Abstract
Objective
To evaluate functional outcome after hemiarthroplasty for displaced proximal humeral fractures and to review whether prosthesis type, intraoperative technique or previous ipsilateral shoulder surgery could affect the outcome.
Methods
We reviewed the medical records and radiographs of patients who had undergone hemiarthroplasty for proximal humeral fractures between 1992 and 2000. We identified 45 patients, 39 with acute fractures and 6 with fracture-related complications. One surgeon performed 17 surgeries (38%), and the rest were carried out by 11 other orthopedic surgeons. Using the American Shoulder and Elbow Surgeons Evaluation Form and the Western Ontario Rotator Cuff Index, we evaluated patients who had been followed for at least 2 years for residual shoulder pain, range of motion, strength, stability and function. The senior authors reviewed the radiographs.
Results
The mean age of the patients at presentation was 70 (range 46–95) years. The mean active forward elevation was 87°, abduction 63° and external rotation 22°; the mean internal rotation was to the L2 vertebra. Of the patients, 15% reported severe pain, and 25% were unable to sleep on the affected side. Patients with previous surgeries and those with intraoperative cuff tears were found to have more postoperative pain.
Conclusion
We conclude that soft tissue status and operative technique play an important role in late postoperative pain and range of motion. Hemiarthroplasty after failed open reduction and internal fixation is associated with inferior results. We were unable to show a difference in long-term outcome related to the prosthesis type.
Abstract
Objectif
Évaluer le résultat fonctionnel après une hémiarthroplastie à la suite d'une fracture de la partie proximale de l'humérus avec déplacement et déterminer si le type de prothèse, la technique intraopératoire ou une chirurgie ipsilatérale antérieure de l'épaule pourrait avoir un effet sur le résultat.
Méthodes
Nous avons examiné les dossiers médicaux et les radiographies de patients qui avaient subi une hémiarthroplastie à la suite d'une fracture de la partie proximale de l'humérus entre 1992 et 2000. Nous avons trouvé 45 patients, dont 39 avaient subi une fracture aiguë et 6 avaient eu des complications liées à la fracture. Un chirurgien a pratiqué 17 interventions (38 %) et les autres ont été exécutées par 11 autres chirurgiens orthopédistes. À l'aide du formulaire américain d'évaluation des chirurgies de l'épaule et du coude et de l'indice de la coiffe des rotateurs de l'ouest de l'Ontario, nous avons évalué des patients qu'on avait suivis pendant au moins 2 ans pour déterminer la douleur résiduelle à l'épaule, l'amplitude du mouvement, la force, la stabilité et la fonction. Les auteurs principaux ont étudié les radiographies.
Résultats
Les patients avaient en moyenne 70 ans (intervalle de 46 à 95 ans) lorsqu'ils se sont présentés. L'élévation avant active moyenne était de 87°, l'abduction de 63° et la rotation externe de 22°. La rotation interne moyenne atteignait le niveau de la vertèbre L2. Parmi les patients, 15 % ont signalé une douleur sévère et 25 % ne pouvaient dormir sur le côté touché. Les patients qui avaient subi une intervention chirurgicale antérieure et ceux qui avaient subi un déchirement de la coiffe pendant l'intervention avaient le plus de douleurs postopératoires.
Conclusion
Nous concluons que l'état des tissus mous et la technique opératoire jouent un rôle important dans la douleur postopératoire tardive et l'amplitude du mouvement. L'hémiarthroplastie après une réduction ouverte et une fixation interne échouées est associée à des résultats inférieurs. Nous n'avons pu montrer de différence au niveau des résultats à long terme en ce qui a trait au type de prothèse.
The management of comminuted and displaced proximal humeral fractures continues to be challenging. Often, poor bone quality and injured or degenerative soft tissues in elderly patients render stable fracture fixation and musculotendinous soft tissue repair difficult to achieve. Neer1,2 has shown that overall results that are good to excellent can be consistently obtained. However, other authors have reported less satisfactory or even disappointing results, including stiff and painful shoulders.3–10
The purpose of this retrospective review was to evaluate functional outcome in patients who had undergone hemiarthroplasty for proximal humeral fractures in an academic orthopedic inpatient service.
