Abstract
The treatment of thoracic adolescent idiopathic scoliosis (AIS) of more than 80° traditionally consisted of a combined procedure, an anterior release performed through an open thoracotomy followed by a posterior fusion. Recently, some studies have reassessed the role of posterior fusion only as treatment for severe thoracic AIS; the correction rate of the thoracic curves was comparable to most series of combined anterior and posterior surgery, with shorter surgery time and without the negative effect on pulmonary function of anterior transthoracic exposure. Compared with other studies published so far on the use of posterior fusion alone for severe thoracic AIS, the present study examines a larger group of patients (52 cases) reviewed at a longer follow-up (average 6.7 years, range 4.5–8.5 years). The aim of the study was to evaluate the clinical and radiographic outcome of surgical treatment for severe thoracic (>80°) AIS treated with posterior spinal fusion alone, and compare comprehensively the results of posterior fusion with a hybrid construct (proximal hooks and distal pedicle screws) versus a pedicle screw instrumentation. All patients (n = 52) with main thoracic AIS curves greater than 80° (Lenke type 1, 2, 3, and 4), surgically treated between 1996 and 2000 at one institution, by posterior spinal fusion either with hybrid instrumentation (PSF–H group; n = 27 patients), or with pedicle screw-only construct (PSF–S group; n = 25 patients) were reviewed. There were no differences between the two groups in terms of age, Risser’s sign, Cobb preoperative main thoracic (MT) curve magnitude (PSF–H: 92° vs. PSF–S: 88°), or flexibility on bending films (PSF–H: 27% vs. PSF–S: 25%). Statistical analysis was performed using the t test (paired and unpaired), Wilcoxon test for non-parametric paired analysis, and the Mann–Whitney test for non-parametric unpaired analysis. At the last follow-up, the PSF–S group, when compared to the PSF–H group had a final MT correction rate of 52.4 versus 44.52% (P = 0.001), with a loss of −1.9° versus −11.3° (P = 0.0005), a TL/L correction of 50 versus 43% (ns), a greater correction of the lowest instrumented vertebra translation (−1.00 vs. −0.54 cm; P = 0.04), and tilt (−19° vs. −10°; P = 0.005) on the coronal plane. There were no statistically significant differences in sagittal and global coronal alignment between the two groups (C7-S1 offset: PSF–H = 0.5 cm vs. PSF–S = 0 cm). In the hybrid series (27 patients) surgery-related complications necessitated three revision surgeries, whereas in the screw group (25 patients) one revision surgery was performed. No neurological complications or deep wound infection occurred in this series. In conclusion, posterior spinal fusion for severe thoracic AIS with pedicle screws only, when compared to hybrid construct, allowed a greater coronal correction of both main thoracic and secondary lumbar curves, less loss of the postoperative correction achieved, and fewer revision surgeries. Posterior-only fusion with pedicle screws enabled a good and stable correction of severe scoliosis. However, severe curves may be amenable to hybrid instrumentation that produced analogous results to the screws-only constructs concerning patient satisfaction; at the latest follow-up, SRS-30 and SF-36 scores did not show any statistical differences between the two groups.
Keywords: Adolescent idiopathic scoliosis, Severe thoracic scoliosis, Surgical treatment, Posterior instrumented fusion only, Thoracic pedicle screws
Introduction
In the past, surgical treatment of severe thoracic idiopathic scoliosis consisted of posterior spinal fusion with Harrington instrumentation, combined with a consistent period of preoperative halo-traction and respiratory rehabilitation [40, 43]. Later, the most common treatment was anterior release with an open thoracotomy [10, 13, 26, 44, 46] followed by posterior instrumented fusion. Halo-traction between anterior release and posterior instrumentation was often applied [42]. Sometimes, in highly rigid scoliosis, this combined program was preceded by an additional posterior release [10].The correction rate of severe idiopathic curves with the combined treatment was 45–47%, using Harrington instrumentation [13] or the multiple hook construct [46], 52% using Zielke instrumentation with Harrington rod [26], and up to 67%, using anterior instrumentation and posterior hybrid construct [10]. The combined anterior and posterior procedure was performed in 1- or 2-stage surgery according to different authors with different outcomes. Shufflebarger et al. [46] found decreased hospital stay and operating time, fewer complications, and better correction in the continuous group compared to the staged group; more recently Shen et al. [45] concluded that there was no significant difference in safety or efficacy between the 1- or 2-stage groups.
Additional anterior surgery requires increased time for general anesthesia and may have a negative impact on pulmonary function. Kim et al. [25] recently reported that an open anterior approach may have a deleterious effect on pulmonary function for as long as 5 years postoperatively, after surgical treatment of adolescent idiopathic scoliosis. Video-assisted thoracoscopy (VAT), used for the anterior release, followed by posterior instrumentation for scoliosis treatment [2, 29, 36, 37] can minimize, but not eliminate, the negative effect on pulmonary function, as reported by Newton et al. [36].
Combined anterior and posterior vertebral column resection has been used more often [8, 9, 54] to treat congenital severe and rigid scoliosis and more rarely idiopathic curves. This demanding procedure was used by Bradford and Tribus [9] for seven patients with severe idiopathic curves (mean Cobb angle 91°), who achieved an average scoliosis correction of 59%. Suk et al. [53] presented the results of vertebral column resection at the apex of the deformity performed through a single posterior approach in 16 cases (six of them with idiopathic curves) in curves of more than 80° and with a flexibility of less than 25%; the procedure obtained a scoliosis curve correction of 59%, with severe complications in four cases.
Recently, some authors [3, 12, 14, 18, 27] have used posterior-only fusion for the treatment of severe thoracic adolescent idiopathic scoliosis (AIS). The correction rate of scoliosis was 53.9% using a hook-only construct [18], 54% with hybrid instrumentation [3], and 67–68% with pedicle screws only [14, 27]. Furthermore, two recent studies [20, 33] compared combined treatment (anterior and posterior fusion) versus posterior fusion only in severe AIS. Luhmann and Lenke [33] concluded that the patients treated with pedicle screw-only instrumentation presented similar results to patients with combined treatment (60.7 vs. 58.5%), without the negative effects on pulmonary function from anterior release. The aim of the present study was to assess the clinical and radiographic outcome of surgical treatment for severe thoracic (>80°) AIS by posterior spinal fusion alone (PSF). The patients were also divided into two subgroups based on the posterior construct used, pedicle screws-only or hybrid instrumentation (proximal hooks and distal pedicle screws).
Materials and methods
Patient evaluation
A retrospective review, based on a database search, was performed to identify all patients who had undergone a posterior spinal fusion alone between January 1996 and December 2000 at our department. The inclusion criteria were: (1) diagnosis of adolescent idiopathic scoliosis, (2) main thoracic curve (Lenke type 1, 2, 3, and 4) with preoperative Cobb ≥80°, (3) age between 11 and 20 years old at surgery, (4) no preoperative treatment such as halo-traction or serial corrective Risser’s plasters, (5) one-stage posterior instrumented fusion using third generation spinal instrumentation, (6) a minimum clinical and radiographic follow-up of 4.5 years.
An independent spine surgeon reviewed all the medical records and X-rays of the patients considered. Inpatient and outpatient charts were used for collecting demographic data, peri-operative treatment, and annotation of any medical and surgical-related complications, including revision surgeries. Radiographic evaluation included standing postero-anterior and lateral films on long-cassettes (90 × 30 cm), before and after surgery and at the latest follow-up. The Lenke et al. [28] surgical classification of AIS was used to describe curve patterns. Cobb measurements [16] of the major thoracic (MT) and compensatory lumbar (TL/L) curves were obtained, and the lateral films were evaluated for thoracic kyphosis (T5–T12), lumbar lordosis (superior endplate of L1 to inferior endplate of L5), and thoracolumbar sagittal alignment (T10–L2). Supine preoperative bending films of the major and compensatory curves were also used to determine flexibility. Supine preoperative radiographs were also performed in a corrective Risser plaster, held for few hours, to assess the correction rate in the plaster cast. Offset in the coronal plane was determined by measuring (in cm) the distance between the C7 plumb line and the perpendicular line drawn through the center of the S1 vertebral body [center sacral vertical line (CSVL)] (global coronal balance), the translation of the apical thoracic vertebra (AVT), as the distance between C7 plumb line and the center of the apical thoracic vertebral body or disc, the distance between CSVL and the apical lumbar vertebra (AVL), and finally the distance between CSVL and the lowest instrumented vertebra (LIV). The lowest instrumented vertebra tilt angle (LIV tilt) on the coronal plane (angle between an horizontal line and the lower endplate of LIV) was also assessed in degrees [38, 48]. MRI of the spine, including cervical, thoracic, and lumbar segments, was performed preoperatively to exclude congenital intramedullary anomalies.
