Abstract
This study is to compare the therapeutic effect of posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF) with pedicle screw fixation on treatment in adult degenerative spondylolisthesis. A retrospective analysis of 187 patients to compare the complications and associated predictive factors of the two techniques of one level lumbar fusion. Ninety-one had PLIF with two cages and pedicle fixation (group 1), and ninety-six had TLIF with one cage and pedicle fixation (group 2). The two groups had similar age and sex distribution, and level of pain. Inclusion criteria and outcome measurements were identical in both groups. The two groups were operated on with autograft and cage with pedicle fixation. Before surgery and at the 2-year follow-up, pain (VAS) and functional disability (JOA) were quantified. The results showed there were no intraoperative deaths in our study. In the end 176 cases had 2-year follow-up while 11 cases were lost to follow-up. The follow-up rate was 93.4% (85/91) in the PLIF group and 94.8% (91/96) in the TLIF group. All patients had bone fusion, and there were no cases of cage extrusion. The pain index improved from 7.08 ± 1.13 to 2.84 ± 0.89 in PLIF patients and improved from 7.18 ± 1.09 to 2.84 ± 0.91 in TLIF patients (P < 0.001). There were 42 cases of excellent, 29 cases of good, 11 cases of general, and 3 cases of poor results in PLIF group. There were 46 cases of excellent, 31 case of good, 12 case of general, and 2 cases of poor results in TLIF group. The JOA score in all patients was 84.1% of good or excellent (83.5% in PLIF and 84.6% in TLIF, P > 0.05). The average preoperative slip was 30.1 ± 7.2% in PLIF group while in the TLIF it was 31.4 ± 8.3%. Immediately post operatively it was reduced to 7.3 ± 2.1% and 7.4 ± 2.7% and at last F/U it was 8.1 ± 2.8% and 8.2 ± 2.6%, respectively. The average of reduction rate was 75.2 ± 6.4% in PLIF and 75.4 ± 6.2 in TLIF on the initial post operatively X-ray, and 72.6 ± 5.2% and 72.4 ± 5.4% on the follow-up. The percentage rate, reduction rate and lost of reduction rate between the two groups was similar (P > 0.05). The average pre operative disk and foramen height in the PLIF group improved from 6.8 ± 2.3 and 14.2 ± 1.7 preoperatively to 11.6 ± 1.5 and 18.7 ± 1.8 post operatively, respectively. At last follow up there was minimal lost of correction down to 11.24 ± 1.2 and 18.1 ± 1.8, respectively. Similarly in the TLIF group, pre operative disk and foramen height were improved from 6.7 ± 1.7 and 14.1 ± 1.8 to 11.4 ± 1.6 and 18.5 ± 1.6 immediately post operative. At last follow up minimal lost of correction was noted with average disc height of 11.3 ± 1.4 and 18.2 ± 1.7. Both techniques achieve statistical significance in restoration of disc and foraminal (P < 0.01); however, there was no statistical difference between the two techniques. In conclusion, interbody fusion with either a PLIF technique or a TLIF technique provides good outcomes in the treatment of adult degenerative spondylolisthesis. The TLIF procedure is simpler and is as safe and effective as the PLIF technique.
Keywords: Spondyolisthesis, Interverterbral fusion, Internal fixation
Introduction
Interbody fusion techniques have been developed to provide solid fixation of spinal segments while maintaining load-bearing capacity and proper disc height [13]. The ability to reconstruct the anterior column after disc evacuation is important because 80% of the compressive, torsion, and shear forces are transmitted through the anterior column [5, 8, 15]. Reconstruction of the anterior column can be performed via the anterior approach, with direct transperitoneal or retroperitoneal access to the lumbar spine. Posterior fusion and instrumentation can be added to obtain a 360° or circumferential fusion. This technique involves two surgical approaches, with increased operating time (compared to posterolateral fusion) as well as potential complications pertaining to anterior approaches to the lumbar spine. An alternative method of reconstructing the anterior column is via posterior lumbar interbody fusion. The original technique [1] of posterior lumbar interbody fusion was modified by some surgeons. The transforaminal posterior lumbar interbody fusion technique developed by Dr. Harms involves a transforaminal approach to the anterior interspace, and thought that the disadvantages associated with the TLIF, for example the epidural scarring, can be potentially avoided [6].