Methods
We retrospectively reviewed all consecutive cases of patients who underwent hemiarthroplasty for displaced proximal humeral fractures at the General Campus of the Ottawa Hospital in the period between 1992 and 2000. We evaluated their medical records, surgical notes and outpatient records. The senior authors (J.B. and G.F.D.) assessed the patients' pre-and postoperative radiographs. We excluded patients who had been followed for less than 2 years.
We attempted to contact all identified patients for follow-up to evaluate their residual pain levels and functional ability. In addition, they were examined for active and passive range of motion and strength. Standardized anteroposterior, transscapular lateral and axillary views were obtained for all patients. The 2 senior authors, who were blinded to the identity and treatment of the patients, assessed prosthetic loosening, migration, subsidence, tuberosity detachment, glenoid erosion and heterotopic bone formation. The age and sex of the patients, the presence of previous shoulder surgery, the interval to surgery from the time of injury and intraoperative variables (cementing, type of prosthesis, method of attaching the tuberosities and the presence of rotator cuff tear) were recorded as potential variables of importance. The patients whose hemiarthroplasty was performed by a single surgeon were compared with the rest of the patients.
With the help of the research coordinators (A.F.C. and H.H.) and to assess further objective outcomes at the time of follow-up, every patient completed the validated American Shoulder and Elbow Surgeons Evaluation (ASES) form and the Western Ontario Rotator Cuff Index (WORC). The ASES is a health care provider questionnaire that includes 5 domains: pain, motion, strength, stability and function. The maximum score is 100 and is based on the sum of scores for each domain except motion, which is reported separately in degrees. The WORC is a self-report questionnaire that is designed to measure health-related quality of life in people with injures and conditions of the shoulder rotator cuff. It includes 21 questions in 5 domains: pain and physical function, sports and recreation, work, lifestyle and emotions. The respondents answer on a visual analogue scale with anchors ranging from no pain/difficulty to extreme pain/difficulty.11
Because of the small sample size relative to the large number of variables of interest, the nonparametric Kruskal–Wallis and Mann–Whitney U tests were computed to determine which pre-and intraoperative variables influenced functional outcome. Statistical significance was set at p < 0.05.
Results
Of 56 patients who underwent hemiarthroplasty for proximal humeral fractures or fracture-related complications, 45 (33 women, 12 men) were available for review according to the aforementioned criteria (4 were deceased, 3 refused to come back for the assessment, and 4 could not be contacted).
The patients' mean age at the time of presentation was 63.0 (standard deviation [SD] 11.8) years for men and 72.8 (SD 12.3) years for women (p = 0.017). The mean time to follow-up was 48 (range 24–123) months. Before their hemiarthroplasty, 6 patients had undergone a previous open reduction and internal fixation (ORIF) of their fractures. As classified by Neer,12 there were three 2-part fractures (2 of which were displaced subcapital fractures, and 1 of which was a 2-part surgical neck fracture nonunion), fourteen 3-part fractures, seventeen 4-part fractures, 7 fracture dislocations and 4 head split fractures (Table 1). The indications for hemiarthroplasty in the group with a previous ORIF were loss of reduction (2), avascular necrosis (2), nonunion (1) and malunion (1). Thirty-nine patients had their surgeries within 3 weeks of injury, and 6 underwent surgery more than 3 weeks after injury. Of the 45 patients, 17 (38%) were operated on by a dedicated shoulder surgeon, whereas the remaining 28 (62%) were distributed among 11 different orthopedic surgeons. A deltopectoral approach was used in all cases. The Neer monobloc prosthesis (Smith & Nephew) was used in 18 patients (40%) and the Global modular prosthesis (DePuy Orthopaedics) in 27 (60%). Of the prostheses, 35 (78%) were cemented. Sutures were used to reattach the tuberosities in 37 patients (82%), and wires were used in 8 (18%). In 29 shoulders (64%), a tear in the rotator cuff tissue was reported and repaired at the time of the replacement. One patient had a brachial plexus injury that was missed preoperatively.
