with diet, exercise and medication adherence [19-22].
As long as insufficient numbers of dieticians with in-depth knowledge of the culture and language of the UAE are available, their role should be assumed as best as possible by physicians. During follow-up visits, it is important for the clinician to ask specifically about diet and exercise to reinforce their importance. Ideally, patients should be able to quote their dietary prescriptions in detail.
Sustaining motivation is rather difficult. Achieving treatment goals such as weight reduction, better glycemic, lipid and blood pressure control, can be reinforced with appropriate feedback to the patient [23]. At the individual level, it is important to identify personal and familial barriers to adherence to prescribed diabetic diets [24]. In this respect, it may be worth remembering that patients and educators may view barriers differently [25]. Dietary workshops with small groups of patients have proven to be of great benefit in Western societies [26]. The local applicability and feasibility of this practice should be tested.
Self-monitoring of blood glucose was done by a minority of our patients (40%). Frequent self-monitoring of blood glucose levels needs to be taught and encouraged, as it is known to be associated with better glycemic control regardless of diabetes type or therapy [27]. Self-monitoring of dietary intake and weight, as well as periodic adjustments to fit changing lifestyle patterns, is important in sustaining and promoting dietary compliance. In our setting, there are few qualified diabetes dieticians who see patients on appointment. Most patients find it difficult to be scheduled for appointments with a dietician. An integrated multidisplinary team is the best solution to improve care.
Diabetes education websites in both Arabic and English would provide a great educational resource for some diabetic patients and their family members alike. The media should be more actively involved in keeping patients well informed and up to date about their care and the importance of their condition. Currently the media play only a minor role in education.
The limitations of our study refer to the way of dietary assessment, which was based on self-reported dietary habits. The best tool to assess compliance is keeping accurate records of food intake using a diet diary. All the subjects in our study were from Al-Ain City and thus the results cannot be generalized to the whole of the UAE. This is a cross-sectional study. While this has well known limitations, it does give a clear snapshot of the current situation and may help in both developing improvements in care and in designing future prospective studies to assess those improvements. One area in need of assessment is the impact and value of locally trained dieticians on our diabetic patients.
Conclusions
This study showed that the dietary practices of subjects with diabetes are inadequate and need improvement. The number of practicing dieticians needs to be increased in Al-Ain District to meet the demands for education and sustained lifestyle changes in a growing number of diabetic patients in the city. In addition, as health education is best done in settings where real, local, food is used, selected local food items should be part of the routine dietary advice offered by the dietician.
Acknowledgments
This work was financially supported by the Faculty of Medicine and Health Sciences, UAE University, under contract number NP/06/18. Our special thanks are extended to the staff, doctors and nurses working in the Tawam hospitals and primary health care centers, where the survey was conducted, for their invaluable support. Our special thanks go to Mrs. Shaikha Almarar at the Department of Internal Medicine, FMHS, for her help in data entry and to Mr. Hussain Al-Ajab from the Department of Community Medicine, FMHS, for his help with data analysis and tabulating the study results.