A total of 52 consecutive patients (one single institution, three different surgeons) fulfilled our inclusion criteria. According to the type of posterior instrumentation used, two distinct treatment groups were identified: posterior spinal fusion with hybrid, proximal thoracic hooks and distal pedicle screws (PSF–H group, n = 27 patients), and pedicle screws-only instrumentations (PSF–S group; n = 25 patients).
Operative procedures
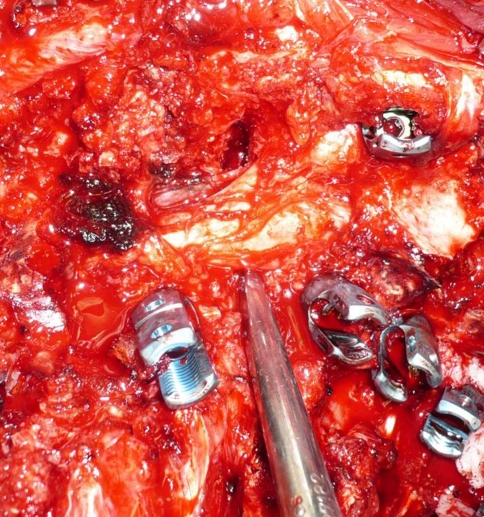
Somatosensory-evoked potentials were recorded during surgery in all patients of both groups; the wake-up test was performed intraoperatively only in four cases (three patients of group H, and one of group S) due to particular technical difficulties in acquiring the potentials. The same operating table was used in all patients. All cases underwent posterior instrumented fusion after a meticulous exposure of the posterior elements of the spine to the tips of the transverse processes bilaterally. Arthrodesis was carried out using banked bone (obtained from femoral epiphyses) and autologous chips obtained from resected ribs after thoracoplasty. In 25 of the 52 patients a posterior thoracoplasty was performed using the same midline incision, removing four ribs on average (range 3–5). A radical posterior release was performed in every case at each level to be fused. In curves of more than 100° a pedicle subtraction osteotomy was also performed at the apex of scoliosis (Fig 1).
Fig. 1.
In curves of more than 100° a pedicle subtraction osteotomy was also performed at the apex of scoliosis
For thoracic screw placement we used a technique already described in a previous paper by the present authors [19] that allowed for inspection with a spatula inside the canal of the superior, medial, and inferior borders of the pedicle. A mini-laminotomy was performed in the cephalad part of the lamina; after excision of the spinous process, the ligamentum flavum was completely removed with a small portion of the lamina in the upper part. Besides the spatula inside the canal, to determine the pedicle entry point the well-known anatomic landmarks were used [24, 51, 55, 56]. The presumed pedicle entry point was prepared with a rongeur. The pedicle was entered using a small curette. The instrument was inserted by applying mild pressure for 30 mm in the proximal thoracic pedicles, 35 mm in the mid-thoracic region, and 40 mm for the lower thoracic pedicles, directed along the axis of the pedicle in the frontal and sagittal plane. The screw tract inside the pedicle was checked with a pedicle sound to palpate five distinct bony borders: a floor and four walls. Metallic pins were inserted in the thoracic holes. Fluoroscopy was performed. Pedicle screws were inserted with slow and gentle force using a screw diameter corresponding to about 80% of the pedicle diameter [51, 52]. The screw length corresponded to about 70% of the vertebral body on lateral view of fluoroscopy. The direction of the screw was more convergent medially in the upper thoracic spine, convergent in the mid-thoracic spine, and quite straight at T11 and T12 level. Screw placement was confirmed by fluoroscopy, using the AP, lateral, and oblique views. The oblique view permitted a further check for screw placement inside the pedicle and also to check the tip of the screw and the anterior border of the vertebral body. That way, if the tip of the screw presented beyond the anterior border of the body, it was immediately removed, its tract palpated, and a new screw inserted with the appropriate shorter length.
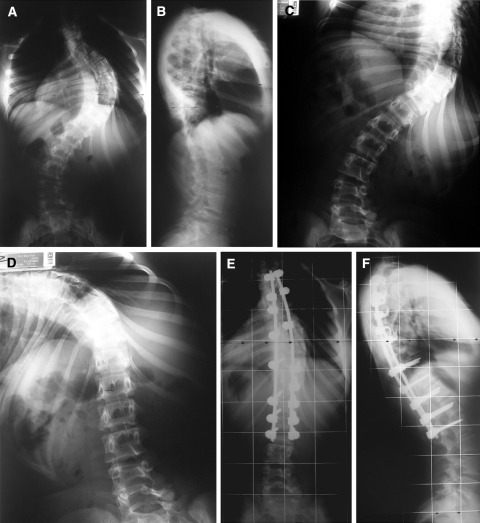
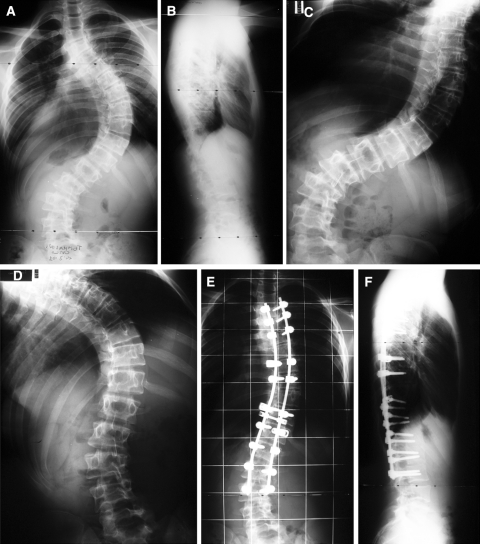
In the PSF–H group (Fig. 2), instrumentation consisted of an average of 6.5 hooks (range 5–9) and an average of 8.5 pedicle screws (range 6–10); instrumentation extended from T1 in two cases, T2 in one patient, T3 in 19, and T4 in five cases, to L1 in one patient, L2 in six cases, L3 in 16 and L4 in four. In the PSF–S group (Fig. 3), instrumentation included an average of 13.5 screws (range 10–21), and extended from T3 in ten cases, T4 in 12, T5 in three, to T12 in one case, L1 in four, L2 in six, L3 in eight and L4 in six.
Fig. 2.
PM, 13-year-old female. Risser 1. AIS: right thoracic (90°) and left lumbar (60°), Lenke type 1CN curve (a, b). In supine side flexion radiographs thoracic and lumbar curves bended out to 65° and 20°, respectively (c, d). X-rays control 4 years after hybrid posterior spinal fusion (thoracic curve correction to 25° and lumbar to 15°) (e, f)
Fig. 3.
CT, 15-year-old female. Risser 3. AIS: right thoracic (94°) and left lumbar (56°), Lenke type 3BN curve (a, b). In supine side flexion radiographs thoracic and lumbar curves bended out to 66° and 42°, respectively (c, d). X-rays control 3 years after pedicle screw-only posterior spinal fusion (thoracic curve correction to 40° and lumbar to 35°) (e, f)
Deformity correction was carried out using a combination of different corrective techniques, including rod cantilevering, translational techniques, and concave rod rotation maneuver. The operation time averaged a mean of 270 min in the PSF–H group (range 180–350 min) and 380 min in the PSF–S group (range 240–400 min). Mean perioperative bleeding was 850 ml (range 500–1,300 ml) in the PSF–H, and 900 ml (range 250–1,500 ml) in the PSF–S group, with a mean estimated blood loss of 15.4 and 16.7 cc/kg, respectively. No postoperative brace or a cast was prescribed in any of the patients.