Table 1
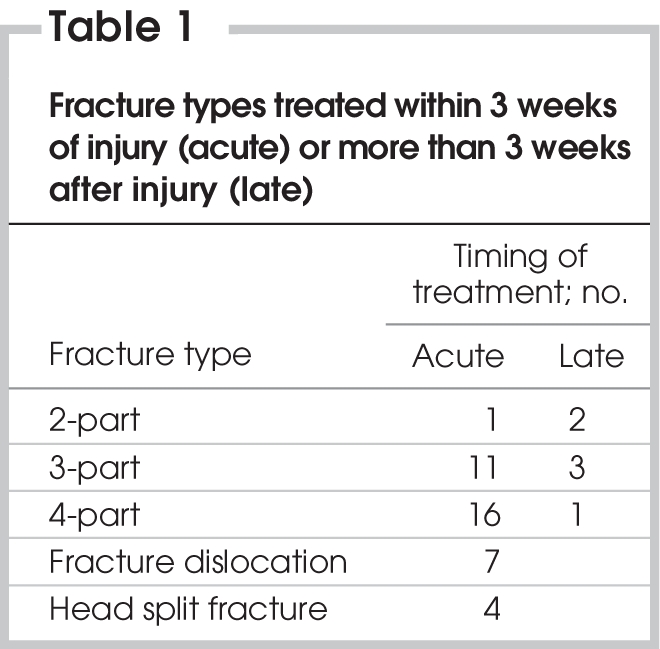
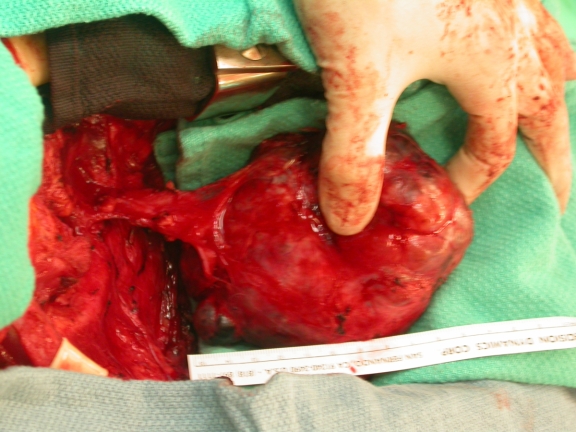
Patients were evaluated with the ASES form and the WORC. Average active forward elevation was 87° (range 15°– 160°), active abduction 63° (range 10°– 120°), active external rotation 22° (range –15° to 120°); active internal rotation was between L1 and L3. The mean WORC score was 63.3% (range 17%–97%). Pain severity at follow-up is depicted in Figure 1. The presence of heterotopic bone formation was not associated with decreased range of motion (ROM). No difference in the amount of loosening and subsidence was found between the cemented and uncemented prostheses (Fig. 2).
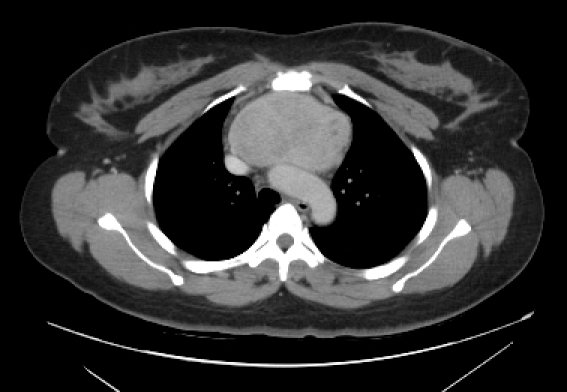
FIG. 1. Pain severity at final follow-up in primary versus secondary hemiarthroplasty.
FIG. 2. Radiographic image of the shoulder of a 73-year-old man with poor outcome after hemiarthroplasty for 4-part fracture.