To the best of our knowledge, there is a few reported in the medical literature comparing the complications and their predictive factors between PLIF and TLIF one level segment treatment in adult degenerative spondylolisthesis. The purpose of our study was to compare the two surgical procedures, identify procedure-specific complications, and determine preoperative factors that may predict the complications.
Materials and methods
A retrospective study on patients with L5–S1 or L4–L5 adult degenerative spondylolisthesis spondylolisthesis (grades I–II) from June 2002 to July 2005 that had PLIF or TILF. One hundred and eighty-seven patients initially fulfilled the study criteria, and 11 patients were lost to follow-up. Of the remaining 176 patients available for analysis, 85 had PLIF with two cages and pedicle fixation (group 1, included 41 men and 44 women with an average age of 58.73 ± 9.61 years, and 91 had TLIF with one cage and pedicle fixation (group 2, included 46 men and 45 women with an average age of 57.51 ± 11.17 years). The inclusion criteria were adult degenerative spondylolisthesis (grades I–II) which only one level fusion. Exclusion criteria included pathologic conditions of the lumbar spine (trauma, tumor, or infection). The two groups had similar age and sex distribution, level of pain, and the pain history (Table 1).
Table 1.
Patient data
| Group | Sex | Old (years) | Level | History (years) | ||
|---|---|---|---|---|---|---|
| Male | Female | L45 | L5S1 | |||
| PLIF | 41 | 44 | 58.73 ± 9.61 | 40 | 45 | 4.16 ± 1.02 |
| TLIF | 46 | 45 | 57.51 ± 11.17 | 44 | 47 | 4.30 ± 1.08 |
| t/x | 0 | 0.56 | 0.36 | −0.83 | ||
| P | 1 | 0.57 | 0.55 | 0.41 | ||
There was no significant difference between two groups (P > 0.05)
Surgical procedures
All patients had single level fusion performed. The PLIF procedure were performed in the standard fashion reported in previous studies, with two cages packed with autologenous bone graft [9]. Posterior segmental spinal pedicle screw instrumentation was used in all cases. The TLIF procedure was performed in the standard fashion reported in previous studies, with one cage packed with autologenous bone graft [6]. Posterior segmental spinal pedicle screw instrumentation was used in all cases. Brace support was recommended for 6–8 weeks after surgery.
Critical of clinical outcomes
Before surgery and at the 2-year follow-up, pain (VAS) and functional disability (JOA) were quantified. The focus was to evaluate four radiographic characteristics at follow-up: (1) percentage of slip and percentage of reduction, (2) height of disk space and intervertebral foramen, (3) cage position, and (4) fusion rate. Bone fusion was determined by the method described by Gertzbein [3]. The criteria for fusion were continuity of trabecular pattern, and the fusion rate assessed using CT-scan reconstruction.
Statistical analysis
All measurements were performed by a single observer and are expressed as means ± SD. Using the SPSS 11.5 statistics software, classic t-test and chi-square test were performed.
Results
There was no intraoperative death in our study. In ends 176 cases had follow-up and 11 cases lost, and the follow-up rate was 93.4% (85/91) in the PLIF group and 94.8% (91/96) in the TLIF group. The followed time from 24 to 35 months (average 29 months), and average (29.49 ± 3.66) months on PILF and (29.63 ± 3.68) months on TLIF (t = −0.24, P = 0.81, >0.05).
The pain index improved from 7.08 ± 1.13 to 2.84 ± 0.89 (t = 27.03, P = 0.0000, <0.001) in PLIF patients and improved from 7.18 ± 1.09 to 2.84 ± 0.91 (t = 29.57, P = 0.0000, <0.001) in TLIF patients. There were 42 cases of excellent, 29 cases of good, 11 cases of general, and 3 cases of poor in PLIF group. There were 46 cases of excellent, 31 case of good, 12 case of general, and 2 cases of poor in TLIF group. The JOA score in all patients was 84.1% of good or excellent (83.5% in PLIF and 84.6% in TLIF, x = 5.29, P = 0.21, >0.05).