Questionnaires
Two self-reported, patient-based outcome tools, the Italian version of the SF-36 questionnaire [1] and of the SRS-30 [4, 5] were mailed to all patients during this retrospective review. Statistical analysis was performed using the t test (paired and unpaired), the Wilcoxon test for non-parametric paired analysis, and the Mann–Whitney test for non-parametric unpaired analysis. Results are expressed as the mean (range), with a P value of <0.05 considered as being statistically significant.
Results
We were able to review the entire series of 52 cases at an average follow-up of 6.7 years (range 4.5–8.5 years). There were no statistical differences between the two groups in terms of age, Risser’s sign, curve patterns according to Lenke’s classification, Cobb preoperative main thoracic (MT) curve magnitude and flexibility on supine side bending and in Risser’s plaster cast, secondary lumbar (TL/L) curve and its flexibility (Table 1), sagittal preoperative contour, and offset measurements on the coronal plane (Tables 2, 3).
Table 1.
Posterior spinal fusion: pedicle screws versus hybrid
| Coronal Cobb angle measurements | PSF–S | PSF–H | Significance |
|---|---|---|---|
| Main thoracic curve preop | 88° (80–136) | 92° (80–135) | NS |
| Preop side-bender main thoracic | 66° (54–110) | 67.18° (50–101) | NS |
| Flexibility main thoracic curve | 25.62% (12.79–35.29) | 27.23% (16–44) | NS |
| Supine Risser cast main thoracic | 58.43° (43–95) | 60.25° (45–90) | NS |
| Main thoracic curve follow-up | 40° (20–105) | 51° (25–90) | P = 0.002 |
| Final main thoracic curve correction | 52.4% (22.79–75) | 44.52% (17.58–72.22) | P = 0.001 |
| Main thoracic curve post surgical loss (final-postoperative) | −1.9° (−5.3 to 0) | −11.3° (−44.23 to 0) | P = 0.0005 |
| Secondary lumbar curve preop | 57.19° (34–80) | 52° (27–90) | NS |
| Flexibility secondary lumbar curve | 32.7% (10–50) | 29.6% (13–70) | NS |
| Secondary lumbar curve postop | 29° (5–62) | 28° (10–72) | NS |
| Secondary lumbar curve follow-up | 29° (5–62) | 29.7° (10–68) | NS |
| Final secondary lumbar curve correction | 50.05% (20.5–86.8) | 43.35% (4.4–75.6) | NS |
| Secondary lumbar curve post surgical loss (final-postoperative) |
0% (−12 to 13.04) | 4% (−12.5 to 28.5) | 0.03 |
Table 2.
Posterior spinal fusion: pedicle screws versus hybrid
| Sagittal Cobb angle measurements | PSF–S | PSF–H | Significance |
|---|---|---|---|
| T5–T12 preop | 35.32° (0–78) | 35.22° (7–80) | NS |
| T5–T12 postop | 26° (10–60) | 29.3° (9–50) | NS |
| T5–T12 final | 28.4° (12–60) | 32.4° (10–50) | NS |
| T10–L2 preop | 13.08° (−10 to 85) | 11.81° (−18 to 60) | NS |
| T10–L2 postop | 4.48° (−15 to 70) | 6.7° (−10 to 22) | NS |
| T10–L2 final | 5.4° (−10 to 65) | 8.11° (−10 to 22) | NS |
| L1–L5 preop | −45.9° (−70 to −15) | −44.37° (−80 to −20) | NS |
| L1–L5 postop | −41.88° (−70 to −15) | −40.67° (−80 to −15) | NS |
| L1–L5 final | −46.88° (−70 to −30) | −40.85° (−65 to −20) | NS |
Table 3.
Posterior spinal fusion: pedicle screws versus hybrid
| Coronal offset measurements | PSF–S | PSF–H | Significance |
|---|---|---|---|
| Global coronal balance (C7–S1) preop (cm) | 1.1 (0–3.9) | 1.35 (0–4) | NS |
| Global coronal balance (C7–S1) postop (cm) | 0.98 (0–4) | 1.22 (0–3.4) | NS |
| Global coronal balance (C7–S1) follow-up (cm) | 0.44 (0–2) | 0.7 (0–2.5) | NS |
| Translation of the apical thoracic vertebra preop (cm) | 6.03 (2.6–9) | 7.11 (2.8–12) | NS |
| Translation of the apical thoracic vertebra postop (cm) | 3.06 (0–8) | 3.55 (0–9.5) | NS |
| Translation of the apical thoracic vertebra follow-up (cm) | 3 (0.2–7) | 4.07 (0.5–10) | 0.05 |
| Surgical overall change (preop-final) AVT | −3.03 (−0.3 to 5.5) | −3.04 (0.8 to 6.7) | NS |
| Translation of the apical lumbar vertebra preop (cm) | 2.48 (0–7) | 1.45 (0–6.5) | NS |
| Translation of the apical lumbar vertebra postop (cm) | 1.61 (0–4) | 1.02 (0–4) | NS |
| Translation of the apical lumbar vertebra follow-up (cm) | 1 (0–3.3) | 0.95 (0–4.5) | NS |
| Surgical overall change (preop-final) AVL | −1.49 (0.5 to −5) | −0.5 (1.8 to −2) | 0.02 |
| Translation of the lowest instrumented vertebra preop (cm) | 1.92 (0–5.2) | 1.32 (0–4) | NS |
| Translation of the lowest instrumented vertebra postop (cm) | 1.28 (0–4) | 0.94 (0–2) | NS |
| Translation of the lowest instrumented vertebra follow-up (cm) | 0.92 (0–3) | 0.77 (0–3) | NS |
| Surgical overall change (preop-final) LIV translation | −1.00 (0.5 to −3.2) | −0.55 (0.7 to −1.5) | 0.04 |
| Tilt of the lowest instrumented vertebra preop (degrees) | 24.08 (0–60) | 19.96 (4–42) | NS |
| Tilt of the lowest instrumented vertebra postop (degrees) | 9.24 (0–40) | 8.48 (0–30) | NS |
| Tilt of the lowest instrumented vertebra follow-up (degrees) | 7.54 (0–40) | 8.00 (0–36) | NS |
| Surgical overall change (preop-final) LIV tilt | −19° (−14 to −22) | −10° (−6 to −17.5) | 0.005 |
The PSF–H group (n = 27 patients) consisted of 23 female and 4 male patients, with a mean age at surgery of 14.9 years (11–20), and a mean Risser’s sign of 2.34 (0–5). The curve patterns according to the Lenke’s classification were 11 (40%) type 1, 9 (33.3%) type 2, 3 (11%) type 3, and 4 (15%) type 4. In this group we observed a preoperative main thoracic Cobb of 92° (80–135), which bent down to 67.18° (50–101), with a flexibility of 27.23% [16–44], being corrected on average to 60.25° (45–90) in the Risser’s cast preoperative test, and achieved a follow-up correction down to 51° (25–90), for a final correction of 44.52% (17.58–72.22), and a mean loss of −11.3° (−44.23–0) (Table 1).
The PSF–S group (n = 25 patients) had 16 female and 9 male patients, with a mean age at surgery of 16.4 years (11–20), and a mean Risser’s sign of 3.04 (0.5–5). The curve patterns according to the Lenke’s classification were 9 (36%) type 1, 9 (36%) type 2, 3 (12%) type 3, and 4 (16%) type 4. The PSF–S group showed a preoperative Cobb of 88° (80–136), bent down to 66° (54–110), with a flexibility of 25.62% (12,79–35,29), being corrected on average to 58.43 (43–95) in the Risser’s cast preoperative test, final correction down to 40° (20–105); an overall correction of 52.4% (22.79–75), and an average loss of −1.9° (−5.3 to 0) (Table 1).
In conclusion, the pedicle screws group compared to the hybrid group, both showed a significantly greater final correction (P < 0.001) and a significantly better maintenance of the initial correction (P < 0.0005) of the main thoracic curve (Table 1). The PSF–S group had a greater TL/L final correction compared to the PSF–H group (50.05 vs. 43.35%), without reaching a statistically significant difference.