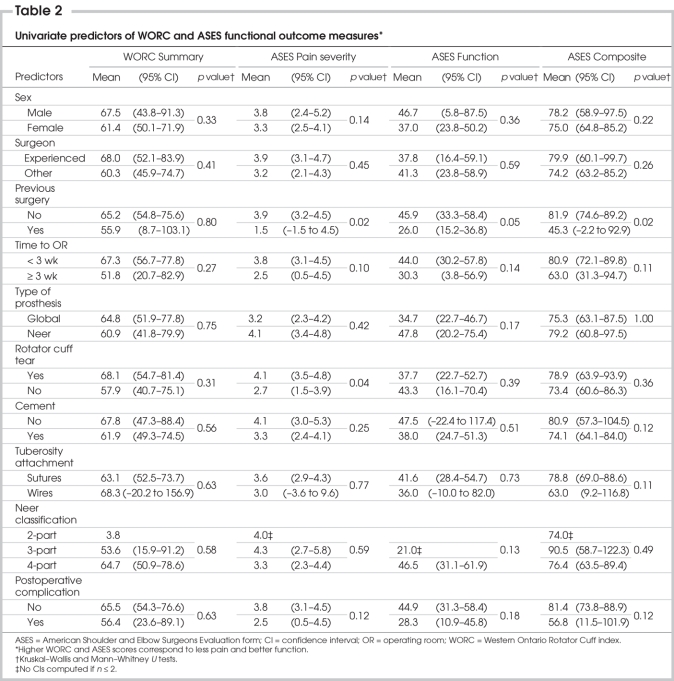
Table 2 demonstrates the univariate relations between several predictor variables and ASES and WORC outcomes. There were some interesting findings. Complexity of fracture pattern, age, time to the operating room, type of prosthesis and tuberosity attachment were not related to functional outcome.
Table 2
Patients who had previous ORIF of their fractures were found to have more pain (p = 0.022) and had less function as measured by the functional and composite scores on the ASES (p = 0.052 and 0.017, respectively), compared with those who had a primary hemiarthroplasty for their fractures. Patients who had a rotator cuff tear that was repaired intraoperatively were found to have more postoperative pain (p = 0.042) than those with no tear. Although not statistically significant, they also reported lower scores on the WORC functional outcome measure. A comparison of the group of patients treated by the surgeon who had special expertise in shoulder surgery and the remainder of the patients showed that patients in the first group trended toward a better range of motion, less pain and higher functional outcome WORC scores. There was also a trend for patients with an uncemented prosthesis to function better than those with cement.
Several complications resulted: 2 superficial wound infections, 3 proximally migrated prostheses, 1 intraoperative fracture distal to the prosthesis, 4 late detachments of the tuberosities and 1 excessive heterotopic ossification equivalent to Brooker type III. One patient sustained a myocardial infarction 2 days after surgery. The complications did not adversely affect outcome scores.
Discussion
Proximal humeral fractures represent 5%–7% of all fractures and 40% of all humeral fractures. In the elderly, they represent up to 76% of humeral fractures. Several published articles have suggested different treatment methods.8,13–15 Recently, satisfactory results in 85% of the procedures have been reported after open reduction and internal fixation of proximal humeral fractures.16 With more than 90% of outcomes being satisfactory, Neer1,2 reported outstanding results with respect to range of motion and pain relief. Other studies, however, have reported poor or less-than-optimal results with hemiarthoplasty for proximal humeral fractures.3–10 Further, some studies have reported comparable results with conservatively treated 3-part fractures.17,18
Virtually all published studies on hemiarthroplasty for proximal humeral fractures included series with small numbers of patients and short follow-up periods. For this reason, among others, we believe it is important to report our results wherein 45 patients had a mean follow-up of 48 months. Of our patients, 64% had no pain, or only mild pain; only 3 patients (12%) reported severe pain. The presence of a complete rotator tear at the time of hemiarthroplasty was found to be associated with more severe postoperative pain. Because of our study design, we are unable to determine whether these tears were present before the injury; although they may assist the operative exposure, the quality of the cuff tissue itself possibly contributed to the inferior results. The range of motion in our patients was not as good as that reported by other authors17,19 and might reflect variations in postoperative rehabilitation after transfer to small community hospitals only a few days postsurgery. Despite the presence of some factors that could adversely affect the final outcome (previous ORIF and delay in surgery), the group of patients treated by an experienced shoulder surgeon trended toward a better range of motion, less pain and a better WORC score, compared with the rest of the patients. Despite the lack of statistical significance, this observation suggests that surgeon experience positively influences outcome.