The average of spondylolisthesis was 30.1 ± 7.2% in PLIF and 31.4 ± 8.3% in TLIF on the preoperatively, 7.3 ± 2.1% and 7.4 ± 2.7% on the initial postoperatively, and 8.1 ± 2.8% and 8.2 ± 2.6% on the final follow-up. The average of reduction rate was 75.2 ± 6.4% in PLIF and 75.4 ± 6.2 in TLIF on the initial postoperatively, and 72.6 ± 5.2% and 72.4 ± 5.4% on the follow-up (Table 2). The rate of spondylolisthesis and reduction were not significantly altered between the initial postoperative to the final postoperative follow-up (P > 0.05). The spondylolisthesis rate, reduction rate and lost of reduction rate were similar between two groups (P > 0.05).
Table 2.
Lithe and reduction rate compared to between two groups (x ± s) (%)
| Groups | Spondylolisthesis rate | Reduction rate | ||||
|---|---|---|---|---|---|---|
| Pre- | Post- | Follow-up | Post- | Follow-up | Lost | |
| PILF | 30.1 ± 7.2 | 7.3 ± 2.1* | 8.1 ± 2.8 | 75.2 ± 6.4 | 72.6 ± 5.2 | 3.2 ± 1.1 |
| TILF | 31.4 ± 8.3 | 7.4 ± 2.7* | 8.2 ± 2.6** | 75.4 ± 6.2 | 72.4 ± 5.4** | 3.4 ± 1.2 |
* Compared to the pre-operation P < 0.05; ** Compared to PILF P > 0.05
The average disk and foramen height was 6.8 ± 2.3 and 14.2 ± 1.7 preoperatively, 11.6 ± 1.5 and 18.7 ± 1.8 on the initial postoperatively, and 11.24 ± 1.2 and 18.1 ± 1.8 on the follow-up in PLIF (Table 3). Compare to PLIF, the average disk and foramen height was 6.7 ± 1.7 and 14.1 ± 1.8 preoperatively, 11.4 ± 1.6 and 18.5 ± 1.6 on the initial postoperatively, and 11.3 ± 1.4 and 18.2 ± 1.7 on the follow-up in TLIF. The disk height and intervertebral foramen height were better than preoperational (P < 0.01), and there were no difference between two groups (P > 0.05). The lost of intervertebral space and intervertebral foramen were similar between two groups (P > 0.05).
Table 3.
The intervertebral space and intervertebral foramen height compared to between two groups (x ± s) (mm)
| Groups | Intervertebral space height | Intervertebral foramen height | ||||
|---|---|---|---|---|---|---|
| Pre- | Post- | Follow-up | Pre- | Post- | Follow-up | |
| PILF | 6.8 ± 2.3 | 11.6 ± 1.5* | 11.2 ± 1.2 | 14.2 ± 1.7 | 18.7 ± 1.8* | 18.1 ± 1.8 |
| TILF | 6.7 ± 1.7 | 11.4 ± 1.6* | 11.3 ± 1.4** | 14.1 ± 1.8 | 18.5 ± 1.6* | 18.2 ± 1.7** |
* Compared to the pre-operation P < 0.05; ** Compared to PILF P > 0.05
All patients achieved spinal fusion with no cases of cage extrusion. There were three cases of loss of disk space height and foramen height between the initial and final postoperative X-rays suggestive of cage subsidence over time. But there were no infection on the clinical outcomes because all patients had the bone fusion.
There were four complications of group 1, included three cases of radiculitis (one man and two women) and one case of screw loosening (woman). CT-myelogram revealed two radiculitis patients had normal radiologic findings, and the third had left S1 radiculopathy after L4–L5 fusion that was caused by left foraminal stenosis at L5–S1. Three complications related to group 2, included two cases of radiculitis (one man and one woman) and one case of screw loosening (man). CT-myelogram revealed radiculitis patients had normal radiologic findings. Removal of the loosed pedicle screw was performed 18 months after had bone fusion and index surgery.