Concerning the coronal balance radiographic measurements (Table 2), we observed the same aforementioned trend of better results in the PSF–S group, with less final apical MT vertebra translation (PSF–S: 3.0 cm vs. PSF–H: 4.07 cm; P = 0.05), a greater overall change (preop-final) both of the apical TL/L vertebra translation (PSF–S: −1.48 cm vs. PSF–H: −0.49 cm; P = 0.02), LIV coronal translation (PSF–S: −1.00 cm vs. PSF–H: −0.54 cm; P = 0.04), and LIV coronal tilt (PSF–S: −19° vs. PSF–H −10°; P = 0.005).
We found no statistically significant differences between the two groups in terms of both sagittal contour and global coronal alignment, with no patients decompensated in the final follow-up (Tables 2, 3).
The thoracic kyphosis T5–T12 angle was similar in each group before surgery (PSF–S 35.32° vs. PSF–H 35.22°), immediate postoperative (26° vs. 29.3°), and at final follow-up evaluation (28.4° vs. 32.4°). The thoracolumbar T10–L2 angle was similar in each group before surgery (13.08° in PSF–S group and 11.81° in PSF–H group). The immediate postoperative thoracolumbar contour averaged 4.48° in PSF–S group and 6.7° in PSF–S group. Thoracolumbar alignment at the latest follow-up averaged 5.4° and 8.11°, respectively. Lumbar lordosis was similar in each group before surgery (PSF–S: −45.9° vs. PSF–H −44.37°), in the immediate postoperative (−41.88° vs. −40.67°), and at the final follow-up evaluation (−46.88° vs. −40.85°).
Concerning the extension of the area of fusion, this was shorter on average by one level in the PSF–S group with 11.84 levels (range 9–14) versus 12.89 (range 12–15) (P < 0.002) in the PSF–H group. The free levels below the fusion were on average 3.48 (range 2–6) in the PSF–S screw group versus 3.11 (range 1–5) (P = 0.04) in the PSF–H group.
Younger patients
We further examined separately the results obtained in 11 younger patients (with a Risser’s sign of 0–1) of the 52 reviewed. Nine of them were in the PSF–H group and two in the PSF–S group. These 11 patients were all premanarche females with a mean age of 12.1 (11–13). There were no cases of crankshaft phenomenon or decompensation. Furthermore, none of these younger patients required revision surgery at a mean follow-up of 61.7 months (range 55–122) (Table 5).
Table 5.
Posterior spinal fusion in Risser 0–1 patients (11 cases)
| Coronal Cobb angle measurements | Mean (range) | Significance |
|---|---|---|
| Age | 12.18 (11–13) | NA |
| Risser’s sign | 0.4 (0–1) | NA |
| Follow-up (in months) | 61.7 (36–122) | NA |
| Main thoracic curve preop | 95.6° (80–130) | NA |
| Preop side-bender main thoracic | 69.8° (50–100) | NA |
| Flexibility main thoracic curve | 27.27% (21.05–44.44) | NA |
| Main thoracic curve postop | 46.7° (20–87) | P = 0.000* |
| Main thoracic curve follow-up | 49° (25–87) | P = 0.000** |
| Postoperative main thoracic curve percent correction | 51.14% (27.1–77) | NA |
| Final main thoracic curve percent correction | 48.76% (23.9–72.22) | NS*** |
| Main thoracic curve post surgical loss (final-postoperative) | 2.27° (0- 5) | NS*** |
| Kyphosis T5–T12 preop | 35.72° (7–80) | NA |
| Kyphosis T5–T12 postop | 27.54° (9–42) | NS* |
| Kyphosis T5–T12 follow-up | 31.45° (12–50) | NS** |
| Kyphosis T5–T12 post surgical change (final-postoperative) | 3.9° (3–8) | NS*** |
| Global coronal balance (C7–S1) preop (cm) | 1.17 (0.2–4) | NA |
| Global coronal balance (C7–S1) postop (cm) | 1.21 (0.2–2.5) | NS* |
| Global coronal balance (C7–S1) follow-up (cm) | 0.76 (0–2.1) | NS** |
NA not applicable, NS not statistically significant,*NS not statistically significant post versus pre, **NS not statistically significant final versus pre, ***NS not statistically significant post versus final
Pedicle substraction osteotomy cases
A pedicle subtraction osteotomy (Fig. 1) was performed at the apex of scoliosis in seven patients, two from the PSF–H group and five from the PSF–S group, presenting a main thoracic curve with a Cobb angle superior to 100°.
A wide laminectomy was performed over the apical level with the entire lamina of the cephalad and caudad vertebrae being removed. Then, the pedicles to be resected were encircled and removal of the vertebral body was started (more aggressive on the convexity of the curve) by means of straight and curved curettes through a lateral pedicle-body entrance. Finally a posterior-based closing wedge osteotomy was performed. It was very important to minimize epidural and osseous blood loss during these surgeries, not only with careful subperiosteal stripping of the posterior vertebral elements, but also with the continuous use of adjunctive hemostatic agents.
The seven patients included five females and two males, with a mean preoperative thoracic curve of 113° (range 100°–135°), which bent down to 85° (range 75°–101°), with a flexibility of 22.62% (range 10°–35.29°), final correction down to 68° (range 48°–90°); overall correction was 58.6% (range 37–69%). The mean estimated perioperative blood loss in this series of patients was 17.45 cc/kg, ranging from 7.7–27.27 cc/kg. In this group of seven patients no complications were observed.
A further statistical analysis was performed, excluding these seven “osteotomy group” patients, on a total number of 45 patients, 25 hybrid and 20 pedicle screw patients. No statistically significant difference was found in any parameter (preoperative, postoperative, and final radiographic measurements), with respect to the entire series. The same trend of better results in the pedicle screws group was observed, with the same radiographic parameters reaching a similar statistically significant difference, when compared to the hybrid group.
Questionnaires
SRS-30 scores and SF-36 scores were available in 47 of 52 patients, at the last follow-up. Pre- to postoperative comparison of SRS scores could not be performed since the majority of the patients in both groups had undergone surgery before an Italian version of the SRS-30 questionnaire was available. The SRS pain domain was found to correlate well with the SF-36 bodily pain domain; correlation was found also for the function domain with the SF-36 physical role domain [5, 6]. At the latest follow-up, SRS-30 and SF-36 findings were similar between the two groups, with mean scores shown in Table 4. This came from similar global coronal and sagittal balance, which patients could easily recognize.
Table 4.
Posterior spinal fusion: pedicle screws vs hybrid
| Patient-based outcome tools (follow-up) | PSF–S | PSF–H | Significance |
|---|---|---|---|
| SRS pain | 4.16 | 4.23 | NS |
| SRS self-image | 3.84 | 3.46 | NS |
| SRS function | 3.54 | 3.25 | NS |
| SRS mental health | 4.02 | 3.63 | NS |
| SRS satisfaction | 4.1 | 4.36 | NS |
| SRS total score | 3.91 | 3.76 | NS |
| SF-36 physical function | 85 | 78.57 | NS |
| SF-36 role physical | 67.5 | 57.14 | NS |
| SF-36 bodily pain | 70.25 | 66.79 | NS |
| SF-36 general health | 71.6 | 72.57 | NS |
| SF-36 vitality | 70 | 69.29 | NS |
| SF-36 role emotional | 73.27 | 66.6 | NS |
| SF-36 social function | 70 | 75 | NS |
Complications
At the latest follow-up we found no fatal complications or neurologic injuries, either acute or delayed deep wound infection in this case series.
Hybrid group
In the hybrid series (27 patients) seven surgery-related complications in seven patients (25.9%) required three revision surgeries in three patients (11.1%).
A 15-year-old girl, presented a substantial loss of correction due to upper hook dislodgement with skin prominence, and was successfully treated by means of hook replacement at 3.6 years after the index procedure. Another 15-year-old girl presented with a pseudarthrosis, 7 years after the first surgery, producing a significant loss of correction. She underwent a revision procedure with an extension of the instrumentation/arthrodesis to one level below. The third revision surgery was performed on a 17-year-old girl who complained 7.6 years postoperatively of late operative site pain, and persistent rib hump deformity; in this case implant removal and posterior thoracoplasty were performed, as a solid fusion mass was detected intraoperatively.