References
- 1.IDF Atlas. International Diabetes Federation; Available online at http://www.eatlas.idf.org/Complications/ [Google Scholar]
- 2.Saadi H, Carruthers SG, Nagelkerke N, Al-Maskari F, Afandi B, Reed R, Lukic M, Nicholls MG, Kazam E, Algawi K, Al-Kaabi J et al. Prevalence of diabetes mellitus and its complications in a population-based sample in Al-Ain, United Arab Emirates. Diabetes Res Clin Pract. 2007;78(3):369–377. doi: 10.1016/j.diabres.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 3.Pastors JG, Warshaw H, Daly A, Franz M, Kulkarni K. The evidence for the effectiveness of medical nutrition therapy in diabetes management. Diabetes Care. 2002;25(3):608–613. doi: 10.2337/diacare.25.3.608. [DOI] [PubMed] [Google Scholar]
- 4.Pi-Sunyer FX, Maggio CA, McCarron DA, Reusser ME, Stern JS, Haynes RB, Oparil S, Kris-Etherton P, Resnick LM, Chait A et al. Multicenter randomized trial of a comprehensive prepared meal program in type 2 diabetes. Diabetes Care. 1999;22(2):191–197. doi: 10.2337/diacare.22.2.191. [DOI] [PubMed] [Google Scholar]
- 5.Kulkarni K, Castle G, Gregory R, Holmes A, Leontos C, Powers M, Snetselaar L, Splett P, Wylie-Rosett J. Nutrition Practice Guidelines for Type 1 Diabetes Mellitus positively affect dietitian practices and patient outcomes. The Diabetes Care and Education Dietetic Practice Group. J Am Diet Assoc. 1998;98(1):62–70. doi: 10.1016/s0002-8223(98)00017-0. [DOI] [PubMed] [Google Scholar]
- 6.Wing RR, Blair EH, Bononi P, Marcus MD, Watanabe R, Bergman RN. Caloric restriction per se is a significant factor in improvements in glycemic control and insulin sensitivity during weight loss in obese NIDDM patients. Diabetes Care. 1994;17(1):30–36. doi: 10.2337/diacare.17.1.30. [DOI] [PubMed] [Google Scholar]
- 7.Close EJ, Wiles PG, Lockton JA, Walmsley D, Oldham J, Wales JK. The degree of day-to-day variation in food intake in diabetic patients. Diabet Med. 1993;10(6):514–520. doi: 10.1111/j.1464-5491.1993.tb00112.x. [DOI] [PubMed] [Google Scholar]
- 8.Monnier L, Grimaldi A, Charbonnel B, Iannascoli F, Lery T, Garofano A, Childs M. Management of French patients with type 2 diabetes mellitus in medical general practice: report of the Mediab observatory. Diabetes Metab. 2004;30(1):35–42. doi: 10.1016/s1262-3636(07)70087-3. [DOI] [PubMed] [Google Scholar]
- 9.Rivellese AA, Boemi M, Cavalot F, Costagliola L, De Feo P, Miccoli R, Patti L, Trovati M, Vaccaro O, Zavaroni I Mind.it Study Group. Dietary habits in type II diabetes mellitus: how is adherence to dietary recommendations? Eur J Clin Nutr. 2008;62(5):660–664. doi: 10.1038/sj.ejcn.1602755. [DOI] [PubMed] [Google Scholar]
- 10.Holmström IM, Rosenqvist U. Misunderstandings about illness and treatment among patients with type 2 diabetes. J Adv Nurs. 2005;49(2):146–154. doi: 10.1111/j.1365-2648.2004.03274.x. [DOI] [PubMed] [Google Scholar]
- 11.Al-Maskari F, El-Sadig M. Prevalence of risk factors for diabetic foot complications. BMC Fam Pract. 2007;8:59. doi: 10.1186/1471-2296-8-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hernandez-Ronquillo L, Tellez-Zenteno JF, Garduno-Espinosa J, Gonzalez-Acevez E. Factors associated with therapy noncompliance in type-2 diabetes patients. Salud Publica Mex. 2003;45(3):191–197. doi: 10.1590/s0036-36342003000300008. [DOI] [PubMed] [Google Scholar]
- 13.Howteerakul N, Suwannapong N, Rittichu C, Rawdaree P. Adherence to regimens and glycemic control of patients with type 2 diabetes attending a tertiary hospital clinic. Asia Pac J Public Health. 2007;19(1):43–49. doi: 10.1177/10105395070190010901. [DOI] [PubMed] [Google Scholar]