Discussion
Degenerative spondylolisthesis in adults is characterized by the loss of disk height across the affected segment with sagittal translational and is often coupled with rotational deformity. The goal of the surgical treatment of spondylolisthesis includes: the stabilization of the motion segment, the decompression of neural elements, the reconstitution of disk space height, and the restoration of sagittal plane translational and rotational alignment. The goal of stabilizing the spondylolytic level is accomplished by arthrodesis from a posterior, anterior, or combined approach. Depending on the severity and clinical features of the spondylolisthesis, it may also be desirable to reduce the forward translation, increase disk space height, decompress the neural elements, and increase or restore lumbar lordosis. Posterolateral instrumented or noninstrumented fusion (with or without decompression), anterior interbody fusion, and circumferential fusion have all been reported to provide acceptable fusion rates and clinical outcomes in adult patients with spondylolisthesis [9, 11]. In this study, the pain index improved from 7.08 ± 1.13 to 2.84 ± 0.89 in PLIF patients and from 7.18 ± 1.09 to 2.84 ± 0.91 in TLIF patients. There were 42 cases of excellent results and 29 cases of good results in PLIF group. There were 46 cases of excellent results and 31 cases of good results in TLIF group. The JOA score in all patients was 84.1% of good or excellent (83.5% in PLIF and 84.6% in TLIF), which means PLIF and TLIF were good methods for the spondylolisthesis and no difference of outcomes between two methods (Figs. 1, 2).
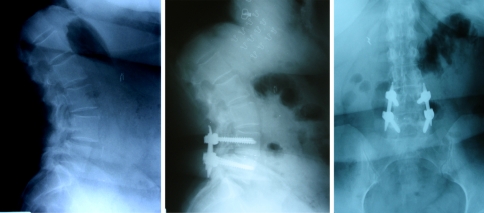
Fig. 1.
TLIF procedure with anterolisthesis reduction for L45 grade I spondylolisthesis. Note the severe disk space collapse and grade I anterolisthesis on the preoperative film (a), on the postoperative film (b, c). Note the reduction in the anterolisthesis and restoration of disk height and had the bone fusion
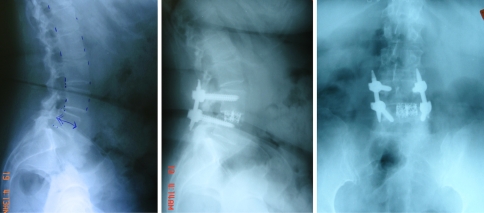
Fig. 2.
PLIF procedure with anterolisthesis reduction for L45 grade I spondylolisthesis. Note the severe disk space collapse and grade I anterolisthesis on the preoperative film (a), on the postoperative film (b, c). Note the reduction in the anterolisthesis and restoration of disk height and had the bone fusion
Posterior lumbar interbody fusion (PLIF) was first attempted by Cloward [1] in 1940 and later revised by Lin [9]. The chip PLIF procedure entails less retraction of the spinal cord and increases the bone fusion surface area, but it does not provide the additional mechanical support of an interbody cage. Interbody fusion techniques were developed in an attempt to preserve the load-bearing capacity of the spine, restore the sagittal plane alignment, and use the compressive loading on the bone to enhance the likelihood of fusion. The interbody fusion immediately produces a biomechanically stable postoperative spine, thus enhancing the opportunity for arthrodesis [2, 12, 14]. A posterolateral graft is easily added to this procedure, further enhancing the stability and likelihood of fusion. Additionally, the posterior approach avoids the morbidity factors associated with an anterior path to the spine. The PLIF procedure has gained popularity, with indications including spinal stenosis, instability, degenerative disc disease, spondylolisthesis, spondylolysis, and bilateral disc herniation. Although the PLIF procedure is useful in many cases, there are complications and contraindications. To obtain unobstructed access to the disc, the surgeon must retract the dural sheath out to midline. This manipulation can lead to nerve damage or neurogenic pain. Additionally, PLIF usually is limited to L3–S1 because of the increased risk of damage to the conus medullaris and cauda equine resulting from the need for retraction above these levels. In this study, the average of spondylolisthesis was 30.1 ± 7.2% in PLIF and 31.4 ± 8.3% in TLIF on the preoperatively, 7.3 ± 2.1% and 7.4 ± 2.7% on the initial postoperatively, and 8.1 ± 2.8% and 8.2 ± 2.6% on the final follow-up. The average of reduction rate was 75.2 ± 6.4% in PLIF and 75.4 ± 6.2 in TLIF on the initial postoperatively, and 72.6 ± 5.2% and 72.4 ± 5.4% on the follow-up (Table 2). The rate of spondylolisthesis and reduction were not significantly altered between the initial postoperative to the final postoperative follow-up (P > 0.05). The spondylolisthesis rate, reduction rate and lost of reduction rate was similar between two groups (P > 0.05).