Few studies highlight the importance of tuberosity healing and position on functional outcome,20–22 and more tuberosity nonunion was noted in centres where hemiarthroplasty for proximal humeral fractures is performed less frequently.22 We reported a 14% incidence of definite tuberosity detachment or migration, which might be a factor in the less-than-optimal functional outcomes we observed in this cohort.
Overall, we found that patients who had uncemented hemiarthroplasty had less pain and better overall function. The treating surgeon decided whether to perform cemented as opposed to uncemented hemiarthoplasty, and the decision was based on the quality of bone and the intraoperative stability of trial components. In other words, uncemented hemiarthoplasty was performed on patients with higher bone quality and adequate soft tissue, which could potentially explain the better results they enjoyed. Our patient population had good pain relief and moderate functional improvement similar to that reported by Anjum.23 Nevertheless, these results seem inferior to those reported for cohorts with primary elective arthroplasty for arthritis.24,25
Conclusion
This retrospective review reports the collective experience of a large number of academic surgeons with different levels of experience in shoulder surgery working in a trauma centre and treating displaced proximal humeral fractures. Our careful review of patients illustrates that the outcome of hemiarthroplasty for proximal humeral fractures is not as good as previously reported with first-and second-generation implants. It would appear that the availability of an experienced surgeon positively influences the final outcome of these difficult injuries. Our results can serve as a benchmark against which newer modular designs, which may allow more anatomic tuberosity positioning and better offset, can be compared with this historical cohort.
Presented at the Canadian Orthopedic Association Annual Meeting, Calgary, Alta., June 17–20, 2004.
Contributors: Drs. Fallatah, Dervin and Brunet designed the study. Dr. Fallatah and Mses. Conway and Hrushowy acquired the data, which Drs. Fallatah, Dervin, Brunet and Ms. Conway analyzed. Drs. Fallatah and Dervin wrote and reviewed the article; Dr. Brunet, Ms. Conway and Ms. Hrushowy also reviewed it. All authors gave final approval for publication.
Competing interests: None declared.
Accepted for publication Sept. 14, 2007
Correspondence to: Dr. G.F. Dervin, The Ottawa Hospital—General Campus, Critical Care Wing, Rm. 1640, Box 502, 501 Smyth Rd., Ottawa ON K1H 8L6; fax 613 737-8837; gdervin@ottawahospital.on.ca
References
- 1.Neer CS II. Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am 1970;52:1090-103. [PubMed]
- 2.Neer CS II, Mcllveen SJ. Recent results and technique of prosthetic replacement for four-part proximal humeral fractures. Orthop Trans 1986;10:475.