- 14.Abioye-Kuteyi EA, Ojofeitimi EO, Ijadunola KT, Fasanu AO. Assessment of dietary knowledge, practices and control in type 2 diabetes in a Nigerian teaching hospital. Niger J Med. 2005;14(1):58–64. doi: 10.4314/njm.v14i1.37137. [DOI] [PubMed] [Google Scholar]
- 15.Khattab MS, Aboifotouh MA, Khan MY, Humaidi MA, al-Kaldi YM. Compliance and control of diabetes in a family practice setting, Saudi Arabia. East Mediterr Health J. 1999;5(4):755–765. [PubMed] [Google Scholar]
- 16.Williamson AR, Hunt AE, Pope JF, Tolman NM. Recommendations of dieticians for overcoming barriers to dietary adherence in individuals with diabetes. Diabetes Educ. 2000;26(2):272–279. doi: 10.1177/014572170002600207. [DOI] [PubMed] [Google Scholar]
- 17.Nuttall FQ. Carbohydrate and dietary management of individuals with insulin-requiring diabetes. Diabetes Care. 1993;16(7):1039–1042. doi: 10.2337/diacare.16.7.1039. [DOI] [PubMed] [Google Scholar]
- 18.Brekke HK, Jansson PA, Mansson JE, Lenner RA. Lifestyle changes can be achieved through counseling and follow-up in first-degree relatives of patients with type 2 diabetes. J Am Diet Assoc. 2003;103(7):835–843. doi: 10.1016/s0002-8223(03)00378-x. [DOI] [PubMed] [Google Scholar]
- 19.Albright TL, Parchman M, Burge SK RRNeST Investigators. Predictors of self-care behavior in adults with type 2 diabetes: an RRNeST study. Fam Med. 2001;33(5):354–360. [PubMed] [Google Scholar]
- 20.Wen LK, Shepherd MD, Parchman ML. Family support, diet, and exercise among older Mexican Americans with type 2 diabetes. Diabetes Educ. 2004;30(6):980–993. doi: 10.1177/014572170403000619. [DOI] [PubMed] [Google Scholar]
- 21.Wen LK, Parchman ML, Shepherd MD. Family support and diet barriers among older Hispanic adults with type 2 diabetes. Fam Med. 2004;36(6):423–430. [PubMed] [Google Scholar]
- 22.Guare JC, Wing RR, Marcus MD, Epstein LH, Burton LR, Gooding WE. Analysis of changes in eating behavior and weight loss in type II diabetic patients. Which behaviors to change. Diabetes Care. 1989;12(7):500–503. doi: 10.2337/diacare.12.7.500. [DOI] [PubMed] [Google Scholar]
- 23.Hadden DR, Blair AL, Wilson EA, Boyle DM, Atkinson AB, Kennedy AL, Buchanan KD, Merrett JD, Montgomery DA, Weaver JA. Natural history of diabetes presenting age 40-69 years: a prospective study of the influence of intensive dietary therapy. Q J Med. 1986;59(230):579–598. [PubMed] [Google Scholar]
- 24.Vijan S, Stuart NS, Fitzgerald JT, Ronis DL, Hayward RA, Slater S, Hofer TP. Barriers to following dietary recommendations in Type 2 diabetes. Diabet Med. 2005;22(1):32–38. doi: 10.1111/j.1464-5491.2004.01342.x. [DOI] [PubMed] [Google Scholar]
- 25.Shultz JA, Sprague MA, Branen LJ, Lambeth S. comparison of views of individuals with type 2 diabetes mellitus and diabetes educators about barriers to diet and exercise. J Health Commun. 2001;6(2):99–115. doi: 10.1080/108107301750254457. [DOI] [PubMed] [Google Scholar]
- 26.Heller SR, Clarke P, Daly H, Davis I, McCulloch DK, Allison SP, Tattersall RB. Group education for obese patients with type 2 diabetes: greater success at less cost. Diabet Med. 1988;5(6):552–556. doi: 10.1111/j.1464-5491.1988.tb01050.x. [DOI] [PubMed] [Google Scholar]
- 27.Karter AJ, Ackerson LM, Darbinian JA, D'Agostino RB Jr, Ferrara A, Liu J, Selby JV. Self-monitoring of blood glucose levels and glycemic control: the Northern California Kaiser Permanente Diabetes registry. Am J Med. 2001;111(1):1–9. doi: 10.1016/s0002-9343(01)00742-2. [DOI] [PubMed] [Google Scholar]