The transforaminal lumbar interbody fusion (TLIF) technique was described by Harms and Jeszenszky [6] as a modification of the well-established PLIF procedure. The TLIF uses a posterior approach to the spine that runs through the far lateral portion of the vertebral foramen accesses the disc space, which provides the surgeon with a fusion procedure that may reduce many of the risks and limitations associated with PLIF, yet produces similar stability in the spine. This has been shown to reduce the incidence of postoperative radiculitis [7]. TLIF usually is performed unilateral approach preserving the interlaminar surface on the contralateral side, which can be used as a site for additional fusion. Like PLIF, TLIF is easily enhanced when combined with posterolateral fusion and instrumentation. Both procedures can provide circumferential spinal stabilization through a single posterior approach, but the more lateral access to the disk space in the TLIF technique requires less retraction of the thecal sac and neural elements than with the PLIF technique. In this study, the average disk and foramen height was 6.8 ± 2.3 and 14.2 ± 1.7 preoperatively, 11.6 ± 1.5 and 18.7 ± 1.8 on the initial postoperatively, and 11.24 ± 1.2 and 18.1 ± 1.8 on the follow-up in PLIF (Table 3). Compared to PLIF, the average disk and foramen height was 6.7 ± 1.7 and 14.1 ± 1.8 preoperatively, 11.4 ± 1.6 and 18.5 ± 1.6 on the initial postoperatively, and 11.3 ± 1.4 and 18.2 ± 1.7 on the follow-up in PLIF. The disk height and intervertebral foramen height were better than preoperational (P < 0.01), and there were no difference between two groups (P > 0.05). The lost of intervertebral space and intervertebral foramen were similar between two groups (P > 0.05).
Because the cauda equina obstructs the approach to the disc when PLIF is performed, the spine surgeon must perform the discectomy and graft insertion in a bilateral fashion, increasing the operative time. In contrast, the angle of approach normally obtained during TLIF allows a unilateral approach to the disc space, thus reducing operative time and blood loss. Humphreys et al. [7] found that patients undergoing the PLIF procedure had a higher incidence of complications, including radiculitis, which they attributed to the need for greater medial retraction of the thecal sac with the PLIF technique. In this study, there were four complications in the PLIF group 1, included three cases of radiculitis (one man and two women) and one case of screw loosening (woman). CT-myelogram revealed two radiculitis patients had normal radiologic findings, and the third had left S1 radiculopathy after L4–L5 fusion that was caused by left foraminal stenosis at L5–S1. Three complications related to the TLIF group 2, included two cases of radiculitis (one man and one woman) and one case of screw loosening (man). CT-myelogram revealed radiculitis patients had normal radiologic findings. Removal of the loosed pedicle screw was performed 18 months after had bone fusion and index surgery.
Altering the attachment sites for the musculature is likely to affect the mechanics of the lumbar spine [4]. This could lead to a change in direction of applied forces on the spinal column, increased pain during the recovery process, and a prolonged recovery time. With PLIF, the spinous processes of the involved vertebrae are destroyed. These bony structures serve as attachment sites for the muscular envelope that covers and supports the spinal column. Without the spinous processes intact, the muscular envelope produced by the erector spinae muscles cannot be restored properly. Patwardhan et al. [10] determined that the compressive load carrying capacity of the lumbar spine increased when the load path remained within a small range around the rotation centers of the lumbar segments. By using and preserving the bony attachments of the lumbar spine, the TLIF technique can quicken and improve the patient’s recovery. In the current study, the authors inserted a single interbody cage in TLIF and two interbody cages in PLIF shows sufficient mechanical stability was achieved. All patients had bone fusion, and there were no cases of cage extrusion. All patients achieved spinal fusion with no cases of cage extrusion. There were three cases of loss of disk space height and foramen height between the initial and final postoperative X-rays suggestive of cage subsidence over time. But there were no infection on the clinical outcomes because all patients had the bone fusion.