An adding-on phenomenon was observed in a 15-year-old boy with an increase of the fractional curve below the arthrodesis, performed down to L3. The proposed revision procedure extending the arthrodesis was refused by the parents; at 6 years’ follow-up he was doing well and his fractional curve was stabilized.
The remaining three implant-related complications were due to upper hook displacement in two patients and lower pedicle screw loosening in a third one. These mechanical failures did not produce any loss of correction or pain, and did not require revision procedure.
Pedicle screws group
In the pedicle group series (25 patients) 11 surgery-related complications in 11 patients (44.0%) required one revision surgery in one patient (4.0%).
The revision surgery was performed 2.7 years after the index procedure. This patient was a 17-year-old girl, who presented with an upper convex site pedicle screw pull-out and persistent rib hump, which represented a serious concern for her. She was treated by means of pedicle screw replacement and posterior thoracoplasty between T5 and T9.
As for the hybrid group, we observed an adding-on phenomenon in a 16-year-old girl with a T4–L3 arthrodesis. Revision surgery was refused by her parents, and at the latest follow-up of 5 years she was free of pain and the fractional curve was stabilized.
In the pedicle screw group there were other complications, including dural lesions in four patients and thoracic screw misplacement in five cases, which did not require revision surgeries.
Dural lesions occurred in four out of the 25 patients of group PSF–S (16%), shown by the leakage of cerebrospinal fluid while preparing the screw holes. They all occurred when entering concave thoracic pedicles, while using the small currette, at T5 in one case, at T6 in one case, T7 in one case, and at T8 in one patient. A hemilaminectomy was performed immediately to have a direct view of the lesion and repair it rapidly with suture thread and fibrin glue. No spinal fluid leaks were noted postoperatively. In all cases the dural tear was a small hole.
Screw misplacement at thoracic level was suspected, on postoperative X-rays, when a different screw angulation, with respect to the other screws, was present. A postoperative CT, using established 2-mm increments, was performed in only 12 of the 25 patients (48%), when standard and oblique postoperative radiographs had raised well-founded doubts regarding the positioning of a total of 29 thoracic screws, (intrapedicular, 0 to <2 mm pedicle breach, 2 to <4 mm of breach, >4 mm breach) [7]. The total number of screws examined by CT was 128. In five patients, five thoracic screws (one screw for each patient) were found to be misplaced, as confirmed by CT. Screw malposition did not present evidence of risks and did not cause any symptoms. The positions of these five malpositioned screws were: one screw in T3, one in T4, one in T5, one in T6 and one in T7. The malposition was always lateral, three positioned on the concavity and two on the convexity of the curves. These malpositioned screws presented a moderate lateral cortical perforation (with pedicle breach between 1.0 and 2.0 mm) and were not in proximity to the aorta or any other principal vessel (with a distance of more than 5 mm): consequently, it was decided to leave the misplaced screws in place. At a mean follow-up of 6.5 years (range 4.5–7 years), there were no changes in the X-ray control and no symptoms.
Discussion
The use of thoracic pedicle screws has reassessed the role of posterior-only fusion as treatment for severe thoracic AIS.
Previous studies used posterior-only instrumentation with multiple hooks [18] or hybrid construct [3, 12]. De Giorgi et al. [18] used CD instrumentation in 19 cases of idiopathic scoliosis between 80° and 145°, and achieved a correction of 53.9%. The instrumentation had only hooks and, in some cases, was preceded by halo-traction or elongation cast, and required a postoperative cast or a brace for 3 months. The crankshaft phenomenon occurred in a girl of 11 years old and a distal hook dislodged in another case. A hybrid construct (a varied combination of hooks, wires and screws) was used by Burton et al. [12] in the treatment of 46 patients with adolescent idiopathic scoliosis and thoracic curves between 70° and 90°. They achieved an average curve correction of 64% and reported one pseudarthrosis and one lower hook dislodgement as complications, requiring in both cases a new operation. The conclusion of the authors was that curves between 70° and 90° do not need anterior release to achieve acceptable results. The hybrid construct (thoracic hooks and lower screws) has been used also by Arlet et al. [3] in 15 cases with thoracic scoliosis between 70° and 90° and achieved 54% correction at a mean follow-up of 32 months.
However, it was the use of thoracic pedicle screws that increased the interest for posterior fusion alone in deformity correction of large-magnitude scoliosis. The first to report on thoracic screws in idiopathic scoliosis was Suk et al. [50], more than 10 years ago, albeit in mild curves. Recently, Chang [14] used posterior pedicle screws-only instrumentation in 26 cases with thoracic scoliosis between 75° and 135°. The cantilever bending technique achieved a correction of 67%. Kuklo et al. [27] used 352 thoracic screws in 20 patients (17.6 screws/case) to correct idiopathic scoliosis over 90° and achieved 68% correction. The scoliosis correction rate of these two studies [14, 27] adopting pedicle screws, was surprisingly high, similar to that achieved by Bullman et al. [10] using a combination of anterior instrumentation and a posterior hybrid construct. Most of the literature on the surgical treatment of severe idiopathic thoracic curves shows more contained values, generally lower than 60% regardless of the technique used [3, 9, 26, 53, 54]. In severe thoracic scoliosis the aim should not be to maximize the curve correction, but to obtain an acceptable balance of the spine and save levels of fusion. In fact, at the latest follow-up, all 52 patients in our series had a mean global coronal balance of 0.44 cm (range 0–2) for PSF–S patients and 0.7 cm for the PSF–H group (range 0–2.5). This good spine balance corresponded to good patient satisfaction; a mean SRS-30 satisfaction of 4.1 in the PSF–S group and 4.3 in the PSF–H group. For a better cosmetic result (which is very important for our young patients) in most cases we used a posterior thoracoplasty. Furthermore, the risks of a too aggressive posterior-only correction not preceded by an anterior release should not be underestimated. Overdistraction should be avoided due to the risk of spinal cord ischemia [17]. In the past, it was reported that an intraoperative correction exceeding the preoperative bending correction was one of the factors related to an increased risk of spinal cord injury [58].
Our correction rate achieved using hybrid instrumentation was lower than that obtained using the screws-only construct (44.52 vs 52.4%) and presented more loss of correction at final follow-up (−11.3° vs. −1.9°), in agreement with other authors in the treatment of severe thoracic scoliosis [19, 33]. Furthermore, the PSF–S group had a greater TL/L final correction compared to that of the PSF–H group. Concerning the coronal balance, there was the same trend of better results in the PSF–S group, with less final apical MT vertebra translation, a greater overall change (preop-final) both of the apical TL/L vertebra translation, LIV coronal translation, and LIV coronal tilt. In addition, the extension of the fusion area was shorter by an average of one level in the PSF–S group.
However, hybrid constructs can be certainly considered for the treatment of severe scoliosis. The authors concur that severe curves may be amenable to hybrid instrumentation, which has produced results similar to those of the screw-only construct with regards to patient satisfaction. At the latest follow-up, SRS-30 and SF-36 scores did not show any statistical differences between the two groups. This lack of significant difference was due to a similar global coronal and sagittal balance, which patients could easily recognize. Therefore, despite large and stiff curves, cosmesis can be improved by posterior instrumentation alone [11]; these results are consistent with previous reports [5, 6, 11, 33], although comparison is somewhat difficult because of the different instrumentation used throughout the literature. Furthermore, in favor of the hybrid construct, there is a longer operation time with the screws-only construct and a higher incidence of surgery-related complications in the screws group (44.0 vs. 25.9%), represented more often by dural lesions and misplaced screws, which however did not require a revision surgery. Dural lesions were repaired immediately and no spinal fluid leaks were noted postoperatively. Furthermore, five thoracic screws were found to be misplaced. These screws did not show any signs of risk and did not cause any symptoms, and consequently it was decided to leave the misplaced screws in place. They were screws with a moderate lateral cortical perforation (with a pedicle breach between 1.0 and 2.0 mm), which up to the last follow-up had not caused any complications. Conversely, a higher rate of revision surgeries was found in the hybrid group (11.1 vs. 4.0%), including among others pseudoarthosis in one 13-year-old patient.