- 3.Dimakopoulos P, Potamitis N, Lambiris E. Hemiarthroplasty in the treatment of comminuted intraarticular fractures of the proximal humerus. Clin Orthop Relat Res 1997;341:7-11. [PubMed]
- 4.Goldman RT, Koval KJ, Cuomo F, et al. Functional outcome after humeral head replacement for acute three-and four-part proximal fractures. J Shoulder Elbow Surg 1995;4:81-6. [DOI] [PubMed]
- 5.Green A, Barnard WL, Imbird RS, et al. Humeral head replacement for acute four-part proximal humerus fractures. J Shoulder Elbow Surg 1993;2:249-54. [DOI] [PubMed]
- 6.Hawkins RJ, Switlyk P. Acute prosthetic replacement for severe fractures of the proximal humerus. Clin Orthop Relat Res 1993;289:156-60. [PubMed]
- 7.Kraulis J, Hunter G. The results of prosthetic replacement in fracture-dislocations of the upper end of the humerus. Injury 1976;8:129-31. [DOI] [PubMed]
- 8.Stableforth PG. Four-part fractures of the neck of the humerus. J Bone Joint Surg Br 1984; 66:104-8. [DOI] [PubMed]
- 9.Tanner MW, Cofield RH. Prosthetic arthoplasty for fractures and fracture dislocations of the proximal humerus. Clin Orthop Relat Res 1983;179:116-28. [PubMed]
- 10.Willems WJ, Lim TEA. Neer arthroplasty for humeral fractures. Acta Orthop Scand 1985;56:394-5. [DOI] [PubMed]
- 11.Kirkley A, Alvarez C, Griffin S. The development and evaluation of a disease specific quality-of-life questionnaire for disorders of the rotator cuff. The Western Ontario Rotator Cuff Index. Clin J Sport Med 2003;13:84-92. [DOI] [PubMed]
- 12.Neer CS II. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 1970;52:1077-89. [PubMed]
- 13.Cofield RH. Comminuted fractures of the proximal humerus. Clin Orthop Relat Res 1988;230:49-57. [PubMed]
- 14.Jakob RP, Miniaci A, Anson PS, et al. Four-part valgus impacted fractures of the proximal humerus. J Bone Joint Surg Br 1991;73:295-8. [DOI] [PubMed]
- 15.Moda SK, Chadha NS, Sangwan SS, et al. Open reduction and fixation of proximal humeral fractures and fractures dislocations. J Bone Joint Surg Br 1990;72:1050-2. [DOI] [PubMed]
- 16.Wijgman AJ, Roolker W, Patt TW, et al. Open reduction and internal fixation of three-and four-part fractures of the proximal humerus. J Bone Joint Surg Am 2002;84:1919-25. [PubMed]
- 17.Zyto K, Kronberg M, Brostrom LA. Shoulder function after displaced fractures of the proximal humerus. J Shoulder Elbow Surg 1995;4:331-6. [DOI] [PubMed]
- 18.Schai P, Imhoff A, Preiss S. Comminuted humeral head fractures: a multicenter analysis. J Shoulder Elbow Surg 1995;4:319-30. [DOI] [PubMed]
- 19.Zyto K, Wallace A, Frostick SP, et al. Outcome after hemiarthroplasty for three-and four-part fractures of the proximal humerus. J Shoulder Elbow Surg 1998;7: 85-9. [DOI] [PubMed]
- 20.Loew M, Heitkemper S, Parsch D, et al. Influence of the design of the prosthesis on the outcome after hemiarthroplasty of the shoulder in displaced fractures of the head of the humerus. J Bone Joint Surg Br 2006;88:345-50. [DOI] [PubMed]
- 21.Demirhan M, Kilicoglu O, Altinel L, et al. Prognostic factors in prosthetic replacement for acute proximal humerus fractures. J Orthop Trauma 2003;17:181-8. [DOI] [PubMed]
- 22.Kralinger F, Schwaiger R, Wambacher M, et al. Outcome after primary hemiarthroplasty for fracture of the head of the humerus. A retrospective multicenter study of 167 patients. J Bone Joint Surg Br 2004;86:217-9. [DOI] [PubMed]
- 23.Anjum SN, Butt MS. Treatment of comminuted proximal humerus fractures with shoulder hemiarthroplasty in elderly patients. Acta Orthop Belg 2005;71:388-95. [PubMed]
- 24.Krepler P, Wanivenhaus A, Wurnig C. Outcome assessment of hemiarthroplasty of the shoulder: a 5-year follow-up with 4 evaluation tools. Acta Orthop 2006;77:778-84. [DOI] [PubMed]
- 25.Lo IK, Litchfield RB, Griffin S, et al. Quality-of-life outcome following hemiarthroplasty or total shoulder artrhroplasty in patients with osteoarthritis: a prospective randomized trial. J Bone Joint Surg Am 2005;87:2178-85. [DOI] [PubMed]