Conclusion
Interbody fusion with either a PLIF technique or a TLIF technique provides good outcomes in the treatment of adult degenerative spondylolisthesis. The TLIF procedure is simpler and is as safe and effective as the PLIF technique. This study demonstrates that the TLIF technique offers a useful alternative to the more traditional PLIF procedure. Although this study has investigated the acute effects of the TLIF and PLIF procedures, long-term clinical outcomes studies are necessary to address issues concerning the clinical effectiveness of these procedures.
References
- 1.Cloward R. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. J Neurosurg. 1953;10:154–168. doi: 10.3171/jns.1953.10.2.0154. [DOI] [PubMed] [Google Scholar]
- 2.Evans JH. Biomechanics of lumbar fusion. Clin Orthop. 1985;193:38–46. [PubMed] [Google Scholar]
- 3.Gertzbein SD, Betz R, Clements D, et al. Semirigid instrumentation in the management of lumbar spinal conditions combined with circumferential fusion. A multicenter study. Spine. 1996;21:1918–1925. doi: 10.1097/00007632-199608150-00018. [DOI] [PubMed] [Google Scholar]
- 4.Goel VK, Kong W, Han JS, et al. A combined finite element and optimization investigation of lumbar spine mechanics with and without muscles. Spine. 1993;18:1531–1541. doi: 10.1097/00007632-199318110-00019. [DOI] [PubMed] [Google Scholar]
- 5.Harms J. Screw-threaded rod system in spinal fusion surgery. Spine. 1992;6:541–575. [Google Scholar]
- 6.Harms JG, Jeszenszky D. The unilateral, transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol. 1998;6:88–99. [Google Scholar]
- 7.Humphreys SC, Hodges SD, Patwardhan AG, et al. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine. 2001;26:567–571. doi: 10.1097/00007632-200103010-00023. [DOI] [PubMed] [Google Scholar]
- 8.Ishihara H, Osada R, Kanamori M, et al. Minimum 10-year followup study of anterior lumbar interbody fusion for isthmic spondylolisthesis. J Spinal Disord. 2001;14:91–99. doi: 10.1097/00002517-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Lin PM. A technical modification of Cloward’s posterior lumbar interbody fusion. Neurosurgery. 1977;1:118–124. doi: 10.1097/00006123-197709000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Patwardhan AG, Havey RM, Meade KP, et al. A follower load increases the load-carrying capacity of the lumbar spine in compression. Spine. 1999;24:1003–1009. doi: 10.1097/00007632-199905150-00014. [DOI] [PubMed] [Google Scholar]
- 11.Spruit M, Pavlov PW, Leitao J, et al. Posterior reduction and anterior lumbar interbody fusion in symptomatic low-grade adult isthmic spondylolisthesis: short-term radiological and functional outcome. Eur Spine. 2002;11:428–433. doi: 10.1007/s00586-002-0450-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steffee AD, Sitkowski DJ. Posterior lumbar interbody fusion and plates. Clin Orthop. 1988;227:99–102. [PubMed] [Google Scholar]
- 13.Stonecipher T, Wright S. Posterior lumbar interbody fusion with facet-screw fixation. Spine. 1989;14:468–471. doi: 10.1097/00007632-198904000-00026. [DOI] [PubMed] [Google Scholar]
- 14.Voor MJ, Mehta S, Wang M, et al. Biomechanical evaluation of posterior and anterior lumbar interbody fusion techniques. J Spinal Dis. 1998;11:328–334. [PubMed] [Google Scholar]
- 15.Yang SW, Langrana NA, Lee CK. Biomechanics of lumbosacral spinal fusion in combined compression-torsion loads. Spine. 1986;11:937–941. doi: 10.1097/00007632-198611000-00014. [DOI] [PubMed] [Google Scholar]