Thoracic screw fixation can be potentially dangerous in the surgical treatment of scoliosis [35, 55]. The technical difficulties in scoliotic deformities have been emphasized [7]. In severe scoliosis placement of thoracic screws may present further difficulties. However, the biomechanical advantages associated with their use, make screws the ideal construct in large curves [27]. Thoracic screws on the concavity are the crucial anchor points for better scoliosis correction and restoring thoracic kyphosis [49]. Instead, the use of hooks at the apex of severe scoliosis was proved to be unreliable, besides being dangerous; they are inside the canal and are thus invasive. It has been found that canal intrusion of a medially placed screw (with 3-mm breach) is less invasive than a perfectly positioned pediatric laminar hook [41]. Therefore, hooks can be sometimes more dangerous than screws, because of their position, and cause complications themselves [6]. Furthermore, hooks ensure a less rigid fixation, which can lead to dislocation during correction maneuvers or subsequently [49], due to hook pullout with laminar fractures.
Severe complications related to screw over-penetration in the thoracic cavity have been reported in scoliosis treatment [15, 34], but they involve only two cases in the literature out of nearly 1,000 patients [7, 24, 27, 30, 31, 51] treated all together by means of almost 9,000 thoracic screws; in these large series of not severe scoliosis treated using thoracic pedicle screws, however, the authors report less severe complications such as small hematoma [30] or spontaneous pneumothorax [51], not directly related to a pedicle screw. In the series of severe scoliosis treated with thoracic pedicle screws [14, 27], as also in our series, no complications caused by intra-thoracic screws have been reported. However, when screws are in proximity of the thoracic aorta’s wall (less than 5 mm) there is the risk of a subsequent vascular lesion, and a CT scan with intravenous contrast or an aortograph is recommended before the removal of the screw [47].
Neurological complications are rarely reported in the literature in thoracic scoliosis treatment with pedicle screws [39, 51], although medially positioned thoracic screws are quite commonly reported. Kuklo et al. [27] reported screw accuracy of 96.3% in severe scoliosis by postoperative CT scanning. Ten screws had a breach of between 2 and 4 mm (three medial and seven lateral), while in three screws it was >4 mm (two medial and one lateral). The two medial screws (0.57%) were the only ones removed, although there were no neurological complications. However, the authors claimed that these screws would not be removed nowadays. We agree with this claim. In fact, even now their acceptability remains controversial [7]. According to some authors [30] medial wall penetration equal to or less than 2 mm is well tolerated and the screws can be considered acceptably positioned. Other authors [21] have hypothesized a 4 mm “safe zone” of medial encroachment (2 mm of epidural space and 2 mm of subarachnoid space). Others [24] hypothesize a “definite safe zone” within 2 mm and “probable safe zone” within 2 and 4 mm, and a “questionable safe zone” of 4–8 mm of medial encroachment. Recently, however, Liljenqvist et al. [32] showed with magnetic resonance imaging that the width of the epidural space was less than 1 mm at the thoracic apical level on the concave side. This means that there is no safety zone on the concavity and therefore screw placement, especially at this level should be very precise.
To make thoracic pedicle screw placement safer various techniques are used. These include the “anatomical” techniques such as the free hand method [24] and the open-lamina technique [59]. The latter provides direct visualization of the medial wall of the pedicle. Flavotomy and laminotomy have been performed for pedicle screw insertion in severe idiopathic scoliosis [3], to visualize the medial border of the pedicle for safer screw insertion. A similar method to the open-lamina technique, but more economical in resecting the lamina, is the technique used by the present authors in recent years and in this series, called the mini-laminotomy [19, 23], which allows palpation with a spatula inside the canal of the borders of the thoracic pedicles. Furthermore, in severe scoliosis fluoroscopy is not always helpful and may lead the surgeon to evaluation errors due to severe vertebral body rotation.
When performing posterior fusion alone, a wide posterior release should be performed at each level, which should be more aggressive, especially at the level of the apex of the scoliosis. Therefore, the mini-laminotomy procedure (i.e., excision of the spinous process, and complete removal of the yellow ligament with a small portion of the upper part of the lamina) is the first step of the posterior release, which is completed later during surgery when the screws have been placed. Posterior release is fundamental to improve the chances of correcting scoliosis, especially when screw fixation is performed. Apical Smith–Petersen osteotomies have been performed by some authors [20] for thoracic scoliosis more than 110° on the preoperative standing X-rays with a residual curve equal to or greater than 80° on side bending radiographs. In curves of more than 100° a pedicle subtraction osteotomy was also performed at the apex of scoliosis (Fig. 1), in seven patients (two from the PSF–H group and five from the PSF–S group), to enhance a better curve correction. A mean preoperative thoracic curve of 113° (range 100°–135°), with a flexibility of 22.62% (range 10°–35.29°), showed a final average Cobb angle of 68° (range 48°–90°) with an overall correction of 58.6% (range 37–69%). When a subanalysis on the remaining 45 patients without osteotomy (25 hybrid and 20 pedicle screw patients) was performed, no difference on results with respect to the entire series was found, meaning that apical pedicle subtraction osteotomy did enhanced a better curve correction without altering in a statistically significant way the trend versus a better correction by means of pedicle screws with respect to hybrid instrumentation.
There is still some concern about performing a posterior fusion alone in younger patients (under 11 years old). In our series of 52 patients, there were 11 patients, all premanarche females with a Risser’s sign inferior to one (average: 0.4; range 0–1), mean age 12.1 (11–13), two in the pedicle screw group and nine in the hybrid group. The crankshaft phenomenon was not observed and the average loss of scoliosis correction was 2.27 (range 0–5) (Table 5). This is an important result, since most of them were treated by hybrid instrumentation, as with eight premenarcheal cases of Arlet’s series [3]. This suggests that a stiffer posterior construct with many screws might prevent the crankshaft phenomenon even in younger patients with idiopathic scoliosis, thus avoiding anterior fusion, as advocated by some authors [3, 11]. Furthermore, in young children pedicle screw fixation was found to be the only procedure to provide a secure anchorage in short segment instrumentation [22]. Larger studies and a longer follow-up will be needed, however, to assess the efficacy of posterior-only fusion with pedicle screws in severe scoliosis in younger patients.
The definition of how large or stiff a curve must be to require an anterior stage is an ongoing debate in the literature. According to some authors, adolescent idiopathic thoracic curves of about 85° or less and 35% or more flexibility can be treated with posterior fusion only [11]. Others [3], on the other hand, believe that larger and stiffer curves of more than 90° or with a side bend of less than 65° still require anterior release followed by posterior instrumentation, and often a halo-traction period; posterior-only fusion can instead be used in curves up to 90° which bend to less than 65°. Some authors [42] advocate single-stage posterior procedure for curves up to or exceeding 100°. We believe that a wide posterior release and a pedicle subtraction osteotomy at the apex of the deformity associated with a pedicle screws-only instrumentation might enable the use of posterior-only fusion also in stiffer curves. Traction films seem to be more useful than supine side bending films in decision making on the necessity of performing an anterior release [57]. We believe that for stiffer curves the preoperative Risser cast, maintained as long as necessary to perform supine X-rays, is more suitable. In this way, an immediate indication is obtained on the flexibility of the curve and confirmation that treatment can be performed by posterior fusion alone, which in our series was used for curves up to 136°.
Conclusions
The present series should be interpreted in the context of its limitations, including the retrospective nature of the review and the fact that patients were not randomized between hybrid and pedicle screw instrumentation: the orientation toward the use of pedicle screws-only construct has been gradual. However, this series is consecutive, with no statistical differences between the two groups in terms of age, Risser’s sign, Cobb’s preoperative main thoracic curve magnitude and flexibility, secondary lumbar curve and its flexibility, sagittal preoperative contour, and offset measurements on the coronal plane. These findings may serve to reduce some of the potential selection bias associated with non-randomized studies.
In this series of 52 patients, we assessed the results of posterior spinal fusion alone for severe thoracic (>80°) AIS and compared the results of posterior fusion with hybrid construct (proximal hooks and distal pedicle screws) versus pedicle screw instrumentation, at an average follow-up of 6.7 years (range 4.5–8.5 years).
The screw group, compared to the hybrid group, had a better MT final correction rate of 52.4 versus 44.52% (P = 0.001), and a smaller loss of correction at final follow-up (−1.9° vs. 11.3°, P < 0.0005). Furthermore, the PSF–S group had a greater TL/L final correction compared to the PSF–H group (50.05 vs. 43.35%), without reaching a statistically significant difference. Concerning the coronal balance, there was the same trend of better results in the PSF–S group, with less final apical MT vertebra translation (PSF–S: 3.0 cm vs. PSF–H: 4.07 cm; P = 0.05), a greater overall change (preop-final) both of the apical TL/L vertebra translation (PSF–S: −1.48 cm vs. PSF–H: −0.49 cm; P = 0.02), LIV coronal translation (PSF–S: −1.00 cm vs. PSF–H: −0.54 cm; P = 0.04), and LIV coronal tilt (PSF–S: −19° vs. PSF–H: −10°; P = 0.005).
Screw-only constructs presented a higher incidence of surgery-related complications (44.0 vs. 25.9%), represented by dural lesions and misplaced screws, which however did not require a new surgical operation; conversely one revision surgery (4%) was performed on a girl 2.7 years after the index procedure. A higher rate of revision surgeries instead was found in the hybrid group (11.1%), including among others a pseudoarthosis in one 13-year-old patient.
Posterior-only fusion with pedicle screws permitted a satisfactory and stable correction of severe thoracic AIS. However, even hybrid constructs can be certainly considered for the treatment of severe scoliosis; severe curves may be amenable to hybrid instrumentations, which have provided results similar to those of screw-only constructs with regards to patient satisfaction.
At the latest follow-up, SRS-30 and SF-36 scores did not show any statistical differences between the two groups. Therefore, despite large and stiff curves, cosmesis can be improved by posterior instrumentation alone.
References
- 1.Apolone G, Mosconi P, Ware JE (1997) Questionario sullo stato di salute SF-36. Guerini e Associati Milano
- 2.Arlet V. Anterior thoracoscopic spine release in deformity surgery: a metaanalysis and review. Eur Spine J. 2000;9:S17–S23. doi: 10.1007/s005860000186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arlet V, Jiang L, Ouellet J. Is there a need for anterior release for 70–90° thoracic curves in adolescent scoliosis. Eur Spine J. 2004;13:740–745. doi: 10.1007/s00586-004-0729-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Asher MA, Min Lai S, Burton DC. Further development and validation of the Scoliosis Research Society (SRS) outcomes instrument. Spine. 2000;25:2381–2386. doi: 10.1097/00007632-200009150-00018. [DOI] [PubMed] [Google Scholar]
- 5.Asher M, Min Lai S, Burton D, et al. The reliability and concurrent validity of the Scoliosis Research Society-22 patient questionnaire for idiopathic scoliosis. Spine. 2003;28:63–69. doi: 10.1097/00007632-200301010-00015. [DOI] [PubMed] [Google Scholar]
- 6.Been HD, Kalkman CJ, Traast HS, Ongerboer de Visser BW. Neurologic injury after insertion of laminar hooks during Cotrel-Dubousset instrumentation. Spine. 1994;19:1402–1405. doi: 10.1097/00007632-199404150-00021. [DOI] [PubMed] [Google Scholar]
- 7.Belmont PJ, Klemme WR, Dhawan A, Polly DW. In vivo accuracy of thoracic pedicle screws. Spine. 2001;26:2340–2346. doi: 10.1097/00007632-200111010-00010. [DOI] [PubMed] [Google Scholar]
- 8.Bradford DS. Vertebral column resection. Orthop Trans. 1987;11:502. [Google Scholar]
- 9.Bradford DS, Tribus CB. Vertebral column resection for the treatment of rigid coronal decompensation. Spine. 1997;22:1590–1599. doi: 10.1097/00007632-199707150-00013. [DOI] [PubMed] [Google Scholar]
- 10.Bullmann V, Halm HFH, Schulte T, Lerner T, Weber TP, Liljenqvist UR. Combined anterior and posterior instrumentation in severe and rigid idiopathic scoliosis. Eur Spine J. 2006;15:440–448. doi: 10.1007/s00586-005-1016-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burton DC, Asher MA, Burke SW, Sama AA, Boachie Adjei O, Huang RC, et al. The treatment of large (>70°) thoracic curves in patients with idiopathic scoliosis with posterior scoliosis instrumentation and arthrodesis: When anterior release is indicated? Abstract presented POSNA meeting. FLA, USA: Amelia Isl Plant; 2003. [Google Scholar]
- 12.Burton DC, Sarna AA, Asher MA, et al. The Treatment of large (>70°) thoracic idiopathic scoliosis curves with posterior instrumentation and arthrodesis: when is anterior release indicated? Spine. 2005;30:1979–1984. doi: 10.1097/01.brs.0000176196.94565.d6. [DOI] [PubMed] [Google Scholar]
- 13.Byrd JA, Scoles PV, Winter RB, Bradford DS, Lonstein JE, Moe JH. Adult idiopathic scoliosis treated by anterior and posterior spinal fusion. J Bone Joint Surg Am. 1987;69:843–850. [PubMed] [Google Scholar]
- 14.Chang KW. Cantiliver bending technique for treatment of large and rigid scoliosis. Spine. 2003;28:2452–2458. doi: 10.1097/01.BRS.0000092063.63315.D5. [DOI] [PubMed] [Google Scholar]
- 15.Choi JB, Han JO, Jeong JW. False aneurysm of the thoracic aorta associated with an aorto-chest wall fistula after spinal instrumentation. J Trauma. 2001;50:140–143. doi: 10.1097/00005373-200101000-00029. [DOI] [PubMed] [Google Scholar]
- 16.Cobb JR. Outline for the study of scoliosis. AAOS Instr Course Lect. 1948;5:261–275. [Google Scholar]
- 17.Delank KS, Delank HW, Konig DP, Popken F, Furderer S, Eysel P. Iatrogenic paraplegia in spinal surgery. Arch Orthop Trauma Surg. 2005;125:33–41. doi: 10.1007/s00402-004-0763-5. [DOI] [PubMed] [Google Scholar]
- 18.Giorgi G, Stella G, Becchetti S, Martucci G, Miscioscia D. Cotrel-Dubousset instrumentation for the treatment of severe scoliosis. Eur Spine J. 1999;8:8–15. doi: 10.1007/s005860050120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Di Silvestre M, Parisini P, Lolli F, Bakaloudis G. Complications of thoracic pedicle screws in scoliosis treatment. Spine. 2007;32:1655–1661. doi: 10.1097/BRS.0b013e318074d604. [DOI] [PubMed] [Google Scholar]
- 20.Dobbs MB, Lenke LG, Kim YJ, Luhmann SJ, Bridwell KH. Anterior/posterior spinal instrumentation versus posterior instrumentation alone for the treatment of adolescent idiopathic scoliotic curves more than 90°. Spine. 2006;31:2386–2391. doi: 10.1097/01.brs.0000238965.81013.c5. [DOI] [PubMed] [Google Scholar]
- 21.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine. 1990;15:11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Harms J. Personal Comunication. 1st International Course. Bologna: New Trends Spinal Surg; 2006. [Google Scholar]
- 23.Kabins MB. Point of view. Spine. 2004;29:342. doi: 10.1097/01.BRS.0000109984.65138.0C. [DOI] [Google Scholar]
- 24.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 25.Kim YJ, Lenke LG, Bridwell KH, Kim KL, Steger-May K. Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure. J Bone Joint Surg Am. 2005;87:1534–1541. doi: 10.2106/JBJS.C.00978. [DOI] [PubMed] [Google Scholar]
- 26.Korovessis P. Combined VDS and Harrington instrumentation for treatment of idiopathic double major curves. Spine. 1987;12:244–250. doi: 10.1097/00007632-198704000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Kuklo TR, Lenke LG, O’Brien MF, Lehman RA, Polly DW, Schroeder BS. Accuracy and efficacy of thoracic pedicle screws in curves more than 90°. Spine. 2005;20:222–226. doi: 10.1097/01.brs.0000150482.26918.d8. [DOI] [PubMed] [Google Scholar]
- 28.Lenke L, Betz R, Harms J, Bridwell KH, Clements DH, Lowe TG, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83:1169–1181. [PubMed] [Google Scholar]
- 29.Lenke LG. Anterior endoscopic discectomy and fusion for adolescent idiopathic scoliosis. Spine. 2003;28:S36–S43. doi: 10.1097/00007632-200308011-00007. [DOI] [PubMed] [Google Scholar]
- 30.Liljienqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 31.Liljenqvist UR, Lepsien U, Hackeberg L, Niemeyer T, Halm H. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J. 2002;11:336–343. doi: 10.1007/s00586-002-0415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liljenqvist UR, Allkemper T, Hackenberg L, Link TM, Steinbeck J, Halm HFH. Analysis of vertebral morphology in idiopathic scoliosis with use of magnetic resonance imaging and multiplanar reconstruction. J Bone Joint Surg Am. 2002;84:359–368. doi: 10.2106/00004623-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M. Thoracic adolescent idiopathic scoliosis curves between 70° and 100°. Is anterior release necessary? Spine. 2005;30:2061–2067. doi: 10.1097/01.brs.0000179299.78791.96. [DOI] [PubMed] [Google Scholar]
- 34.Minor ME, Morrissey NJ, Peress R, Carroccio A, Ellozy S, Agarwal G, et al. Endovascular treatment of an iatrogenic thoracic aortic injury after spinal instrumentation: case report. J Vasc Surg. 2004;39:893–896. doi: 10.1016/j.jvs.2003.10.056. [DOI] [PubMed] [Google Scholar]
- 35.Mulholland RC. Editorial. Pedicle screw fixation in the spine. J Bone Joint Surg. 1994;76:517. [PubMed] [Google Scholar]
- 36.Newton PO, Marks M, Faro F, Betz R, Clements D, Haher T, et al. Use of video-assisted thoracoscopic surgery to reduce perioperative morbidity in scoliosis surgery. Spine. 2003;28:S249–S254. doi: 10.1097/01.BRS.0000092475.04293.F5. [DOI] [PubMed] [Google Scholar]
- 37.Niemeyer T, Freeman BJ, Grevitt MP, Webb JK. Anterior thoracoscopic surgery followed by posterior instrumentation and fusion in spinal deformities. Eur Spine J. 2000;9:499–504. doi: 10.1007/s005860000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.O’Brein M, Kuklo T (2004) Spinal Deformity Study Group. Radiografic Measurement Manual. Ed. Medtronic Sofamor Danek
- 39.Papin P, Arlet V, Marchesi D, Rosenblatt B, Aebi M. Unusual presentation of spinal cord compression related to misplaced pedicle screws in thoracic scoliosis. Eur Spine J. 1999;8:156–160. doi: 10.1007/s005860050147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pellin B, Zielke K. Severe scoliosis in adults and older, adolescents 41 operated cases. Rev Chir Orthop Reparatrice Appar Mot. 1974;60:623–633. [PubMed] [Google Scholar]
- 41.Polly DW, Potter BK, Kuklo T, Young S, Johnson C, Klemme WR. Volumetric spinal canal intrusion: a comparison between thoracic pedicle screws and thoracic hooks. Spine. 2004;29:63–69. doi: 10.1097/01.BRS.0000105525.06564.56. [DOI] [PubMed] [Google Scholar]
- 42.Rinella A, Lenke L, Whitaker C, Kim Y, Park SS, Peelle M, et al. Perioperative halo-gravity traction in the treatment of severe scoliosis and kyphosis. Spine. 2005;30:475–482. doi: 10.1097/01.brs.0000153707.80497.a2. [DOI] [PubMed] [Google Scholar]
- 43.Savini R, Parisini P, Corbascio M, Prosperi L (1977). L’halo trazione associata alla fisio kinesi terapia nel trattamento correttivo delle scoliosi con gravissimi deficit respiratori. C·O.M vol XLIII° fasc. IV:353–360 [PubMed]
- 44.Savini R, Parisini P, et al. The surgical correction of severe vertebral deformities by combined anterior and posterior instrumentation. Prog Spinal Pathol. 1989;4:211–221. [Google Scholar]
- 45.Shen J, Qiu G, Wang Y, Zhang Z, Zhao Y. Comparison of 1-stage versus 2-stage anterior and posterior spinal fusion for severe and rigid idiopathic scoliosis—a randomized prospective study. Spine. 2006;31:2525–2528. doi: 10.1097/01.brs.0000240704.42264.c4. [DOI] [PubMed] [Google Scholar]
- 46.Shufflebarger HL, Grimm JO, Bui V, Thomson JD. Anterior and posterior spinal fusion. Staged versus same-day surgery. Spine. 1991;16:930–933. doi: 10.1097/00007632-199108000-00011. [DOI] [PubMed] [Google Scholar]
- 47.Smythe WR, Carpenter JP. Upper abdominal aortic iniury during spinal surgery. J Vasc Surg. 1997;25:774–777. doi: 10.1016/S0741-5214(97)70310-0. [DOI] [PubMed] [Google Scholar]
- 48.Stokes IAF. Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine. 1994;19:236–248. doi: 10.1097/00007632-199401001-00020. [DOI] [PubMed] [Google Scholar]
- 49.Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994;18:341–346. doi: 10.1007/BF00187077. [DOI] [PubMed] [Google Scholar]
- 50.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. doi: 10.1097/00007632-199506000-00012. [DOI] [PubMed] [Google Scholar]
- 51.Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER. Thoracic pedicle screw fixation in spinal deformities. Are they really safe? Spine. 2001;26:2049–2057. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 52.Suk SI, Lee SM, Chung ER, Kim JH, Kim WJ, Sohn HM. Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis. Spine. 2003;28:484–491. doi: 10.1097/00007632-200303010-00014. [DOI] [PubMed] [Google Scholar]
- 53.Suk SI, Chung ER, Kim JH, Kim SS, Lee JS, Choi WK. Posterior vertebral column resection for severe rigid scoliosis. Spine. 2005;30:1682–1687. doi: 10.1097/01.brs.0000170590.21071.c1. [DOI] [PubMed] [Google Scholar]
- 54.Tokunaga M, Minani S, Kitahara H, Isobe K, Nakata Y, Moriya H. Vertebral decancellation for severe scoliosis. Spine. 2000;25:469–474. doi: 10.1097/00007632-200002150-00013. [DOI] [PubMed] [Google Scholar]
- 55.Vaccaro AR, Rizzolo SJ, Allardyce TJ, Ramsey M, Salvo J, Balderston RA, et al. Placement of pedicle screws in the thoracic spine. Part I: morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77:1193–1199. doi: 10.2106/00004623-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 56.Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, et al. Placement of pedicle screws in the thoracic spine: Part II: an anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200–1206. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 57.Vaughan JJ, Winter RB, Lonstein JE. Comparison of the use of supine bending and traction radiographs in the selection of the fusion area in adolescent idiopathic scoliosis. Spine. 1996;21:2469–2473. doi: 10.1097/00007632-199611010-00012. [DOI] [PubMed] [Google Scholar]
- 58.Wilber RG, Thompson GH, Shaffer JW, Brown RH, Nash CL., Jr Postoperative neurological deficits in segmental spinal instrumentation. A study using spinal cord monitoring. J Bone Joint Surg Am. 1984;66:1178–1187. [PubMed] [Google Scholar]
- 59.Xu R, Ebraheim NA, Ou Y, Yeasting RA. Anatomic consideration of pedicle screw placement in the thoracic spine. Roy-Camille technique versus Open-Lamina tecnique. Spine. 1998;23:1065–1068. doi: 10.1097/00007632-199805010-00021. [DOI] [PubMed] [Google Scholar]